Abstract
Purpose
To evaluate the safety and efficacy of different methods of transconjunctival cannulated vitrectomy versus conventional non-cannulated vitrectomy in various vitreoretinal disorders.
Methods
A prospective randomized study was done from August 2009 to February 2011. The study included 129 eyes of 122 patients, randomly divided into four groups. Group 1 comprised 34 eyes operated on using transconjunctival 20-gauge cannula Claes system. Group 2 comprised 32 eyes operated on using transconjunctival cannulated 23 gauge system. Group 3 comprised 27 eyes operated on using combined 20-gauge non-cannulated and 23-gauge transconjunctival cannulated system. Group 4 comprised 36 eyes operated on using conventional non-cannulated 20-gauge system.
Results
The four groups were demographically similar. Anatomical outcome was achieved in all cases. Vision was improved in 29 eyes (85.3%) in group 1, 23 eyes (71.9%) in group 2, 19 eyes (70.4%) in group 3, and 26 eyes (72.2%) in group 4. There was no statistical difference between the four groups 1-day postoperative (P=0.405) and 1-week postoperative intraocular pressure (P=0.254). The number of sutureless sclerotomies was 68 (66.6%) in group 1, 78 (81.3%) in group 2, 50 (61.8%) in group 3, and 0 in group 4. Hypotony occurred in one eye (2.9%) in group 1, three eyes (9.4%) in group 2, two eyes (7.4%) in group 3, and no eyes in group 4. Operative endophthalmitis did not occur in any one of the four groups.
Conclusion
Final anatomical and functional outcomes were not related to the type of sclerotomy used (cannulated or non-cannulated), the gauge used (20 or 23), the route (transconjunctival or transscleral), or type of suture used. The advantages of small-gauge transconjunctival vitrectomy were patient comfort, early ambulation, and preservation of the conjunctiva. This should be weighed against the cost of this cannula system.
Keywords:
Summary statement
The advantages of the 20-gauge transconjunctival cannulated vitrectomy are that it enables the use of conventional 20-gauge instruments, and is sutureless. The advantages of the 23-gauge system is that it is entirely sutureless so, in addition to rapid visual recovery and less postoperative inflammation and discomfort, it is especially beneficial in patients requiring multiple interventions. The advantages of combination vitrectomy over a pure 23-gauge vitrectomy are faster gel removal and enhanced ability to manipulate with a wide array of 20-gauge instruments.
Introduction
Sutureless vitrectomy has rapidly been accepted as an essential part of a vitreoretinal surgical setup. The size and structure of the wound along with near intact conjunctival covering makes the incision self-sealing and safe. This allows the vitrectomy instruments to be used without creating an initial limited peritomy to expose bare sclera, and obviates the need for sutures at the end of the procedure.
Wound construction is the essential step in ensuring postoperative wound stability. Both one-step and two-step wound constructions have been described. Key points include an oblique, tunneled approach to ensure a valve-like effect as well as misalignment of conjunctival and scleral wounds by displacing conjunctiva during construction.
Advantages include decreased operative times in certain cases and decreased postoperative inflammation, early postoperative rehabilitation, improved patient comfort, and minimal conjunctival damage. Complications are based around wound competence, hypotony, and its relationship to endophthalmitis rates. Early reports highlighted an increase in endophthalmitis, although further studies are required to accurately assess the incidence. Endophthalmitis has not been reported in cases that have undergone fluid/air exchange.Citation1
Patients and methods
This is a prospective study carried out from August 2009 to February 2011 on 129 eyes of 122 patients, divided randomly into four groups. Group 1 comprised 34 eyes operated on using transconjunctival 20-gauge cannula Claes system (DORC, Zuidland, The Netherlands). Group 2 comprised 32 eyes operated on using transconjunctival cannulated 23-gauge system. Group 3 comprised 27 eyes operated on using combined 20-gauge non-cannulated and 23-gauge transconjunctival cannulated system. Group 4 comprised 36 eyes operated on using conventional non-cannulated 20-gauge system. Indications of surgery are summarized in .
Table 1 Preoperative diagnosis of the studied groups
All patients were subjected to full history taking (including medical history [diabetes mellitus and hypertension] and ophthalmic history [eg, intravitreal injection, operations, trauma, and laser drugs]), examination (including best-corrected visual acuity) measurement using Snellen’s chart, intraocular pressure (IOP) measurement using Goldmann applanation tonometer, anterior segment examination using slit lamp, and dilated fundus examination. Investigations (as needed) included ocular ultrasonography, optical coherence tomography, and fundus fluorescein angiography.
Approval was obtained from the ethics review board of Magrabi Hospital for this study. After discussing the nature of surgery with the patients, including the potential risks and complications, all subjects signed a written informed consent document before surgery. All surgeries were performed by a single surgeon (HHG) and at a single center (Magrabi Eye Hospital, Tanta, Egypt).
The vitrectomy machine used was the Accurus Vitrector (Alcon Laboratories, Inc., Fort Worth, TX, USA) and was used for all surgical procedures. The laser machine used was the Nidek diode laser DC 3300 (Nidek Inc., Gamagori, Japan). The illumination system used was that of Accurus Vitrector, Xenon Brightstar illumination system (DORC), Hexon light (DORC), and Xenon light (Geuder AG, Heidelberg, Germany). Viewing system used was Binocular indirect ophthalmomicroscope (BIOM) wide angle viewing system (OCULUS Optikgeräte GmbH, Wetzlar, Germany) and Machemer magnifying lens for macular disorders.
Surgical techniques
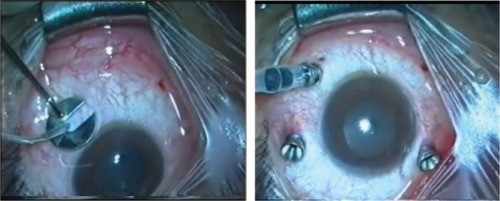
20-gauge Claes system pars plana vitrectomy (PPV) ()
This technique was performed using the Dutch Ophthalmic Research Center two-step reusable cannula Claes system (DORC) with and without valve.
The conjunctiva was displaced using a pressure plate with a central opening 3.5 mm from the edge. Angled incisions were made in the conjunctiva and sclera through the pars plana with a 20-gauge 45° angled microvitreoretinal (MVR) blade in the inferotemporal, superonasal, and superotemporal quadrants parallel to the limbus. The blade was inserted at an angle of approximately 10° to the sclera, 3.5 mm posterior to the limbus, through the central opening of the pressure plate. While keeping the pressure plate in place, the blunt microtrocars were inserted through these wounds, and the infusion cannula was placed in the inferotemporal quadrant, while the superonasal and superotemporal cannulas were used for the retinal instrumentation.
In cases of diabetic vitrectomy, endolaser treatment was applied with a straight 20-gauge laser probe (Nidek). For tractional retinal detachments, membrane dissection was performed primarily with the 20-gauge vitrectomy probe and 20-gauge curved scissor using unimanual dissection. If any of the ports demonstrated persistent leakage, the sclerotomy site was closed, either transconjunctivally or transsclerally using 7–0 Vicryl (PGA) sutures, AssuCryl®, Pully-Lausanne, Switzerland.
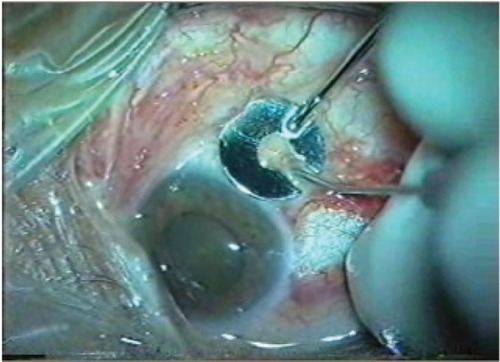
23-gauge PPV
Two-step technique ()
This technique was performed using the Dutch Ophthalmic Research Center two-step reusable system (DORC), the Oertli disposable system, or the MicroVision disposable system.
The conjunctiva was displaced using a pressure plate with a central opening 3.5 mm from the edge. Angled incisions were made in the conjunctiva and sclera through the pars plana with a 23-gauge 45° angled MVR blade in the inferotemporal, superonasal, and superotemporal quadrants parallel to the limbus. The blade was inserted at an angle of approximately 30° to the sclera, 3.5 mm posterior to the limbus, through the central opening of the pressure plate. While keeping the pressure plate in place, the blunt microtrocars were inserted through these wounds, and the infusion cannula was placed in the inferotemporal quadrant, while the superonasal and superotemporal cannulas were used for the retinal instrumentation.
One-step technique ()
This technique was performed using Alcon disposable system or Geuder disposable system with valve.
The trocar was inserted at an angle of approximately 30° to the sclera, 3.5 mm posterior and parallel to the limbus. The direction was then changed to be perpendicular to the sclera to enter the vitreous cavity then the trocar was removed leaving the cannula in place.
For tractional retinal detachments, membrane dissection was performed using the 23-gauge vitrectomy probe as a scissor.
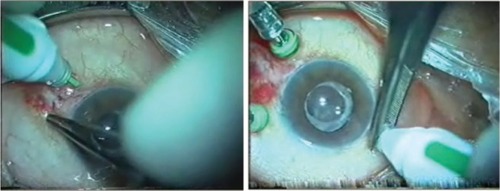
20- and 23-gauge PPV ()
Two 23-gauge sclerotomies were performed (by using the two-step or one-step technique, the disposable or reusable systems) for infusion cannula and illumination probe. One sclerotomy was performed using 20-gauge MVR blade (by reversed scleral incision technique) for vitrectomy using conventional 20-gauge instruments.
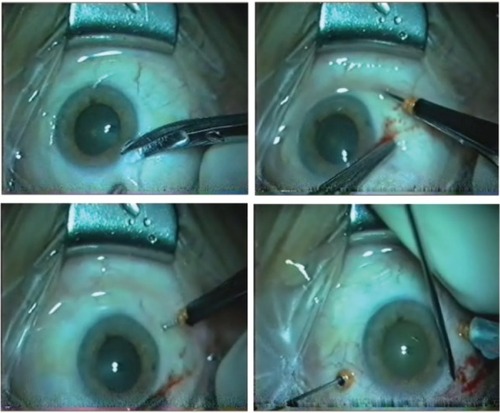
Conventional 20-gauge PPV
Three ports were done by 20-gauge MVR blade. The infusion cannula was fixed infratemporally. Vitrectomy was completed and then all sclerotomies were closed by Vicryl 7–0 sutures.
Postoperatively, all eyes were treated with tobramycin and dexamethasone (Tobradex®; Alcon Laboratories Inc., Fort Worth, TX, USA) eye drops during the postoperative period. Follow-up was done at 1-day postoperative and 1-week postoperative, and then every 4–6 weeks. Postoperative data included postoperative IOP, best-corrected visual acuity at last visit, postoperative anatomical success, lens status, and complications.
Results were collected, tabulated, and statistically analyzed by SPSS statistical package (SPSS Inc., Chicago, IL, USA) version 11.
Results
This is a prospective study carried out from August 2009 to February 2011 on 129 eyes of 122 patients divided randomly into four groups.
Group 1 comprised 34 eyes operated on using 20-gauge cannula Claes system. This group included 16 males (47%) and 18 females (53%). The age range was 20–67 years (mean ± standard deviation [SD] 52.97 ± 10.51). The mean follow-up was 16.70 ± 14.88 weeks (range 12–64 weeks).
Group 2 comprised 32 eyes operated on using the 23-gauge cannula Eckardt system.Citation12 This group included 13 males (40.6%) and 19 females (59.4%). The age range was 11–75 years (mean ± SD 51.06 ± 14.27). The mean follow-up was 16.97 ± 9.14 weeks (range 12–38 weeks).
Group 3 comprised 27 eyes operated on using one conventional 20-gauge opening and two 23-gauge openings. This group included 13 males (48.1%) and 14 females (51.9%). The age range was 30–65 years (mean ± SD 52.89 ± 8.36). The mean follow-up was 28.48 ± 13.56 weeks (range 12–56 weeks).
Group 4 comprised 36 eyes operated on using the conventional 20-gauge system. This group included 23 males (63.9%), and 13 females (36.1%). The age range was 15–78 years (mean ± SD 46.92 ± 17.31). The mean follow-up was 38.30 ± 14.94 weeks (range 12–64 weeks).
With regard to the phakic state, in group 1, there were 30 phakic eyes, three pseudophakic eyes, and one eye with posterior dislocated lens. In group 2, there were 24 phakic eyes, seven pseudophakic eyes, and one eye with posterior dislocated intraocular lens. In group 3, there were 25 phakic eyes and two pseudophakic eyes. In group 4, there were 32 phakic eyes and four pseudophakic eyes.
With regard to the type of tamponade used, silicone oil tamponade was used in 21 eyes (61.8%) in group 1, eleven eyes (34.4%) in group 2, 17 eyes (63%) in group 3, and 28 eyes (77.8%) in group 4. Gas tamponade was used in one eye (2.9%) in group 1, three eyes (9.4%) in group 2, four eyes (14.8%) in group 3, and eight eyes (22.2%) in group 4. Air tamponade was used in eleven eyes (32.3%) in group 1, 17 eyes (53.1%) in group 2, five eyes (18.5%) in group 3, and no eyes in group 4. Fluid tamponade was used in one eye (2.9%) in group 1, one eye (3.1%) in group 2, one eye (3.7%) in group 3, and no eyes in group 4.
The number of sutureless sclerotomies was 68 (66.6%) in group 1, 78 (81.3%) in group 2, 50 (61.8%) in group 3, and 0 in group 4 ().
Table 2 Operative sutures of the studied four groups
Anatomical outcome
Anatomical outcome was achieved in all cases (eg, flattening of the retina in retinal detachment cases, removal of tractional membranes in tractional retinal detachment cases).
Visual outcome
There was highly significant statistical difference between preoperative and postoperative visual acuity in group 1 (P=0.0001), group 2 (P=0.001), group 3 (P=0.003), and group 4 (P=0.002). In group 1, vision was improved from a mean of 20/1218 ± 724.43 (range 20/2000–20/50 in 32 cases + two cases of light perception [LP]) to 20/449 ± 531.60 (range 20/2000–20/40 in 33 cases + one case of LP). In group 2, vision was improved from a mean of 20/1032 ± 821.69 (range 20/2000–20/25 in 31 cases + one case of LP) to 20/346 ± 435.22 (range 20/2000–20/30 in 32 cases). In group 3, vision was improved from a mean of 20/1123 ± 648.04 (range 20/2000–20/80 in 24 cases + three cases of LP) to 20/583 ± 442.07 (range 20/1600–20/28 in 24 cases + three cases of LP). In group 4, vision was improved from a mean of 20/1151 ± 818.35 (range 20/2000–20/300) to 20/522 ± 522.31 (range 20/2000–20/50).
Vision was improved in 29 eyes (85.3%) in group 1, 23 eyes (71.9%) in group 2, 19 eyes (70.4%) in group 3, and 26 eyes (72.2%) in group 4. Vision remained unchanged in three eyes (8.8%) in group 1, three eyes (9.4%) in group 2, three eyes (11.1%) in group 3, and two eyes (5.5%) in group 4. Vision was worsened in two eyes (5.9%) in group 1, six eyes (18.7%) in group 2, five eyes (18.5%) in group 3, and eight eyes (22.2) in group 4.
IOP
With regard to the preoperative, 1-day postoperative, and 1-week postoperative IOP of patients of the studied groups, there was statistical difference (P=0.030) between the four groups regarding the preoperative IOP, and there was no statistical difference between them regarding 1-day postoperative (P=0.405) and 1-week postoperative IOP (P=0.254) ().
Table 3 Preoperative, 1-day postoperative, and 1-week postoperative intraocular pressure of patients of the studied groups
Complications
Non-entry site iatrogenic retinal tears occurred in 10 eyes (29.4%) in group 1, three eyes (9.4%) in group 2, seven eyes (25.9%) in group 3, and two eyes (5.5%) in group 4. All iatrogenic tears occurred during dissection of membranes from the retina. There were no entry-site tears in the four groups. Cataract occurred in nine (30%) out of phakic (30) eyes in group 1, seven (29.1%) out of phakic (24) eyes in group 2, 13 (52%) out of phakic (25) eyes in group 3, and ten (31.2%) out of phakic (32) eyes in group 4. In all cases, no cataract extraction was performed during follow-up. Persistent high IOP, despite maximal medical treatment, occurred in two eyes (5.9%) of group 1 and did not occur in the other groups. In both cases, silicone oil tamponade was used. One case was treated with silicone oil removal after 4 months of primary surgery, and the other case did not complete follow-up. Rubeosis occurred in one eye (2.9%) of group 1 and did not occur in the other groups. This case was treated with intravitreal avastin, and the rubeosis disappeared. Recurrent vitreous hemorrhage occurred in two eyes in group 1 and three eyes in group 2. Hypotony (defined as IOP ≤ 6 mmHg) occurred in one eye (2.9%) in group 1, three eyes (9.4%) in group 2, two eyes (7.4%) in group 3, and no eyes in group 4. In all eyes, IOP was normalized within 2–4 days postoperative, no choroidal detachment occurred, no supplemental tamponade was needed, and it had no effect on the visual outcome. Operative endophthalmitis (within 1-week postoperative) did not occur in any of the four groups.
Discussion
Since the introduction of systems for sutureless vitrectomy surgery, there has been debate about which approach is best. We now have options for 20-, 23-, 25-, and 27-gauge instrumentation. Which can provide the best results, ie, the most efficient surgery with the fastest healing, the least inflammation, and the fewest postoperative complications? Which is the most cost-effective? It will take time to answer all these questions.Citation7
This study showed that final anatomical and functional outcomes were not related to the type of sclerotomy used (cannulated or non-cannulated), the gauge used (20 or 23), the route (transconjunctival or transscleral), or type of suture used. The advantages of small-gauge transconjunctival vitrectomy were patient comfort, early ambulation, and preservation of the conjunctiva. This should be weighed against the cost of this cannula system.
This study showed statistically significant difference between pre- and postoperative visual acuity comparable to other studies.Citation2–Citation6,Citation11
The differences between preoperative and postoperative IOP at 1 day and at 1 week were statistically insignificant in group 1 (similar to the work of Atienza et alCitation7) and group 3. There was a statistically significant difference between preoperative and 1-week postoperative IOP (P=0.018) in group 2 (inconsistent with the work of El-BatarnyCitation2 and the work of Erakgun and EgrilmezCitation5).
We used sutures to close sclerotomies if they were leaky, gapped or not covered by the conjunctiva, similar to that recommended by El-BatarnyCitation2 and Kim et al.Citation3,Citation9 We found that leaky sclerotomies were more related to young age and vitreous base dissection, coinciding with the work of Erakgun and EgrilmezCitation5 and Woo et al.Citation10
Non-entry site iatrogenic retinal tears in this study were related to dissection of membranes from the retina in cases of tractional retinal detachment and not to the type of sclerotomy used. This was also seen in other reports.Citation2,Citation4,Citation8
Postoperative hypotony in this study was related to poor wound construction and young age but not related to the gauge used. This was clear in the conventional 20-gauge group, in which no hyoptony was observed; this is consistent with the work of Misra et al.Citation8 No complications were encountered from hypotony like choroidal effusion and retinal folds, which is also consistent with other reports.Citation5,Citation8,Citation10
Disclosure
The authors report no conflicts of interest in this work.
References
- WarrierSKJainRGilhotraJSNewlandHSSutureless vitrectomyIndian J Ophthalmol20085645345818974514
- El-BatarnyAMTransconjunctival sutureless 23-gauge vitrectomy for vitreoretinal diseases: outcome of 30 consecutive casesMiddle East Afr J Ophthalmol2008159910521369464
- KimMJParkKHHwangJMYuHGYuYSChungHSafety and efficacy of transconjunctival sutureless 23 gauge vitrectomyKorean J Ophthalmol200721420120718063883
- FineHFIranmaneshRIturraldeDSpaideRFOutcomes of 77 consecutive cases of 23 gauge transconjunctival vitrectomy surgery for posterior segmentOphthalmology20071141197120017544779
- ErakgunTEgrilmezSSurgical outcomes of transconjunctival sutureless 23-gauge vitrectomy with silicone oil injectionIndian J Ophthalmol200957210510919237782
- KumarAKakkarAJindalSRajeshRCombination 20 and 23-gauge transconjunctival vitrectomy: a new approachIndian J Ophthalmol20095745946119861749
- AtienzaNFSayEAGarciaCPTanquecoRESayASComparison between the DORC (Claes) and Synergetics 20 gauge trocar systems for sutureless transconjunctival vitrectomy surgeryPaper presented at: Retina Congress 2009September 30–October 4, 2009New York, NY
- MisraAHo-YenGBurtonRL23-gauge sutureless vitrectomy and 20-gauge vitrectomy: a case series comparisonEye20092351187119118535586
- KimJEShahSChoiDHanDPConnorTBTransconjunctival 20-gauge pars plana vitrectomy using a single entry cannulated sutureless systemRetina20092991294129819696700
- WooSJParkKHHwangJMKimJHYuYSChungHRisk factors associated with sclerotomy leakage and postoperative hypotony after 23-gauge transconjunctival sutureless vitrectomyRetina200929445646319174725
- LafetáAPClaesCTwenty-gauge transconjunctival sutureless vitrectomy trocar systemRetina2007271136114118040260
- EckardtCTransconjunctival sutureless 23-gauge vitrectomyRetina20052520821115689813