Abstract
Background
Understanding how strabismus impacts a child’s quality of life, as well as their families, should be an important key to guide treatment, not only from the ophthalmological point of view but also regarding psychological and social aspects, which are fundamental for a healthy and harmonious development.
Methods
A cross-sectional study was performed to evaluate the functional vision and eye-related quality of life (ER-QOL) in a population of children with strabismus submitted or not to corrective surgery, using the recently developed Pediatric Eye Questionnaire (PedEyeQ) and to compare with age and gender-matched visually normal children. The PedEyeQ was applied to non-operated children with strabismus (n = 18), operated children with strabismus (n = 24), and visually normal children (n = 21). This instrument is composed of 3 components (Child, Proxy, and Parent) and has different versions according to the child’s age (0–4, 5–11, or 12–17 years-old versions). Clinical data such as age, type of strabismus, angle of deviation, amblyopia, occlusion treatment, and surgical outcome were also recorded.
Results
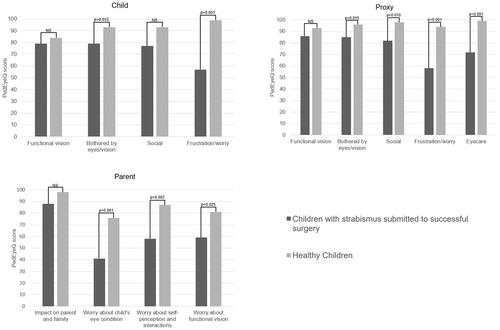
All PedEyeQ domain scores were significantly lower in children with strabismus compared with visually normal children, except the Child “functional vision” domain. Children with strabismus with successful corrective surgery had significantly lower scores in many domains of the Child, Proxy, and Parent components, compared with visually normal children.
Conclusion
This study showed that strabismus has an important impact on affected children and their families, as assessed by PedEyeQ. Interestingly, children with prior successful corrective strabismus surgery had worse PedEyeQ scores compared to visually normal children. Educational programs and psychosocial rehabilitation interventions should be implemented in children with strabismus and their families.
Introduction
Strabismus is a condition in which the visual axis of both eyes is misaligned. Children with strabismus have poorer quality of life than visually normal children, as demonstrated by several studies that used validated questionnaires, including the Hospital Anxiety and Depression Scale (HADS), the 25-item National Eye Institute Visual Functioning Questionnaire (NEI-VFQ-25), the Pediatric Quality of Life Inventory (PedsQL), the Intermittent Exotropia Questionnaire (IXTQ) and, more recently, the Pediatric Eye Questionnaire (PedEyeQ).Citation1–Citation7 However, many of these questionnaires were not specifically designed for children (ie NEI-VFQ-25 and HADS), nor for evaluating the eye-related quality of life (ie HADS, PedsQL). Pediatric instruments should incorporate both child and proxy components.Citation8 Furthermore, the instruments to quantify the impact of vision disorders should be vision-specific, as they provide a higher sensitivity compared with general health-related quality of life instruments.Citation9 Recently, Hatt et alCitation10 developed the vision-specific PedEyeQ, with child and proxy components, to measure the functional vision and eye-related quality of life (ER-QOL) in children and their parents. This is a validated questionnaire that contains age-appropriate questions to assess the impact of strabismus on daily life and well-being from the child’s and parent’s perspectives.Citation11
Understanding how strabismus impacts a child’s quality of life, as well as their families should be an important key to guide treatment, not only from the ophthalmological point of view but also regarding psychological and social aspects, which are fundamental for a healthy and harmonious development. Children with strabismus can suffer from the relationship with peers (eg being less invited to birthday parties), and school performance (eg being negatively viewed by their teachers), becoming more vulnerable to alcohol abuse, depression, and anxiety.Citation12–Citation14
The purpose of this study was to evaluate the functional vision and ER-QOL in a population of children with strabismus submitted or not to corrective surgery, using the recently developed PedEyeQ, and to compare with age and gender-matched visually normal children.
Materials and Methods
This is a cross-sectional study in which the PedEyeQ was applied to non-operated children with strabismus, operated children with strabismus, and visually normal children. Children with strabismus and healthy ones, aged 2 to 17 years old, observed in a Pediatric Ophthalmology appointment in a tertiary center, Centro Hospitalar Universitário do Porto, between September and October 2020, were consecutively selected. Children with a diagnosis of any kind of strabismus, at distance or near fixation (3 meters and 30 cm, respectively), including those submitted to previous corrective surgery, were enrolled. Healthy children had age-appropriate normal best corrected visual acuity in both eyes and no visual disorders.Citation15,Citation16 Children with psychomotor development delays (except cerebral palsy) or eye conditions frequently associated with strabismus, such as amblyopia or refractive errors, were allowed to participate in the study. Children with previous corrective strabismus surgery less than 4 months ago, and parents with a level of English proficiency inferior to that of an independent user (B1 in the Common European Framework of Reference for Languages) were excluded.Citation17
This study was performed in accordance with the Declaration of Helsinki and was approved by the local IRB. The data was completely anonymous, no personal information was collected, and participation in the study was voluntary by accepting to complete the questionnaire. Informed consent was obtained before answering the questionnaire and after proper information about how the aggregated data would be handled. Both the parent and the child (if the child was over 12 years old) gave informed consent.
The clinical data, including age, gender, systemic disorders, type of strabismus, angle of deviation, presence of amblyopia, history of occlusion or penalization therapy (past or present), use of glasses, and previous strabismus surgery (dates and numbers), was assessed at the time of administration of the questionnaire. The diagnosis of strabismus was performed with a cover-uncover test and alternate cover test by a pediatric ophthalmology specialist. The angle of deviation was measured using a prism and alternate cover test and corresponded to the largest prism magnitude that neutralized the deviation. It was defined as small (<10 prismatic diopters [PD]), medium (10–39 PD), and large (>40 PD). Amblyopia was defined as at least a 2-line difference in visual acuity between the two eyes.Citation18 Successful surgical outcome was defined as a postoperative angle of deviation inferior to 10 PD in the primary position with less than 15 degrees of anomalous head posture.
The children and one parent of each child completed the PedEyeQ. The questionnaire was downloaded from the website of the Pediatric Eye Disease Investigator Group (www.pedig.net) and administered in English. One member of the research team explained to the child and parents what this study and questionnaire consisted of, how long it took to complete it, how it was filled out, and made small translations whenever necessary.
The PedEyeQ was developed to assess the functional vision and ER-QOL in children with any eye condition and their parents.Citation10,Citation11 The questionnaire includes three components (Child, Proxy, and Parent) and each has distinct, separately scored domains. The Child PedEyeQ component has two versions (5–11 or 12–17 years-old versions) and is completed by the children. The Proxy and Parent PedEyeQ components have three versions (0–4, 5–11, or 12–17 years-old versions), and are answered by the parent or caregiver. All children with psychomotor development delay were less than 4 years old and, thereby, the whole questionnaire was completed by their parents. The Child PedEyeQ component has four domains: “functional vision”, “bothered by eyes/vision”, “social” and “frustration/worry”. The “functional vision” domain assesses the impact of the eye condition on the child’s daily life, such as playing sports, learning at school, walking, concentrating, and difficulty seeing. The “bothered by eyes/vision” domain evaluates how often the limitations caused by the eye condition bother the child. The “social” domain evaluates the child’s self-perception, the impact of other people’s reactions to the eye condition, and the concerns of the child regarding social interactions. The “frustration/worry” domain assesses the child’s worries and feelings regarding the eye condition, its evolution, and the child’s reaction to the eye care. The Proxy PedEyeQ component contains three domains in the 0–4 years-old version: “functional vision”, “bothered by eyes/vision”, and “social”; and five domains in the 5–11 and 12–17 years-old versions: “functional vision”, “bothered by eyes/vision”, “social”, “frustration/worry”, and “eye care”. The Proxy questionnaire evaluates how the parent or caregiver believes the eye condition affects the child. The Parent PedEyeQ component has four domains: “impact on parent/family”, “worry with child’s eye condition”, “worry with child’s self-perception and interactions”, and “worry with child’s visual function”. This component evaluates the impact of the child’s eye condition in the parent or caregiver and the family. All answers in the PedEyeQ are based on a 3-point frequency scale: “never”, “sometimes”, and “all of the time”.Citation11 For each domain, the Rasch score was calculated using previously published Rasch look-up tables (freely available at: www.pedig.net). The Rasch scores were then converted on a scale from 0 (worst) to 100 (best).
The statistical analysis was performed using IBM SPSS Statistics 26. Categorical variables are summarized as absolute and relative frequency and continuous variables as mean and SD. The comparison of scores between groups was performed with independent sample t-tests or ANOVA test, while the comparison of scores between different domains was performed with paired sample t-tests. When continuous variables had skewed distribution, nonparametric tests were used. Statistical significance was considered in the presence of a p-value inferior to 0.05. A linear regression was carried out to compare the surgical and non-surgical groups, after adjusting for potential confounding factors. The intraclass correlation coefficient (ICC) was used to assess agreement between the child and proxy scores. Based on the 95% confidence interval of the ICC estimate, values less than 0.5, between 0.5 and 0.75, between 0.75 and 0.9, and greater than 0.90 are indicative of poor, moderate, good, and excellent agreement, respectively.Citation19
Results
This study included 42 children with strabismus and 21 visually normal children. Children with strabismus and visually normal children were not different regarding gender (57% vs 63% female, p=0.890), and age (6±4 and 5±2 years, p=0.120). The number of participants with 0–4 years, 5–11 years and 12–17 years was 16 (38%), 18 (43%) and 8 (19%), respectively, in the group of children with strabismus, and 9 (43%), 8 (38%) and 4 (19%) in the control group (p=0.089).
Of the 42 children with strabismus, 24 (57%) had been submitted to one or more strabismus surgeries. The baseline characteristics of children with strabismus, and comparison between surgical and non-surgical groups are shown in . The characterization of children submitted to strabismus surgery is summarized in . Overall, 20 (48%) had exotropia, 18 (43%) had esotropia, and 4 (9%) had hypertropia.
Table 1 Baseline Characteristics of Children with Strabismus
Table 2 Characterization of Children Submitted to Strabismus Surgery
PedEyeQ Scores Comparison Between Children with Strabismus and Visually Normal Children
The mean±SD PedEyeQ scores are represented in .
Table 3 Pediatric Eye Questionnaire (PedEyeQ) Scores in the Study Population
All PedEyeQ domain scores were significantly lower in children with strabismus compared with visually normal children, except the Child “functional vision” domain. Children with successful strabismus surgery had significantly lower scores in many domains compared with healthy ones, as shown in .
PedEyeQ Scores Comparison Between Subgroups of Children with Strabismus
Operated children with strabismus had significantly lower Child “frustration/worry” domain score (p=0.030) compared with non-operated children, but after adjusting for the time since diagnosis and prior occlusion treatment no differences were found. Among the operated children, incisional surgery was associated with a lower Proxy “bothered by eyes/vision” domain score compared with botulinum toxin (86±17 vs 100±0, p=0.029).
Glass wearers had a significantly lower Child “bothered by eyes/vision” domain score (76±19 vs 93±8, p=0.009), and Proxy “functional vision” domain score (81±17 vs 91±12, p=0.019) compared with children with strabismus who did not wear glasses.
PedEyeQ scores by age in children with strabismus are shown in .
Table 4 Pediatric Eye Questionnaire (PedEyeQ) Scores by Age in Children with Strabismus
No differences were found in scores regarding age, gender, psychomotor development delay, strabismus deviation (esotropia or exotropia) and grade, presence of amblyopia, prior or current occlusion treatment, surgical success (postoperative residual deviation < or ≥10 PD), number of previous strabismus surgeries (< or ≥1), time since strabismus surgery (< or ≥12 months ago), and surgery laterality (binocular or monocular).
PedEyeQ Scores Comparison for Each Component (Child, Proxy, and Parent) in Children with Strabismus
In the Child component, the “frustration/worry” domain score was significantly lower than all the other child’s scores (all p<0.001).
In the Proxy component, “frustration/worry” and “eye care” domains scores were both significantly lower than “functional vision” domain score (both p<0.001), “bothered by eyes/vision” domain score (both p<0.001), and “social” domain score (p<0.001 and p=0.006, respectively).
In the Parent component, “worry about child’s eye condition” domain score was significantly lower than all the others parent’s scores (all p<0.001), while the “impact on parent and family” domain score was significantly higher than all the other scores (all p<0.001).
PedEyeQ Scores Comparison Between Child and Proxy Domains Scores in Children with Strabismus
There was an excellent agreement between the Child and Proxy “functional vision” domain scores (ICC 0.909, p<0.001). There was a good agreement between the Child and Proxy “social” domain scores (ICC 0.896, p<0.001), and the Child and Proxy “bothered by eyes/vision” domain scores (ICC 0.830, p<0.001). There was a moderate agreement between the Child and Proxy “frustration/worry” domain scores (ICC 0.657, p=0.013).
Discussion
This study aimed to evaluate the functional vision and ER-QOL in children with strabismus and their parents, using the recently developed and validated questionnaire PedEyeQ. This questionnaire is indicated for children with any eye condition, but it has been scarcely researched in strabismus.Citation6,Citation7,Citation20 In agreement with previous studies, we found that both children with strabismus and their proxies had lower PedEyeQ scores than controls.Citation6,Citation7 Additionally, even those submitted to what was considered a successful strabismus surgery or surgeries had significantly lower scores when compared with visually healthy children.
The impact of strabismus on the quality of life of affected patients has been documented, particularly during adulthood.Citation21,Citation22 In young children, other factors such as amblyopia treatment present an associated issue. It is also harder to evaluate the psychosocial impact of strabismus on children given the inability to self-reporting concerns and feelings. However, it is at least as important to address the functional and psychosocial effects of strabismus during childhood, while the social competencies and personality are developing. There is an increased susceptibility to psychiatric diseases in children with strabismus, with depression or anxiety affecting one-quarter of them.Citation14,Citation23
In the present study, the Child “functional vision” domain was the only PedEyeQ score that did not differ between children with strabismus and healthy children. In contrast, Hatt et alCitation6 found the greatest mean difference between children with strabismus and controls in the Child “functional vision” domain among children aged 5 to 11 years. The discrepant results may be explained by differences in functional vision parameters (visual acuity, visual field, stereopsis) of both cohorts. In our sample, the prevalence of amblyopia was relatively low (21%). The “frustration and worry” domain had the lowest score in the Child and Proxy components in the present study. This is supported by Hatt et al,Citation6 who demonstrated the greatest mean difference between children with strabismus and controls in this domain among children aged 12 to 17 years. Hence, one of the major issues of these patients is that they feel unsure of themselves, frustrated, worried, and different.
There are disparities in results of different studies regarding the impact of the type of strabismus, angle of deviation, presence of amblyopia, and age on quality of life. A study by Uretmen et alCitation13 showed a more pronounced negative social bias against children with strabismus in esotropia versus exotropia. Wen et alCitation3 did not find any differences between both types of strabismus, neither did our study. In the present study, PedEyeQ scores were similarly affected in children with different degrees of eye deviation, in agreement with Lim et al.Citation24 The impact of strabismus may be more related to the patient’s judgment of the problem than to the severity itself. The lack of correlation between the angle of deviation and impairment of quality of life has been also reported in adults.Citation25,Citation26 Nevertheless, patients with latent (no noticeable) deviation have better scores in psychological instruments than those with manifest deviation.Citation27 The presence of amblyopia was not associated with worse PedEyeQ scores in our study. This is in line with the population-based Multi-ethnic Pediatric Eye Disease Study (MEPEDS) which demonstrated a similar impairment between children with concomitant amblyopia and strabismus and children with strabismus alone.Citation3 Unlike strabismus, amblyopia is not apparent to others, so the effect on social and emotional functioning appears to be minimal. On the other hand, occlusion therapy is apparent to others and may be a significant factor in ER-QOL.Citation28 We did not find worse scores in children currently undergoing occlusion treatment, probably because they were only a minority (19%). Instead, more than half (67%) had previously undergone occlusion treatment, which may or may not have a lasting impact on ER-QOL. In accordance with our results, Guimarães et alCitation29 reported that patching was not associated with long-term negative psychosocial outcomes. Not only the occlusion therapy, but also the use of glasses alters the physical appearance. Using PedEyeQ, Leske et alCitation30 recently showed a reduced ER-QOL and functional vision in glasses wearers without strabismus and their parents. Similar findings were demonstrated in our cohort of children with strabismus, which means that the use of glasses may additionally impair the quality of life of these children.
Supported by other studies, the PedEyeQ scores did not significantly differ between age subgroups.Citation5,Citation8 In a study by Sim et al,Citation5 the impact of strabismus on quality of life was observed in children of all ages, as observed in our study, but they found a trend towards higher scores in older children, which could be related to a better coping mechanism and increased maturity and acceptance.Citation8,Citation31
A significant number of studies have reported an improvement in the quality of life of children after strabismus surgery.Citation32–Citation34 Interestingly, this improvement was reported in patients with either successful or unsuccessful surgical outcome.Citation32,Citation35 Some studies showed that children with an unsuccessful surgical outcome do not present lower postoperative quality of life scores compared with those successfully treated, which is consistent with our findings.Citation32,Citation34 This can be explained by an improvement in eye alignment, albeit not attaining the criteria for surgical success. In our cross-sectional study, no differences were found between the surgical and non-surgical cases. We recognize that studies with a prospective design are more appropriate to evaluate the effect of strabismus surgery on ER-QOL. The prospective studies that evaluated the change of ER-QOL scores following surgery did not compare operated children with healthy subjects.Citation32–Citation34 We found that operated children still have worse scores in several parameters of ER-QOL, regardless of surgical outcome, similar to the results in adults of a prospective study by Xu et al.Citation21
The psychosocial impact of strabismus extends to the children’s families. The parents or guardians of children with strabismus have an increased susceptibility to depression, or anxiety, and admit difficulties in establishing a relationship with their children.Citation36,Citation37 Moreover, the psychological status of relatives may depend on the attitude of the children toward treatment and their level of knowledge about the disease.Citation37 Parents’ and children’s concerns may not be the same. In our study, there was a strong agreement between the Child and Proxy components scores, except for the “frustration/worry” domain. Noteworthy, the score of “frustration/worry” domain was lower in the Child component compared with the Proxy component in the surgical group, while the inverse was found in the non-surgical group. This may reflect an underestimation of frustration and worries of children submitted to corrective surgery by their parents. The lack of agreement between self and proxy-reporting, especially in social or emotional domains, has been shown with other instruments.Citation38
In the present study, psychosocial scores of children with strabismus were more impaired than functional scores. Two strategies should be of value in these patients: education and rehabilitation. Rehabilitation interventions are relatively well documented for children with visual impairment, aiming to improve the quality of life, participation in society, and psychosocial functioning.Citation39 However, children with strabismus, and eventually their families, may also benefit from psychosocial rehabilitation strategies. A multidisciplinary approach with ophthalmologists, psychiatrists, or psychologists could help reduce excessive worries and educate parents and children about the disease. Very little is known about the use of psychosocial interventions to improve the quality of life in patients with strabismus, and further research on this topic is needed.Citation22
The first limitation of this study is the relatively small sample size and its heterogeneity. Secondly, a prospective design applying the questionnaire before and after surgery would be more appropriate to address the impact of the surgery on ER-QOL. To our knowledge, this was not done yet with PedEyeQ. Another limitation is the variable time between surgery and questionnaire application, however, a minimum interval of 4 months was implemented to allow for assessment of the surgical outcome. The questionnaire was applied in the English language to Portuguese patients. Only parents who reported a level of English proficiency superior or equal to that of an independent user were included to ensure that they were able to complete the questionnaire themselves, however, this could point to a peculiar social status in the population. The impact of the socioeconomic class was not extensively studied, but previous research showed no correlation between socioeconomic class and the psychosocial impairment caused by strabismus.Citation24,Citation40
To conclude, children with strabismus and their families might have impaired functional vision and reduced ER-QOL. Despite previous evidence of a positive effect of strabismus surgery, children with successful surgical outcome had worse PedEyeQ scores compared to visually normal children. Educational programs and psychosocial rehabilitation interventions should be implemented in children with strabismus and their families.
Ethics
The study was conducted according to the tenets of the Declaration of Helsinki in its latest amendment (Brazil, 2013) and was approved by the local IRB (“Departamento de Ensino, Formação e Investigação”).
Informed Consent
All patients signed an informed consent form.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work. Nisa Silva and Catarina Castro are co-first authors of this work.
Disclosure
The authors have no conflicts of interest for this work to declare.
Additional information
Funding
References
- Chai Y, Shao Y, Lin S, et al. Vision-related quality of life and emotional impact in children with strabismus: a prospective study. J Int Med Res. 2009;37(4):1108–1114. doi:10.1177/147323000903700415
- Tu C, Ye L, Jiang L, Wang Y, Li Y. Impact of strabismus on the quality of life of Chinese Han teenagers. Patient Prefer Adherence. 2016;10:1021–1024. doi:10.2147/PPA.S108771
- Wen G, McKean-Cowdin R, Varma R, et al. General health-related quality of life in preschool children with strabismus or amblyopia. Ophthalmology. 2011;118(3):574–580. doi:10.1016/j.ophtha.2010.06.039
- Hatt SR, Leske DA, Yamada T, Bradley EA, Cole SR, Holmes JM. Development and initial validation of quality-of-life questionnaires for intermittent exotropia. Ophthalmology. 2010;117(1):163–168.e1. doi:10.1016/j.ophtha.2009.06.038
- Sim B, Yap G-H, Chia A. Functional and psychosocial impact of strabismus on Singaporean children. J AAPOS. 2014;18(2):178–182. doi:10.1016/j.jaapos.2013.11.013
- Hatt SR, Leske DA, Castañeda YS, et al. Association of strabismus with functional vision and eye-related quality of life in children. JAMA Ophthalmol. 2020;138(5):528–535. doi:10.1001/jamaophthalmol.2020.0539
- Leske DA, Hatt SR, Wernimont SM, et al. Quality of life and functional vision across pediatric eye conditions assessed using the PedEyeQ. J AAPOS. 2021;25(1):23.e1–23.e5. doi:10.1016/j.jaapos.2020.10.010
- Yamada T, Hatt SR, Leske DA, Holmes JM. Specific health-related quality of life concerns in children with intermittent exotropia. Strabismus. 2012;20(4):145–151. doi:10.3109/09273972.2012.735338
- Raat H, Mohangoo AD, Grootenhuis MA. Pediatric health-related quality of life questionnaires in clinical trials. Curr Opin Allergy Clin Immunol. 2006;6(3):180–185. doi:10.1097/01.all.0000225157.67897.c2
- Hatt SR, Leske DA, Castañeda YS, et al. Development of pediatric eye questionnaires for children with eye conditions. Am J Ophthalmol. 2019;200:201–217. doi:10.1016/j.ajo.2019.01.001
- Leske DA, Hatt SR, Castañeda YS, et al. Validation of the pediatric eye questionnaire in children with visual impairment. Am J Ophthalmol. 2019;208:124–132. doi:10.1016/j.ajo.2019.07.018
- Mojon-Azzi SM, Kunz A, Mojon DS. Strabismus and discrimination in children: are children with strabismus invited to fewer birthday parties? Br J Ophthalmol. 2011;95(4):473–476. doi:10.1136/bjo.2010.185793
- Uretmen O, Egrilmez S, Kose S, Pamukçu K, Akkin C, Palamar M. Negative social bias against children with strabismus. Acta Ophthalmol Scand. 2003;81(2):138–142. doi:10.1034/j.1600-0420.2003.00024.x
- Lin S, Congdon N, Yam JCS, et al. Alcohol use and positive screening results for depression and anxiety are highly prevalent among Chinese children with strabismus. Am J Ophthalmol. 2014;157(4):894–900.e1. doi:10.1016/j.ajo.2014.01.012
- Pan Y, Tarczy-Hornoch K, Cotter SA, et al. Visual acuity norms in pre-school children: the multi-ethnic pediatric eye disease study. Optom Vis Sci. 2009;86(6):607–612. doi:10.1097/OPX.0b013e3181a76e55
- Drover JR, Felius J, Cheng CS, Morale SE, Wyatt L, Birch EE. Normative pediatric visual acuity using single surrounded HOTV optotypes on the Electronic Visual Acuity Tester following the Amblyopia Treatment Study protocol. J AAPOS. 2008;12(2):145–149. doi:10.1016/j.jaapos.2007.08.014
- Council of Europe. Common European Framework of Reference for Languages (CEFR). https://www.coe.int/en/web/common-european-framework-reference-languages/level-descriptions. Accessed September 8, 2021.
- Wallace DK, Repka MX, Lee KA, et al. Amblyopia preferred practice pattern®. Ophthalmology. 2018;125(1):P105–P142. doi:10.1016/j.ophtha.2017.10.008
- Koo TK, Li MY. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med. 2016;15(2):155–163. doi:10.1016/j.jcm.2016.02.012
- Birch EE, Castañeda YS, Cheng-Patel CS, et al. Associations of eye-related quality of life with vision, visuomotor function, and self-perception in children with strabismus and anisometropia. Invest Ophthalmol Vis Sci. 2020;61(11):22. doi:10.1167/iovs.61.11.22
- Xu M, Yu H, Chen Y, Xu J, Zheng J, Yu X. Long-term quality of life in adult patients with strabismus after corrective surgery compared to the general population. PLoS One. 2016;11(11):e0166418. doi:10.1371/journal.pone.0166418
- MacKenzie K, Hancox J, McBain H, Ezra DG, Adams G, Newman S. Psychosocial interventions for improving quality of life outcomes in adults undergoing strabismus surgery. Cochrane Database Syst Rev. 2016;5:CD010092.
- Cumurcu T, Cumurcu BE, Ozcan O, et al. Social phobia and other psychiatric problems in children with strabismus. Can J Ophthalmol. 2011;46(3):267–270. doi:10.1016/j.jcjo.2011.05.017
- Lim SB, Wong WL, Ho RC, Wong IB. Childhood intermittent exotropia from a different angle: does severity affect quality of life? Br J Ophthalmol. 2015;99(10):1405–1411. doi:10.1136/bjophthalmol-2014-306545
- Ritchie A, Colapinto P, Jain S. The psychological impact of strabismus: does the angle really matter? Strabismus. 2013;21(4):203–208. doi:10.3109/09273972.2013.833952
- Sabri K, Knapp CM, Thompson JR, Gottlob I. The VF-14 and psychological impact of amblyopia and strabismus. Investig Ophthalmol Vis Sci. 2006;47(10):4386–4392. doi:10.1167/iovs.05-1365
- Ozates S, Ezerbolat ozates M, Can CU, et al. Improvement in psychiatric symptoms after strabismus surgery in adolescent patients in long-term follow-up. Br J Ophthalmol. 2019;103(7):966–970. doi:10.1136/bjophthalmol-2018-312510
- Hrisos S, Clarke MP, Wright CM. The emotional impact of amblyopia treatment in preschool children. Ophthalmology. 2004;111(8):1550–1556. doi:10.1016/j.ophtha.2003.12.059
- Guimarães S, Carção AA, Carvalho MR, Vieira MJ, Freitas C, Morgado P. Quality of life and mental health in amblyopic children treated with and without occlusion therapy. J AAPOS. 2019;23(6):339.e1–339.e5. doi:10.1016/j.jaapos.2019.09.009
- Leske DA, Hatt SR, Castañeda YS, et al. Eye-related quality of life and functional vision in children wearing glasses. J AAPOS. 2020;24(2):91.e1–91.e6. doi:10.1016/j.jaapos.2019.12.010
- Lukman H, Kiat JE, Ganesan A, Chua WL, Khor KL, Choong YF. Negative social reaction to strabismus in school children ages 8–12 years. J AAPOS. 2011;15(3):238–240. doi:10.1016/j.jaapos.2011.01.158
- Archer SM, Musch DC, Wren PA, Guire KE, Del Monte MA. Social and emotional impact of strabismus surgery on quality of life in children. J AAPOS. 2005;9(2):148–151. doi:10.1016/j.jaapos.2004.12.006
- Wang X, Gao X, Xiao M, et al. Effectiveness of strabismus surgery on the health-related quality of life assessment of children with intermittent exotropia and their parents: a randomized clinical trial. J AAPOS. 2015;19(4):298–303. doi:10.1016/j.jaapos.2015.04.007
- Ziaei H, Katibeh M, Mohammadi S, et al. The impact of congenital strabismus surgery on quality of life in children. J Ophthalmic Vis Res. 2016;11(2):188–192. doi:10.4103/2008-322X.183918
- Mruthyunjaya P, Simon JW, Pickering JD, Lininger LL. Subjective and objective outcomes of strabismus surgery in children. J Pediatr Ophthalmol Strabismus. 1996;33(3):167–170. doi:10.3928/0191-3913-19960501-09
- Akay AP, Cakaloz B, Berk AT, Pasa E. Psychosocial aspects of mothers of children with strabismus. J AAPOS. 2005;9(3):268–273. doi:10.1016/j.jaapos.2005.01.008
- Kitasato M, Iwamitsu Y, Iwata Y, Ueta T, Fukaya E, Ishikawa H. Investigation of stress and distress experienced by guardians of children with strabismus and/or amblyopia. J Binocul Vis Ocul Motil. 2020;70(1):21–28. doi:10.1080/2576117X.2019.1691872
- Hatt SR, Leske DA, Adams WE, Kirgis PA, Bradley EA, Holmes JM. Quality of life in intermittent exotropia: child and parent concerns. Arch Ophthalmol. 2008;126(11):1525–1529. doi:10.1001/archopht.126.11.1525
- Elsman EBM, Al Baaj M, van Rens GHMB, et al. Interventions to improve functioning, participation, and quality of life in children with visual impairment: a systematic review. Surv Ophthalmol. 2019;64(4):512–557. doi:10.1016/j.survophthal.2019.01.010
- Kothari M, Balankhe S, Gawade R, Toshnival S. Comparison of psychosocial and emotional consequences of childhood strabismus on the families from rural and urban India. Indian J Ophthalmol. 2009;57(4):285–288. doi:10.4103/0301-4738.53053