Abstract
Purpose
To investigate the potential usage of biological delivery membranes containing mitomycin C (MMC) or 5-fluorouracil (5-FU) in the construction of glaucoma-filtering blebs, and to evaluate their safety and efficacy.
Methods
Chitosan was selected as the biological membrane carrier to prepare sustained-released membranes. Twelve micrograms of 5-FU or MMC was covalently conjugated onto the membranes by solvent volatilization. Rabbits underwent glaucoma filtration surgery and were randomly allocated into one of the four treatment regimens: glaucoma filtration operation with no implantation of chitosan membrane group (as control), drug-free chitosan membrane implantation group (blank/placebo group), membrane containing 5-FU treatment group (5-FU group), and membrane containing MMC treatment group (MMC group). Each group consisted of 12 rabbits. Intraocular pressure (IOP) was measured and evaluated over a 28-day period follow-up preoperatively, then after surgery on days 1, 3, 5, 7, 14, 21, and 28 by Tono-Pen. The aqueous humor was analyzed in each experimental and control groups at days 4, 6, 8, 10, 12, 14, 16, and 20 after operation. Bleb survival and anterior segment were examined with a slit lamp microscope and photographed simultaneously. Two rabbits from each group were killed on day 28 and eight eye samples obtained for histopathological study. Corneas and lenses were examined by transmission and scanning electron microscopy.
Results
Both 5-FU and MMC significantly prolonged bleb survival compared with control groups. The filtering bleb’s survival period was significantly more prolonged in the MMC and 5-FU groups (maintained 14 days) than the other two groups (maintained 7 days). Significantly lower IOP was observed within the control, blank, and 5-FU groups after surgery on day 14 compared with that before operation, with F-values of 6.567, 11.426, and 13.467, respectively (P < 0.01). The most significant lower IOP was recorded in the MMC group on day 28 postoperation (F-value 26.866, P < 0.01). No obvious abnormalities were found in cornea or anterior lens capsule 28 days after surgery.
Conclusion
The study provided evidence that 5-FU and MMC biological delivery membranes could significantly improve the outcome of filtering procedures, the survival of the bleb, and maintenance of lower IOP. MMC membrane is superior to 5-FU, with regard to the more effective reduction of IOP. The results indicated a safe and effective treatment strategy in glaucoma surgery.
Introduction
Glaucoma filtration surgery is one of the most common surgeries for glaucoma; it helps the eye drain aqueous humor more effectively and reduces intraocular pressure (IOP), especially for patients who respond poorly to conventional medications. However, the failure rate of the first surgery is up to 25% for patients above 40 years old, and more significantly, 40%–60% for people younger than 40 years old.Citation1–Citation3 The most prevalent reason for the failure is always attributed to the proliferation of fibroblasts and formation of scars, which block the filtration pathway. 5-Fluorouracil (5-FU) and mitomycin C (MMC) are antimetabolites that could improve the success rate of glaucoma filtration surgeries, preventing scar formation by inhibition of fibroblast outgrowth in conjunctiva.Citation4 However, there are concerns about the clinical application of these medicines, such as cornea and conjunctiva epithelial ulceration, conjunctiva wound leakage, toxicity to ciliary epithelium and cornea endothelium, persistent chronic low IOP, and other severe complications like endophthalmitis and scleritis.Citation5 Therefore, it is recommended that the lowest effective dosage of antiproliferation drugs be used locally instead of systemically, in order to reduce damage to adjacent tissues. We hypothesize that application of biological delivery membranes in the operation of glaucoma filtration not only provides sustained, lowest effective dosage of antimetabolites locally but also significantly decreases the risk of side effects.Citation6 In this study, we utilized chitosan polysaccharide, a nontoxic, completely biodegradable natural polymer, as carrier, which was conjugated with 5-FU or MMC, to prepare a biological membrane, and investigated the effects of 5-FU and MMC-sustained biological delivery membranes on the conjunctiva and sclera wound-healing process following glaucoma surgery in rabbit eyes.
Materials and methods
Animals
A total of 48 healthy New Zealand albino rabbits of age 12–14 weeks were used in this study, with body weight of 3.0–3.5 kg. All were purchased from and authorized by the animal facility of Capital Medical University (Beijing, People’s Republic of China).
Key reagents
Sumianxin II injection was purchased from the Veterinary Institute of Changchun University (Changchun, People’s Republic of China). Sodium pentobarbital was purchased from Beijing Chemical Reagent Company (Beijing, People’s Republic of China).
Creation of biological delivery system
The biological delivery membrane was developed by the Drug Delivery Institute of the Ocean University of China. For rabbit surgery, the membrane was cut into an inverted trapezoid with upper length of 3 mm, bottom length of 2 mm, and height 3 mm. A 1 × 1 mm notch was made in the middle of the upper bottom of the membrane.
Instruments and equipment
A disposable intravenous catheter was used as a drainage tube for postoperative follow-up examinations (24 Ga × 0.75 in; Becton Dickinson Medical Devices, Suzhou, People’s Republic of China). Island body fluid-phase chromatography (Prominence LC-20A; Shimadzu, Kyoto, Japan) was used for 5-FU and MMC concentration determination. A tonometer (Tono-Pen XL, Medtronic, Minneapolis, MN, USA) was used for IOP measurement pre- and postoperation.
Animal models and filtration surgery protocol
After 0.1 mL/kg intramuscular Sumianxin II injection, 3% sodium pentobarbital was administered 1 mL/kg intravenously as general anesthesia for the rabbits. Proparacaine 0.5% eye drops were used for local anesthesia, with 0.25% chloramphenicol eye drops for cleanup of Tenon’s capsule, followed by routine sterilization procedure. Operation procedure: (1) limbus-based flap of the conjunctiva was made at a distance of 5 mm from the limbus in the superior quadrant of the eye; (2) a half-thickness, rectangular, 4 × 3 mm scleral flap was created; (3) at the limbus of cornea, under the sclera flap, a disposable venous indwelling needle (referred to as the drainage tube) perforated into the anterior chamber around 5 mm, parallel to the iris and across the pupillary margin. Pull the needle out and leave indwelling cannula in situ, remove the rest at 1.5–2 mm away from the cornea limbus, and the indwelling part is fixed in the sclera bed by using 10-0 sutures; (4) chitosan membrane was sutured onto the sclera above the flap with 10-0 nylon thread at two cross corners; (5) the sclera flap was closed with 10-0 nylon sutures. The conjunctiva was closed with a continuous locking suture with 8-0 vicryl thread. After the surgery, Tobradex® (Alcon, Hünenberg, Switzerland) eye ointment was applied to the conjunctiva sac. Postoperative treatment included tobramycin eye drops (twice daily) for a week. All operations and treatments were implemented by experienced ophthalmologists.
Experimental groups
Forty-eight rabbits were randomly divided into four groups, as follows: group A, drainage tube implantation only, twelve rabbits, as control; group B, drainage tube implantation plus blank biological delivery membrane implantation, twelve rabbits, as blank/placebo group; group C, drainage tube implantation plus 5-FU biological delivery membrane implantation, twelve rabbits, as 5-FU group; group D, drainage tube implantation plus MMC biological delivery membrane implantation, twelve rabbits, as MMC group.
Slit-lamp observation
A slit-lamp microscope was used to observe the inflammation condition of operated rabbits’ eyes. Anterior chamber, wound healing, and the bleb situation were examined, recorded, and photographed at days 1, 3, 5, 7, 14, 21, and 28 after operation. Bleb survival was the main outcome measured and was defined as the presence of an elevated subconjunctival fluid pocket at the surgical site during slit-lamp exam. The condition of the bleb was recorded according to .Citation14
Table 1 Filtration bleb-grading standard
IOP measurement
IOP of glaucoma filtration-operated rabbits was measured under local anesthesia on the same day as slit-lamp observation. All IOP measurement was performed by one person each time.
Measurement of drug concentration in aqueous humor
Aqueous humor (0.1 mL) was acquired from six eyes each from the experimental and control groups at days 4, 6, 8, 10, 12, 14, 16, and 20 after operation.
5-FU concentration determination
Island body fluid-phase chromatography was used for 5-FU concentration determination. The system included an AT-130L incubator, an SPD-20A ultraviolet (UV) detector, a CBM-20Alite controller, an LC-20AT high-pressure pump, and an SIL-20A automatic sample injector. Chromatography settings were as follows: Shiseido (Tokyo, Japan) MG C18 reverse-phase chromatography column (4.6 × 250 mm, 5 μm); mobile phase methanol:water 82:18; flow rate 0.8 mL/minute; UV detection at 294 nm; column temperature 35°C; sampling volume 50 μL; standard concentration 102 μg/mL.
Aqueous humor (200 μL) from each rabbit eye was mixed with methylene chloride; an organic layer was obtained after centrifugation. It was then mixed with 100 μL mobile phase and vortexed, and 50 μL was subjected to fluid-phase chromatography. The concentration of each sample was induced from corresponding peak areas and a standard regression curve.
MMC concentration determination
Island body fluid-phase chromatography was used for MMC concentration determination; the system included an AT-130L incubator, an SPD-20A UV detector, a CBM-20Alite controller, an LC-20AT high-pressure pump, and an SIL-20A automatic sample injector. Chromatography settings were as follows: Shiseido-MG C18 reverse-phase chromatography column (4.6 mm × 250 mm, 5 μm); mobile phase methanol: water 25:75; flow rate 0.8 mL/minute; UV detection at 365 nm; column temperature 30°C; sampling volume 20 μL; standard concentration 2.16 μg/mL.
Aqueous humor was mixed well with 3.2 mL ethyl acetate and left to rest for 2–3 hours. Following centrifugation at 3000 rpm, the pellets were removed and the supernatants saved for the subsequent test. The supernatants were incubated in a vacuum-evaporating incubator (ZK-82A; Farui, Shanghai, People’s Republic of China) for a few hours at 40°C. Phosphate-buffered saline:methanol (7:3, 0.1 mL) was added to resuspend the supernatants, filtered, and 20 μL resuspended samples subjected to fluid-phase chromatography, with readout at OD 365 nm (μg/g−1 or μg/mL−1).
Histopathological analysis
The rabbits were sacrificed under general anesthesia. Eyeballs were removed with conjunctiva and fixed by 10% formalin, embedded with paraffin, then sectioned, and stained with hematoxylin and eosin. The metabolic absorption of biological delivery membrane implants, their surrounding tissues, and subconjunctival filtration conditions were observed under microscopy with 5 × objective lens magnification and recorded with photography at 5 × and 10 × objective lens magnification.
Electron microscope transmission scanning
One rabbit for each group was killed at day 28 after operation. The corneal endothelium and anterior lens capsule were scanned by electron microscope and compared with normal cornea.
Statistical analysis
SPSS 13.0 statistical software (IBM, Armonk, NY, USA) was utilized in the current study, and data presented and described as means ± standard deviation. One-way analysis of variance was used for single-factor analysis, and P < 0.01 bilaterally was considered statistically significant.
Results
Slit-lamp observation
The bleb was formed in all groups on the first day after operation, and congestive conjunctiva was observed on day 7 after operation. No shallow anterior chamber formed, and no corneal edema was found in any group. There was a small amount of secretion in the anterior chamber. Mild edema in iris and a few secretions at the operation site were observed. All above signs disappeared 1 week after operation.
Conjunctiva bleb
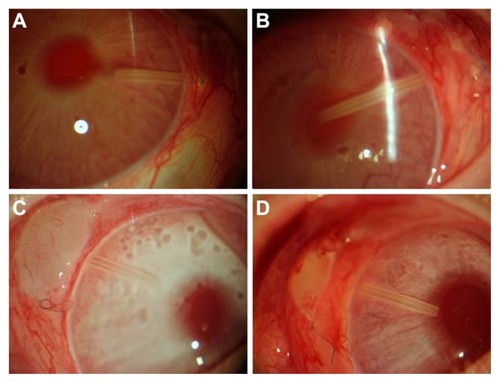
Conjunctiva bleb was obviously formed in all groups within 3 days after operation, and no significant difference was observed. The survival period of the bleb in the MMC group was significantly prolonged compared with the other three groups (P < 0.01); 35% of blebs had disappeared at day 10 after operation. The ranking of the other three groups in terms of the bleb-survival period was 5-FU group > control group > placebo group (). Slit-lamp photography from each group is shown in .
Figure 1 Bleb survival curve.
Abbreviations: MMC, mitomycin C; 5-FU, 5-fluorouracil.
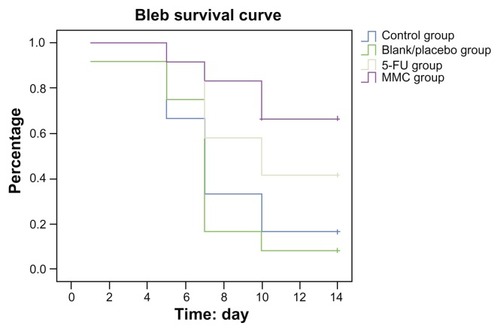
Figure 2 (A–D) Blebs were observed at day 7 after operation under slit-lamp microscope. (A) Control group: blebs disappeared 7 days after operation (16×). (B) Blank/placebo group: blebs disappeared 7 days after operation (16×). (C) MMC group: blebs survived 7 days after operation (16×), less angiogenesis, thinner vessels, lighter color. (D) 5-FU group: blebs shrank, showing the feature of vascular congestion (16×).
Postoperative IOP changes
The IOP comparative data from each group are shown in . Changes in postoperative IOP were quite different among the four groups, though all demonstrated a significant decrease compared to preoperation. A significant decrease in IOPs occurred immediately after operation and lasted to day 28 postoperation in the MMC group (F = 26.866, P < 0.01), whereas IOPs reached their lowest level on day 3 and achieved a general equilibrium point at day 14 postoperation in both the 5-FU (F = 13.467, P < 0.01) and control (F = 6.567, P < 0.01) groups. In the blank/placebo group, IOPs began to increase at day 3 after operation and reached preoperation level at day 7 (F = 11.426, P < 0.01). Intergroup comparisons showed that the MMC group had the longest sustained IOP-decrease period, followed by the 5-FU and control groups. The 5-FU group was superior to the control group, especially at days 15–21 after operation in terms of lower IOP (P < 0.05).
Table 2 Intraocular pressure (IOP) from preoperative and postoperative groups
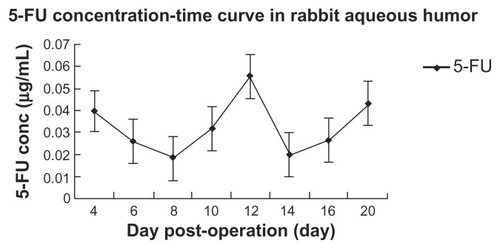
Concentration of 5-FU and MMC in aqueous humor
5-FU from 5-FU biological delivery membrane was detected in aqueous humor from day 20 after operation, and the concentration varied between 0.01885 and 0.04297 μg/mL. The concentration–time curve is shown in . MMC from MMC biological delivery membrane was not detected in aqueous humor till the last day of the experiment.
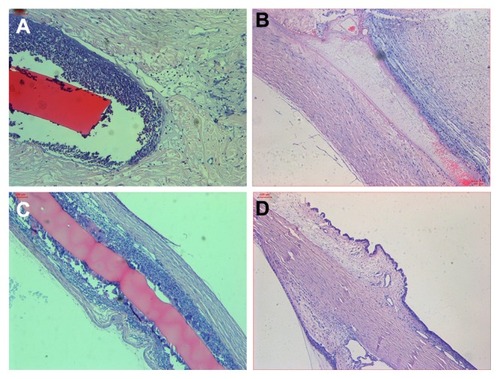
Histopathological analysis of conjunctival bleb
Histopathological studies were performed at day 28 after operation and are shown in . Conjunctiva epithelium was intact in each group after operation. MMC sustained membranes partially degraded, but there were seldom infiltrated inflammatory cells seen in the subconjunctival sclera filtration area. On the contrary, the 5-FU sustained and blank membranes did not degrade at all; however, there was mild to severe infiltration of inflammatory cells. In the control group, the sclera and conjunctiva completely recovered to the original anatomical structure. Most surprising was that in the blank/placebo group, massive inflammation was observed: there were large amounts of infiltrated cells accumulated in the subconjunctival sclera filtration area, resulting in a disappearance of the subconjunctival space.
Figure 4 (A–D) Pathological slides at day 28 after operation. (A) 5-Fluorouracil group: chitosan membrane well tolerated without degradation, inflammatory cells filtrated into the gap between membrane and surrounding sclera tissue (× 5). (B) Mitomycin C group: chitosan membrane partially degraded, few inflammatory cells filtrated (× 5). (C) Blank/placebo group: no degradation of chitosan membrane, surrounded by inflammatory cells filtrated into the gap between membrane and surrounding sclera tissue (× 5). (D) Control group: sclera and conjunctiva recovered to normal (× 5).
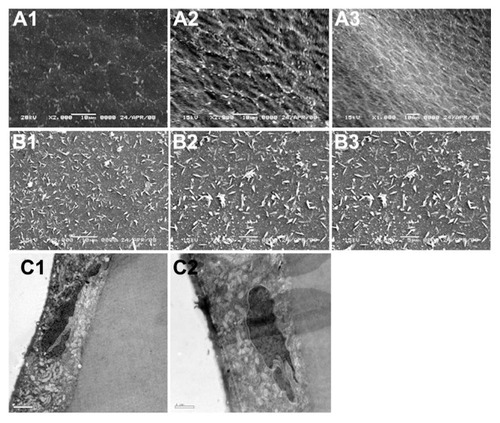
Scanning and transmission electron microscopy analysis
Analysis from scanning and transmission electron microscopy indicated that the corneal endothelium, anterior lens capsule, and epithelium cells from the 5-FU and MMC groups were not changed significantly at day 28 after operation compared to normal corresponding tissues, as shown in . This result indicated a preferable safety profile of using 5-FU and MMC locally.
Figure 5 (A1–C2) Scanning electron microscopy of corneal endothelium and anterior lens capsule, and transmission electron microscopy of corneal endothelial cells on day 28 after operation. (A1) Cornea endothelial cell: smooth surface, in regular hexagonal shape, healthy tight cell junction with microvilli, 200×; (A2) MMC membrane implanted, day 28, no abnormality on cornea endothelial surface, 200×; (A3) 5-FU membrane implanted, day 28, no abnormality on cornea endothelial surface, 100×; (B1) anterior lens capsule from control group, microvilli were observed, 200×; (B2) MMC membrane implanted, day 28, no abnormality on anterior lens capsule surface 200×; (B3) 5-FU membrane implanted, day 28, no abnormality observed on the surface of anterior lens capsule, 200×; (C1) MMC membrane implanted, day 28, microvilli observed on cornea endothelial surface, containing large amount of mitochondria and rough endoplasmic reticulum, no abnormality found, 200×; (C2) 5-FU membrane implanted, day 28, microvilli observed on cornea endothelial surface, containing large amount of mitochondria and rough endoplasmic reticulum, no abnormality found, 200×.
Discussion
Avoiding the ocular scarring after glaucoma filtration surgery is a challenge for ophthalmologists. So far, there has been a lack of ideal and effective ways to solve the problem. Proliferation and migration of fibroblasts play an important role in the wound-healing process, and antimetabolite application has shown improved outcomes following glaucoma filtration operation. However, the systemic application of antimetabolites usually leads to damage of integrity of cornea epithelia, leakage of bleb, sustained low IOP, endophthalmitis, and scleritis, partially due to improper dosing of antimetabolites pre- and postoperation. The application of a sustained-delivery medicine system to release 5-FU and MMC locally provides a possible solution to avoid the potential complications when administrated systemically.
Chitosan is deacetylated chitin, with advantages of ideal biocompatibility, biodegradability, ability to staunch bleeding, and antibacterial effects. These unique features promote tissue repair, reduce scar adhesion, and facilitate drug absorption. Chatelet et alCitation7 found that fibroblasts cannot proliferate or spread on the chitosan membrane though still alive; indicating the selective inhibitory effect of chitosan on the growth of fibroblasts effectively reduces synthesis of collagens and prevents tissue adhesion. It was reported that chitosan eye drops inhibit proliferation of fibroblasts, maintain an unobstructed bleb-filtration pathway, and reduce IOP, and are even superior to antimetabolite thiotepa. Therefore, the application of a biological delivery system, with chitosan as carrier, combined with antimetabolites, has been highly regarded as a potential therapeutic approach in glaucoma operation.Citation8
Chitosan as carrier containing MMC (12 μg) or 5-FU (12 μg) was adopted in this study, being implanted into eyes under sclera during glaucoma filtration operation. IOPs and bleb formation as two indexes to evaluate the effects of glaucoma filtration operation were recorded and evaluated for feasibility and effectiveness (validity) of MMC and 5-FU.
Our findings showed that there was little fibroblastic secretion in the anterior chamber in all operated eyes, no significant difference among all groups, and the secretion disappeared within 1 week after operation. There was no significant difference in blebs in terms of size and shape across all four groups, indicating the success of the operation.
The survival period of blebs in the MMC group was prolonged significantly compared with the other three groups. The ranking of the other three groups in terms of bleb-survival period was 5-FU group > control group > placebo group. Sixty-five percent of blebs in the MMC group survived for about 14 days, moreover, with less angiogenesis, minor inflammation (thinner wall of bleb), and no other complications (lighter color). The MMC group was much superior to the other groups in terms of bleb survival.
shows that there was no difference in IOPs before operation among all four groups. A significant decrease in IOP was observed in the 5-FU and MMC groups 1 week after operation – 31%–52% – almost twice that of the control and placebo groups, which had a decrease of 17%–32%. Significant decrease in IOP compared to preoperation was observed within all 28 days in the MMC group (P < 0.01), whereas within 14 days after operation, IOP rebounded to preoperation levels in the 5-FU group (P < 0.01). Intergroup comparison showed that the MMC group had the longest sustained IOP-decrease period, followed by the 5-FU and control groups. The 5-FU group was superior to the control group, especially at days 15–21 after operation in terms of lower IOP (P < 0.05). Most surprising was that the blank/placebo group, which had blank biological membrane implanted, had the shortest IOP-decrease period, even shorter than the control group. A possible reason for this is that though chitosan has a certain anti-inflammation effect, it is still a kind of foreign tissue that can incur inflammation. It is well known that cytokines and adhesive factors are rapidly released from macrophages once stimulated by explants, followed by increased permeability of blood vessels, accumulation of inflammatory cells (neutrophils and mononucleocytes), and exacerbated inflammation. This is very similar to what we found in the blank group, and confirmed by pathologic study showing massive infiltration of inflammatory cells under sclera in the blank group on day 28 after operation. It was severe local inflammation that resulted in the shorter IOP-decrease period.
Therefore, whether chitosan per se has a powerful anti-inflammatory effect, as reported in the literature, is still an open question. However, once combined with antimetabolites, the anti-inflammatory effect of chitosan becomes obvious.
The stability and histocompatibility of biological materials have great impact on the outcome of operations.Citation9,Citation10 Therefore, we implanted blank biological membranes deliberately into the anterior chamber, and found that the implantation could result in mild anterior chamber flare, with the inflammation regressing gradually 1 week after operation. It took nearly 1 year for the biological delivery membrane to be completely degraded.Citation11
Moreover, the outcome of the operation was also dependent on the total dosage of MMC or 5-FU. It was reported that 12 μg delivered gradually by membrane would maintain the lowest effective dosage to improve operation success. However, an in vitro assay showed that 53% of the total amount of 5-FU was released within 33 hours, whereas it took 136 hours for MMC to release 53% of the total amount.Citation12 Though in vivo release studies have not been performed yet, the current data at least indicated that the effective therapeutic concentration is restricted to the site of operation, and it would take 5-FU and MMC more than 33 hours and 136 hours, respectively, to reach the operation site. Because the carrying capacity of chitosan for MMC or 5-FU has not been defined yet, the maximum tolerated doses of MMC or 5-FU in glaucoma operation were not determined in this study.
In this study, the IOP maintained a relatively lower level for quite a long time in some cases after operation, even though blebs had already disappeared. One possible interpretation is that there might be a potential filtrating pathway created after operation that is invisible to the naked eye; the other possibility is that the toxicity of MMC and 5-FU impairs the secretion of aqueous humor from ciliary epithelium. However, our study indicated that MMC was not detectable at all in aqueous humor from day 4 after operation, and 5-FU concentration varied between 0.01885 and 0.04297 μg/mL within 20 days after operation, which is much lower than the toxic concentration of 1–10 mg/mL.Citation13 Moreover, there was no abnormality of cornea endothelia or ciliary epithelia after implantation under examination by transmission and scanning electronic microscopy. In all, the usage of MMC and 5-FU in a biological delivery membrane so far has demonstrated a favorable safety profile.
MMC membrane is superior to 5-FU based on our discoveries. The inflammatory response is much less in MMC membrane implantation than 5-FU membrane. MMC membrane enables a longer survival period for the bleb, and maintains lower IOP. The fact that MMC is not detectable in aqueous humor might be due to its rapid degradation; it is sensitive to light and therefore degrades in aqueous humor faster. However, the stability of MMC membrane needs further improvement.
In summary, MMC and 5-FU biological delivery membranes were proven to be able to maintain low IOP and filter bleb for a much longer period of time, and had milder postoperative inflammation. Our study provides useful information regarding the safety and efficacy of using MMC and 5-FU biological delivery membranes in glaucoma filtration operation, which makes it a promising new approach in the field of glaucoma research. However the study was performed in an established rabbit filtration-surgery model, and the results may not directly correlate with findings in humans. Further studies are needed to validate its potential use and to determine if these results are consistent with humans.
Acknowledgments
This work is supported by the Clinical Medical Technology Development Characteristic Research Projects (Y0204004041131). We appreciate the valuable comments from other members of our laboratories.
Disclosure
The authors report no conflicts of interest in this work.
References
- GresselMGParrishRK2ndFolbergR5-Fluorouracil and glaucoma filtering surgery: I. An animal modelOphthalmology19849143783836717922
- [No authors listed]Three-year follow-up of the Fluorouracil Filtering Surgery StudyAm J Ophthalmol1993115182928420383
- [No authors listed]Five-year follow-up of the Fluorouracil Filtering Surgery Study. The Fluorouracil Filtering Surgery Study GroupAm J Ophthalmol199612143493668604728
- ShaoTLiXGeJTarget drug delivery system as a new scarring modulation after glaucoma filtration surgeryDiagn Pathol201166421736763
- PolakMBValamaneshFFeltOControlled delivery of 5-chlorouracil using poly(ortho esters) in filtering surgery for glaucomaInvest Ophthalmol Vis Sci20084972993300318579761
- ErricoDScrimieriFRiccardiRFedeliRIarossiGTrabeculectomy with double low dose of mitomycin C – two years of follow-upClin Ophthalmol201151679168622205828
- ChateletCDamourODomardAInfluence of the degree of acetylation on some biological properties of chitosan filmsBiomaterials200122326126811197501
- KaurIPSmithaRPenetration enhancers and ocular bioadhesives: two new avenues for ophthalmic drug deliveryDrug Dev Ind Pharm200228435336912056529
- MarquesAPReisRLHuntJAThe biocompatibility of novel starch-based polymers and composites: in vitro studiesBiomaterials20022361471147811829443
- PuFRWilliamsRLMarkkulaTKHuntJAExpression of leukocyte-endothelial cell adhesion molecules on monocyte adhesion to human endothelial cells on plasma treated PET and PTFE in vitroBiomaterials200223244705471812361609
- LiSNLiuWLiSFBiocompatibility of three different chitosan biomembranes in eyesRecent Adv Ophthalmol2010306517522
- WuZHLiSNLiWHWangNLCompare the inhibitory effects of mitomycin C,5-fluorouracil and dexamethasone on cultured rabbit Tenon’s capsule fibroblastsChin J Pract Ophthalmol2009278883887
- MannisMJSweetEHLewisRAThe effect of fluorouracil on the corneal endotheliumArch Ophthalmol198810668168173370011
- KayJSLitinBSJonesMAFryczkowskiAWChvapilMHerschlerJDelivery of antifibroblast agents as adjuncts to filtration surgery – Part II: Delivery of 5-fluorouracil and bleomycin in a collagen implant: pilot study in the rabbitOphthalmic Surg198617127968012434899