Abstract
Purpose
To present a case series on the management options for capillary hemangiomas involving the eyelid and orbit.
Methods
This is a retrospective chart review of clinically diagnosed capillary hemangioma cases involving the periocular region treated at two local eye institutions. The patients’ demographics and clinical presentation – including visual acuity, refractive error, periorbital and orbital examinations, and ultrasound and magnetic resonance imaging findings – were reviewed. The clinical progression, modalities of treatment, and treatment outcomes were studied.
Results
Sixteen cases of capillary hemangiomas involving the eyelid and orbit were studied. The mean age at consultation was 9.6 months (range: 1 month–72 months). The majority were females (75%), with 50% presenting as upper-eyelid hemangiomas and the remaining as lower-eyelid (38%) and glabellar (12%) lesions. Combined superficial and deep involvement was common (64%). Cases whose lesions were located at the upper eyelid or superior orbit led to amblyopia (25%). Fifty-six percent of cases (9/16) were managed conservatively, and 44% (7/16) underwent treatment with either single-agent (n = 4) or combined treatments (n = 3).
Conclusion
Close monitoring of visual development and prompt institution of amblyopia therapy for children with periocular capillary hemangiomas generally preserve vision. Extensive lesions that affect the visual axis require local and systemic treatments, alone or in combination, in order to reduce the size and impact of lesions on the eyeball, to reduce induced refractive error and visual occlusion, and to prevent the development of amblyopia, in order to achieve good visual outcomes.
Video abstract
Point your SmartPhone at the code above. If you have a QR code reader the video abstract will appear. Or use:
Introduction
Periocular capillary hemangiomas are common benign vascular tumors seen in children. Histologically, they are characterized by proliferating endothelial cells. They generally present within a few weeks after birth and undergo a rapid proliferating phase, followed by a period of relative quiescence, regressing after a few years into an involution phase.Citation1–Citation9 The clinical course can be variable. Demographically, these cases occur commonly among females and have not been reported to vary by race, ethnicity, or geographic location.Citation1–Citation6,Citation8,Citation10
Haik et alCitation1 and others classified these lesions according to their characteristics on clinical presentation (eg, strawberry nevus, bluish discoloration), while RootmanCitation11 presented another classification based on the level of involvement (eg, superficial, subcutaneous, deep orbital, or combined).Citation1,Citation2 Hemangiomas of the eyelid and orbit have also been studied according to their size. Schwartz et alCitation2 found that half of the cases with hemangiomas exceeding a widest diameter of one centimeter would require treatment. Regardless of the method of classification, hemangiomas can present at any single location or at a combination of locations within the periocular region.Citation2,Citation11
Acceptable indications for intervention may include rapidly enlarging lesions, obstruction of the visual axis, significant induced astigmatism, and cosmetic concerns. Here, a short series based on local experiences is presented, along with some of the current treatment modalities. The modalities available are intralesional and systemic steroid, bleomycin, interferon-alpha, vincristine, cyclophosphamide, topical timolol maleate, oral propranolol, and surgical excision.Citation1,Citation3,Citation5,Citation7–Citation20
Materials and methods
This is a retrospective chart review of 16 clinically-diagnosed capillary hemangioma cases that presented as red or bluish elevated vascular lesions in the periocular region seen at our institutions. This study has obtained approval from the institutional review board.
The parameters reviewed include age at presentation; size and location of the lesion; best corrected visual acuity using preferential looking tests, Kay pictures, Snellen, or HOTV charts (the top row of letters tested) (depending on the patient’s age); and the results of cycloplegic refraction, orbital, and eyelid examinations. Imaging studies such as magnetic resonance imaging (MRI), magnetic resonance angiography, and ultrasound were studied when available. The management of each patient was reviewed, including indications, modes of treatment, and patients’ responses and outcomes. The clinical progression, related complications, and final visual outcome at end of follow-up were studied. The effectiveness of treatment was ascertained when either partial or complete reduction in the size of the hemangioma was observed, based on clinical photographs and measurements.
Results
Sixteen cases of capillary hemangiomas involving the eyelids and orbits were reviewed. The mean age at consultation was 9 months (range: 1 month–72 months) with a median of 4 months. Seventy-five percent (n = 12) were females, and 25% (n = 4) were males. Eighty-one percent (13) were born full term, while 19% (3) were delivered prematurely (>36 weeks age of gestation) ().
Table 1 Patients’ characteristics
Laterality and location
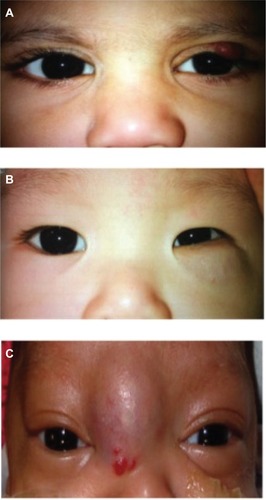
Superficial lesions, which appear as scarlet red in color, were seen in 22% of the cases. Subcutaneous lesions, which appear as bluish-purple hues beneath the skin, were seen in 14% of the cases. Both superficial and subcutaneous features appeared together in 64% of the cases ().
Figure 1 Types of hemangioma according to depth of involvement.
Notes: (A) Superficial left upper-eyelid hemangioma. (B) Subcutaneous left lower-eyelid hemangioma. (C) Combined superficial and subcutaneous hemangioma in the glabella.
Seven cases (44%) had right-sided hemangiomas; similarly, another seven cases (44%) were left-sided. Two cases (12%) had hemangiomas located over the glabellar region, with forehead extension. Upper-eyelid hemangiomas were seen in eight cases (50%) and six (38%) were found in the lower eyelid. Of the cases found in the upper lid (eight), six (75%) measured >1 cm, and two cases (25%) measured <1 cm in diameter. None had bilateral lesions.
Vision, refraction, and amblyopia
The mean logarithm of the minimum angle of resolution (logMAR) visual acuity was 0.77 at the first visit and 0.46 upon the most recent examination (). Of those patients with recorded cycloplegic refraction, a majority of the children less than 2 years of age were hyperopic, with mean spherical refractions of +1.83 and +1.00 on the first and last visits, respectively. All cases whose lesions were located in the upper eyelid had astigmatism, with a mean cylinder of –1.714 (range: 0.75–4.25).
Table 2 Mean visual acuity, and sphere and cylinder refraction at first and last visits
Twenty-five percent (4/16) of patients (mean age of 4 months) were found to be amblyopic during the follow-up period. The majority (75%) were amblyopic because of anisometropia, and a quarter (25%) were amblyopic because of occlusion of the visual axis; all of them had lesions located in the upper eyelid. No cases with lower-eyelid lesions had ambylopia. Two cases presented with proptosis, globe displacement, and limitation in eye movement due to lesions extending deep into the orbit.
Fifty-six percent (9/16) were managed conservatively. Of the remaining 44%, treatment was either with a single agent (57%) or a combination (43%) ().
Table 3 Modes of treatment used for periocular capillary hemangiomas in this series
Management
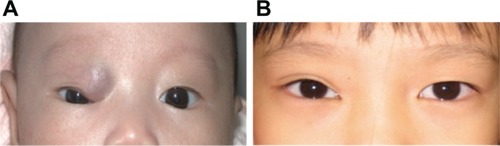
The mean follow-up was 19 months (range: 1.5–72 months), and 12% (n = 2) were lost to follow-up. Fifty-six percent (nine) were managed conservatively, which involved regular spectacle correction and amblyopia therapy, by taping and/or patching, as well as close follow-up. By two years of age, seventy-eight percent (7/9) showed notable regression (according to clinical photos and clinical examinations) in the size of the hemangioma ().
Figure 2 Photograph of one case of capillary hemangioma that resolved spontaneously without treatment at (A) 4 months old upon first visit and at (B) 5 years old upon latest visit.
Forty-four percent (7/16) required medical or surgical intervention. Indications were deep orbital extension, occlusion of the visual axis, and cosmetic concerns.
The treatments we employed included: (1) steroid therapy, (2) surgical excision, (3) oral propranolol, and (4) bleomycin (received at other institutions), either singly or in combination (). Among those that received treatment, 57% (four) were treated with a single agent (oral propranolol, prednisolone, or surgery), and regression was noted in three of them. One developed respiratory distress after propranol therapy, and medication was immediately terminated.
The remaining 43% (three) received a combination of two to three agents (oral prednisolone and intralesional triamcinolone:betamethasone; oral propranolol and intralesional bleomycin, or surgical excision and topical timolol maleate). Regression was observed in two of them. One case that underwent surgical excision for a small superficial hemangioma involving the left medial upper eyelid had a recurrence after 2 weeks. Application of topical timolol maleate 0.5% eyedrops twice daily was advised. However, in this case, there was no change in the size of the lesion after 1 month of eyedrop application. One patient treated with oral prednisolone and intralesional triamcinolone:betamethasone experienced a complication of orbital cellulitis, which was subsequently treated with intravenous antibiotics and drainage of the subperiosteal abscess.
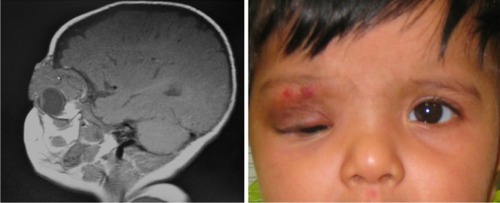
Propranolol
Three patients were treated with oral propranolol. Reduction in the size of the lesion was observed in two out of the three cases. One of the cases treated with oral propranolol was a 6-month-old female with amblyopia from mechanical ptosis, with two previous intralesional bleomycin injections, 2 months apart, from another institution. The hemangioma showed remarkable reduction at the time of consultation at our institution (). The second case was a preterm female with subcutaneous hemangioma involving the left superomedial orbit with maximal MRI axial dimensions of 1.7 × 1.9 cm, which decreased to a clinical measure of 0.8 × 0.3 cm after 7 weeks of treatment.
Figure 3 A 6-month-old female with combined superficial and deep hemangioma over the right superior orbit with inferior globe displacement.
Abbreviation: MRI, magnetic resonance imaging.
Surgery
Surgical removal was performed on two patients. The first case was a 22-month-old female with a glabellar lesion described as an enhancing mass with flow voids in the subcutaneous tissues, representing an arteriovenous malformation. Post-excision, histology reported an ovoid mass with lobulated nests of capillary hemangioma. No recurrence was observed in this case.
Discussion
Capillary hemangiomas represent an abnormal growth of blood vessels characterized by endothelial proliferation. They expand progressively in weeks to months, then involute over the years.Citation1–Citation9,Citation11,Citation22 Formerly dense endotheliomatous lesions during the growth phase become replaced by fewer endothelial channels, increased collagen deposition, and fat, as well as inflammatory cells, as lesions regress.Citation11
The clinical diagnosis of capillary hemangiomas is often straightforward. Superficial hemangiomas may affect the lid or conjunctiva and appear as strawberry lesions, scarlet red in color, whereas deeper lesions lie posterior to the orbital septum and present as a subcutaneous bluish hue. Combined presentations have both superficial and deep components. Entities known as complex hemangiomas are found to be multicentric. These hamartomas often present as isolated lesions or, in rare instances, with systemic associations, such as Kassabach-Merritt syndrome (thrombocytopenia) and neurocutaneous PHACE syndrome (a disorder in which a child is born with posterior fossa malformation, cervico-facial hemangiomas, arterial anomalies, cardiac defects, and various eye anomalies).Citation11,Citation21,Citation22 None of the patients in our series had associated systemic syndromes.
Imaging studies help support the diagnosis. B-scan and Doppler ultrasonography showed the lesions exhibited high echogenicity, with either smooth lobular or irregular contours, and fast blood flow. Computed tomography showed the lesions as well-defined homogenous or inhomogenous, moderate-to-intense enhancing masses. MRI also showed them to be well defined, with some irregular margins, and with low signal intensity on T1-weighted images versus high signal intensity on T2-weighted images with respect to fat and extraocular muscles. With gadolinium, the capillary hemangiomas demonstrated heterogenous or homogenous enhancement. These lesions could be found in any or in a combination of compartments within the orbit, being intraconal and extraconal, pre- and postseptal.Citation11,Citation22
Indications for the treatment of capillary hemangiomas in the periocular region are ptosis with visual axis occlusion, deprivational amblyopia, anisometropia, and cosmesis.Citation7 Similar to the observations by Schwartz et al,Citation2 four of our patients with upper-eyelid lesions, with basal dimensions measuring >1 cm, developed amblyopia secondary to anisometropia and mechanical ptosis that occluded the visual axis.
Refractive errors are potentially reversible, especially when spectacle correction and prompt amblyopia therapy are given. However, our study could not correlate this thoroughly, due to missing data and a small sample size.
Observation remains an option in the management of hemangiomas. More than half of our patients in this study were monitored closely for any change in refractive error, and were treated for ambylopia when it was present.
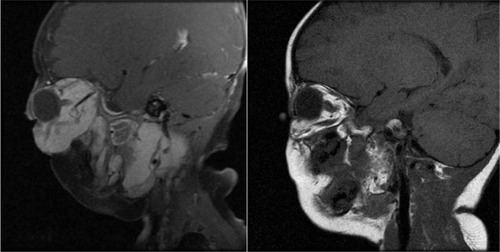
Some of our patients received both local and systemic treatments. Oral prednisolone was commonly prescribed as a systemic treatment for extensive lesions, and we likewise observed regression in the size of the hemangioma (1/2) ().
Figure 4 Sagittal MRI of a hemangioma involving the left orbit and pterygopalatine fossa before (left) and 1 year after treatment (right) with oral prednisolone.
Intralesional steroid injection was the most common form of treatment in the past for capillary hemangioma.Citation5 Weiss observed a reduction in astigmatism of up to 63% within 1 to 14 months after injection.Citation7 In this series, triamcinolone with betamethasone was used as an additional treatment in a case unresponsive to oral prednisolone.
Generally, small and superficial lesions may be effectively managed with topical or intralesional treatments, while larger and deeper hemangiomas require systemic treatments or a combination thereof.Citation5,Citation13 We previously treated patients having relatively superficial and localized lesions with intralesional steroid injections, while for extensive lesions with deep orbital involvement, this was managed through systemic treatments. When one form of treatment was insufficient for reducing the size of the hemangioma, we used a different modality.
Bleomycin is a sclerosing agent and has been widely used as an anticancer drug. We have no local experience with bleomycin in treating hemangiomas. It is believed to act on infantile hemangiomas by reducing vascular endothelial cell proliferation. Sarihan et al were first to report on its application as an intralesional injection for cutaneous hemangiomas.Citation23,Citation24 They noted extensive fibrosis and spontaneous resolution of hemangiomas. One of our patients received intralesional injections of bleomycin at a different institution, as well as oral propranolol.
In recent years, propranolol has produced encouraging results for capillary hemangioma and has become our preferred treatment. We observed dramatic positive responses (2/3) in our patients, except for one who unfortunately developed a systemic complication and had to terminate the treatment.
Systemic complications can be potentially life threatening; one of our patients developed respiratory distress during propranolol treatment. This clearly shows that careful systemic evaluation and patient selection are crucial prior to treatment and that the patient’s family should be informed of the benefits and risks of the therapy.
Although hospital admission with close observation by pediatricians for possible side effects such as hemodynamic changes (eg, bradycardia, hypoglycemia, and respiratory distress)Citation16,Citation18,Citation20 is recommended, outpatient management has been reported by Haider and coworkers to show favorable responses in more than half of patients, with minor side effects.Citation15 Hence, the multidisciplinary collaboration of cardiologists, pediatricians, dermatologists, and ophthalmologists – with pretreatment workups, such as baseline electrocardiography – should remain standard for either inpatient or outpatient intervention.Citation15,Citation16,Citation18
Our study showed there was a favorable response to oral propranolol, with dramatic regression (2/3), except for one who developed respiratory distress. Currently, propranolol is our preferred treatment, at a recommended dose of 1–2 mg/kg/day, given on an outpatient basis when the patient is in good health, or when admitted if otherwise.
To date, several studies have been conducted attesting the efficacy of this nonselective beta-blocker, which has long been used as an antihypertensive agent. It has been speculated that the apparent vasoconstriction may be due to the inhibition of vascular endothelial growth factor and the triggering of endothelial cell apoptosis. In vitro pharmacologic research has shown that propranolol beta adrenergic blockade inhibits several steps in the angiogenic cascade, such as growth factor-induced migration, tubulogenesis, and matrix metalloproteinase secretion of endothelial cells.Citation25
Surgical excision, either complete or partial resection, remains an option for treatment. It is often indicated for sight-threatening hemangiomas that do not respond to medical treatments, or for small well-defined lesions that can be removed completely with minimal morbidity.Citation5,Citation12,Citation13
Conclusion
In general, most children with periocular capillary hemangioma do not require treatment, given their natural capacity for spontaneous involution. The preconditions for intervention are rapidly enlarging lesions, visual axis obscuration, significant induced astigmatism, and cosmetic reasons. For extensive lesions involving the visual axis, local and systemic treatments effectively reduce the size of the lesion, whether they are used alone or in a combination. We recommend systemic treatments such as propranolol for large and deep subcutaneous lesions, especially when these cause visual occlusion, significant refractive error, and globe displacement. Pretreatment, systemic evaluation should be done. Observation is appropriate for small and non-visually threatening hemangiomas. Visual outcomes are generally good when appropriate treatment is given early and existing refractive errors and ambylopia are corrected, which remain of utmost importance. Despite the effectiveness of each treatment, complications exist, and though not frequent, prudence dictates awareness and timely management.
Acknowledgment
We would like to extend our thanks to the following for their contributions in making the completion of this research possible: Dr Sonal Farzavandi, for her support; the eye clinic staff of Kandang Kerbau Women’s and Children’s Hospital, Singapore, for their assistance in the collection of data; and Ms Gian Carla Avendano for her assistance in editing the manuscript.
Disclosure
This paper was originally an Oral Presentation at the Annual European Society of Ophthalmic Plastic and Reconstructive Surgery Meeting, Spazzio Villa Erba, Cernobbio, Italy, September 17, 2011. The authors report no conflicts of interest in this work.
References
- HaikBKarciogluZGordonRAPechousBPCapillary hemangioma (infantile periocular hemangioma)Surv Ophthalmol1994383994268009426
- SchwartzSRBleiFCeislerERisk factors for amblyopia in children with periocular capillary hemangiomas of the eyelid and orbitJ AAPOS20061026226816814181
- FrankRCCowanBJHarropARVisual development in infants: visual complications of periocular hemangiomasJ Plast Reconstr Aesthet Surg2010631819097831
- TambeKMunshiVDewsberryCRelationship of infantile periocular hemangioma depth to growth and regression patternJ AAPOS20091356757020006818
- WassermanBNMedowNBHoma-PalladinoMHoehnMETreatment of periocular capillary hemangiomasJ AAPOS2004817518115088053
- HastingsMMMilotJBarsoum-HomsyMRecombinant interferon alfa-2b in the treatment of vision threatening capillary hemangiomas in childhoodJ Pediatr Ophthalmol Strabismus19971226230
- WeissAHKellyJPReappraisal of astigmatism induced by periocular capillary hemangioma and treatment with intralesional corticosteroid injectionOphthalmology200811539039717588666
- WilsonMWHoehnMEHaikBGLow-dose cyclophosphamide and interferon alfa 2a for the treatment of capillary hemangioma of the orbitOphthalmology20071141007101117337066
- FawcettSLGrantIHallPNVincristine as a treatment for large hemangioma threatening vital functionsBr J Plast Surg20045716817115037175
- ElfleinHMStoffelnsBMPitzSLaser and other treatment options in the therapy of infantile capillary eyelid and periorbital hemangiomas: an overviewMed Laser Appl201025242249
- RootmanJDiseases of the OrbitPhiladelphiaJB Lippincott1988539543
- LeviMSchwartzSBleiFSurgical treatment of capillary hemangiomas causing amblyopiaJ AAPOS200711323023417344079
- MaguinessSMFriedenIJCurrent management of infantile hemangiomasSemin Cutan Med Surg20102910611420579599
- RanchodTMFriedenIJFrederickDRCorticosteroid treatment of periorbital hemangioma of infancy: a review of the evidenceBr J Ophthalmol2005891134113816113367
- HaiderKMPlagerDANeelyDEOutpatient treatment of periocular infantile hemangiomas with propranololJ AAPOS20101425125620603059
- Leaute-LabrezeCDumas de la RoqueEHubicheTPropranolol for severe hemangiomas of infancyN Engl J Med20083582649265418550886
- ElsasFJLewisARTopical treatment of periocular capillary hemangiomaJ Pediatr Ophthalmol Strabismus1994311531567931948
- GuoSNiNTopical treatment for capillary hemangioma of the eyelid using b-blocker solutionArch Ophthalmol2010128225525620142555
- KushnerBJThe treatment of periorbital infantile hemangioma with intralesional corticosteroidPlast Reconstr Surg1985765175244034770
- TabanMGoldbergRAPropranolol for orbital hemangiomaOphthalmology2010117195:e420114117
- JuddCDChapmanPRKochBSheaCJIntracranial hemangiomas associated with PHACE syndromeAJNR Am J Neuroradiol200728252917213418
- Al-MotowaSAChaudhryIAEvaluation and management of periocular capillary hemangioma: a reviewSaudi J Ophthalmol2006203176187
- SarihanHMocanHYildizKA new treatment with bleomycin for complicated cutaneous hemangioma in childrenEur J Pediatr Surg1997731581629241503
- LuoQZhaoFHow to use bleomycin A5 for infantile maxillofacial hemangiomas: clinical evaluation of 82 consecutive casesJ Craniomaxillofac Surg201139748248620675147
- AnnabiBLachambreMPPlouffeKMoumdjianRBeliveauRPropranolol adrenergic blockade inhibits human brain endothelial cells tubulogenesis and matrix metalloproteinase-9 secretionPharmacol Res20096043844519467330