Abstract
Background
Extramacular branch retinal vein occlusion (BRVO) occasionally causes serous macular detachment. We studied the movement of extravasated fluid from BRVO lesions to the submacular space.
Methods
We examined nine eyes from nine patients with serous retinal detachment caused by extramacular BRVO. In addition to a comprehensive ophthalmic examination, optical coherence tomography was performed in all nine eyes. Six of the patients also underwent fluorescein angiography.
Results
Visual acuity ranged from 0.03 to 0.9 (median 0.5). All nine eyes showed localized macular detachment and retinal edema which extended from the extramacular BRVO to the macula. Fluorescein angiography revealed dye leakage in the extramacular area but no macular leakage in the six eyes examined. Optical coherence tomography revealed serous retinal detachment in the macula and intraretinal swelling, with low reflectivity in the outer retina extending from the distant BRVO toward the detached macula in all nine eyes. Six eyes were treated with laser photocoagulation, covering the entire area of BRVO, and the other three eyes were treated with intravitreal bevacizumab. Serous retinal detachment and retinal swelling resolved within 3 months of treatment in all nine eyes.
Conclusion
Distant retinal vascular leakage appears to diffuse through the outer retina to the macula, then permeate into the subretinal space.
Introduction
Macular edema is the most common cause of visual impairment in branch retinal vein occlusion (BRVO). Recently, studies using optical coherence tomography (OCT) have revealed various morphological changes associated with macular edema, including sponge-like retinal swelling, cystic changes, and serous retinal detachment.Citation1–Citation3 Serous retinal detachment is reported to be present in 15%–30% of patients with diabetic macular edemaCitation1,Citation4,Citation5 and in 15%–80.8% of patients with BRVO.Citation6–Citation8 Although fluid leakage from permeable macular vessels usually causes macular edema when the distribution of BRVO involves the macula, Finkelstein and Patz reported a distant effect of peripheral BRVO on the macula.Citation9 We previously reported that the tomographic features of macular edema secondary to distant vascular disorders were caused by serous retinal detachment with slight retinal swelling.Citation10 In that report, we speculated that the subretinal fluid in the macular area appeared to originate from a distant retinal vascular leakage because fluorescein angiography results revealed dye leakage in the extramacular area but not the macular area. Although there have been some reports about macular edema from distant BRVO,Citation11,Citation12 the pathogenesis remains unclear. In the present study, we investigated the tomographic changes involved in macular edema secondary to peripheral BRVO (not involving the macula) to elucidate the mechanisms of fluid movement from extramacular permeable lesions to the subretinal space at the fovea.
Materials and methods
We retrospectively studied nine eyes from nine patients (three male and six female; median age 69 [range 49–81] years) who were followed up in our department between July 2003 and April 2012. The follow-up periods ranged from 6 to 24 (median 14) months. This retrospective study was approved by our institutional review board. We defined extramacular BRVO as occluded vessels that did not involve the macular area (5.5 mm in diameter). Inclusion criteria for this study were eyes with serous retinal detachment secondary to extramacular BRVO and a follow-up period of more than 6 months. Exclusion criteria were eyes with poor quality OCT images, serous retinal detachment caused by other etiologies, such as diabetic retinopathy, uveitis, and vitreoretinal interface disease, a history of laser photocoagulation or vitrectomy, and dense media opacity such as cataract or vitreous hemorrhage. In addition to a comprehensive ophthalmic examination, including best-corrected visual acuity, slit-lamp examination, and indirect ophthalmoscopy, time-domain or spectral-domain OCT (Stratus OCT, Cirrus HD-OCT, Carl Zeiss Meditec Inc, Dublin, CA; or Spectralis HRA/OCT, Heidelberg Engineering, Heidelberg, Germany) was performed. Six of the patients also underwent fluorescein angiography. For the OCT examination, vertical and horizontal scans (5–8 mm in length) centered on the fovea were obtained to measure the thickness of the fovea and the subretinal space. We defined foveal thickness as the distance between the inner retinal surface and the retinal pigment epithelium at the central fovea, which included the serous retinal detachment. The thickness of the subretinal space was defined as the distance between the outer surface of the detached retina and the retinal pigment epithelium at the central fovea. In six of nine eyes, laser photocoagulation was applied to the entire area of BRVO within 2 weeks of the initial examination. The other three eyes were treated with intravitreal injection of 1.25 mg bevacizumab (Avastin®, Genentech Inc, San Francisco, CA) within 2 weeks of the first examination.
Results
The clinical characteristics of the patients are summarized in . At the time of initial examination, visual acuity ranged from 0.03 to 0.9 (median 0.5). All nine eyes showed localized macular detachment and retinal edema which extended from extramacular BRVO to the macula. The site of occlusion was along the inferior vascular arcade in four eyes, along the superior vascular arcade in two eyes (), superonasal to the optic disk in two eyes (), and inferonasal to the optic disk in one eye (). In four eyes, hard exudates were seen in the macula ( and ). Fluorescein angiography in six eyes revealed dye leakage in the extramacular area but no macular leakage ( and ). Widespread nonperfusion of the retinal capillary bed was observed in three of six eyes (). In all nine eyes, OCT showed serous retinal detachment in the macula and outer retinal swelling of low reflectivity extending from the distant permeable lesions toward the fovea (, , and ). On the other side across the fovea, slight retinal swelling was seen in the macula in three eyes, but no retinal swelling was found in the other six eyes. Foveal thickness was 280–575 μm (median 425 μm). The thickness of the subretinal space was 145–373 μm (median 240 μm). After treatment, serous retinal detachment and retinal swelling were resolved within 3 months in all nine eyes.
Figure 1 A 49-year-old man (patient 9) with a branch retinal vein occlusion had a 4-week history of blurred vision in his left eye. Best-corrected visual acuity was 0.5. (A) Fundus photograph shows serous macular detachment, hard exudates, and flame-shaped hemorrhages extending from the superior retinal vascular arcade to the superotemporal mid peripheral fundus. The vertical arrow indicates optical coherence tomography scanning lines (8 mm). (B) In the late phase of the fluorescein angiogram, there is marked hyperfluorescence of the superior retinal vascular arcade but no dye leakage in the macular area. (C) A vertical optical coherence tomography scan shows serous retinal detachment at the fovea and outer retinal swelling, which is evident superior to the fovea (arrow).
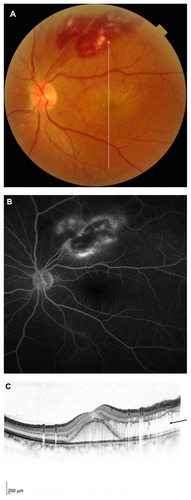
Figure 2 A 72-year-old woman (patient 8) with a branch retinal vein occlusion had a 2-month history of blurred vision in her right eye. Best-corrected visual acuity was 0.15. (A) Fundus photograph shows serous macular detachment and hard exudates. The horizontal arrow indicates optical coherence tomography scanning lines (6 mm). (B) Fluorescein angiogram reveals dye leakage from retinal vessels and a large area of capillary nonperfusion extending from the optic disk to the superonasal mid peripheral fundus but no dye leakage in the macular area. (C) A horizontal optical coherence tomography scan shows a serous retinal detachment at the fovea and outer retinal swelling, which is evident nasal to the fovea (arrow) and hard exudates (arrow heads).
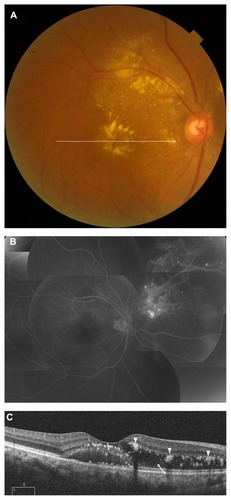
Figure 3 A 74-year-old woman (patient 7) with a branch retinal vein occlusion had a 2-week history of blurred vision in her left eye. Best-corrected visual acuity was 0.9. (A) Fundus photograph shows serous macular detachment and a part of the flame-shaped hemorrhages extending from the optic disk to the inferonasal midperipheral fundus. The horizontal arrow indicates optical coherence tomography scanning lines (6 mm). (B) A horizontal optical coherence tomography scan shows a serous retinal detachment at the fovea and outer retinal swelling, which is evident nasal to the fovea (arrow).
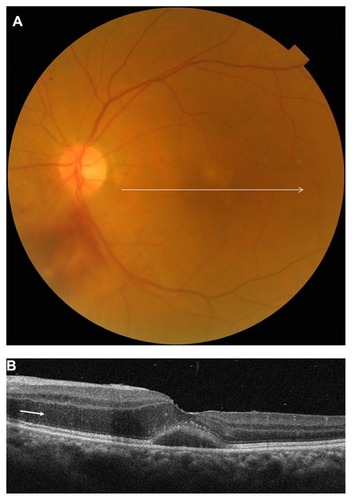
Table 1 Clinical profiles of the patients
Discussion
We examined nine patients with a serous macular detachment secondary to an extramacular BRVO. Fluorescein angiography, performed in six of the nine patients, revealed dye leakage in the extramacular area but not in the macular area. OCT revealed serous retinal detachment in the macula, as well as outer retinal swelling. Importantly, our results demonstrated that retinal swelling extended from the extramacular BRVO toward the fovea.
Retinal swelling and cystoid macular edema are usually caused by leakage from retinal vessels, such as in retinal vascular disease and uveitis. Subretinal fluid can also cause structural changes in the detached neurosensory retina.Citation13 OCT analysis of rhegmatogenous retinal detachment showed intraretinal cyst formation, intraretinal separation, and undulation of the outer detached retina.Citation13,Citation14 In the acute phase of central serous chorioretinopathy, the neurosensory retina is thickened within the area of serous retinal detachment.Citation15 As such, it was previously thought that intraretinal edema was a secondary change in serous retinal detachment caused by distant BRVO, and that the subretinal fluid in the macula originated from distant retinal vascular leakage through the subretinal space.Citation10 However, in the present study, OCT revealed that outer retinal swelling was present not only in the detached retina but also in the attached retina, extending from extramacular permeable lesions toward the fovea. These findings suggest the possibility that distant retinal vascular leakage diffuses through the outer retina to the macula and accumulates there. These accumulations may exude from the intraretinal tissue to the subretinal space at the fovea.
Wise and Wangvivat proposed that the macula has an exaggerated pathological response to some generalized retinal disorders, such as retinal vein occlusion, angioid streaks, uveitis, diabetic retinopathy, and Coats’ disease.Citation16 We found that although outer retinal swelling was identified between extramacular lesions and the fovea, it was seldom observed on the other side of the fovea. This indicates that intraretinal leakage tends to accumulate toward the macula, which may constitute an exaggerated macular response. Yamaguchi et al reported that the incidence of serous retinal detachment was higher in a group with major BRVO (defined as BRVO involving a large area outside the vascular arcade in addition to the macular area) than in a group with macular BRVO (defined as BRVO in which retinal hemorrhage is confined within the major vascular arcade) and that foveal thickness in individuals with major BRVO (mean of 610 μm) was significantly greater than that in individuals with macular BRVO (mean of 500 μm).Citation6 This also indicates that vascular leakage from congested retinal veins outside the macular area is related to retinal swelling and subretinal fluid accumulation in the macula. Although the reason for this exaggerated macular response is unclear, Naumann and Apple proposed the following factors as partially responsible for the occurrence of this phenomenon: increased thickness of the sensory retina in the perifoveal region; special orientation of the fibers of the outer plexiform layer in this region, forming Henle’s fiber layer; high content of melanin within retinal pigment epithelial cells in this region; and high concentration of retinal pigment epithelial cells at the posterior pole.Citation17
An increased vascular endothelial growth factor level may also cause serous retinal detachment in the macula and outer retinal swelling, because fluorescein angiography showed widespread nonperfusion of the retinal capillary bed in three of six eyes examined. In addition, the fact that serous retinal detachment and outer retinal swelling resolved after laser photocoagulation or intravitreal injection of bevacizumab suggests involvement of vascular endothelial growth factor. However, it is unlikely that macular vessels were directly affected by vascular endothelial growth factor because fluorescein angiography showed no macular leakage. In conclusion, distant retinal vascular leakage seems to diffuse through the outer retina to the macula and permeate into the subretinal space.
Disclosure
The authors report no proprietary interest in any aspect of this work.
References
- OtaniTKishiSMaruyamaYPatterns of diabetic macular edema with optical coherence tomographyAm J Ophthalmol1999127668869310372879
- SpaideRFLeeJKKlancnikJKJrGrossNEOptical coherence tomography of branch retinal vein occlusionRetina200323334334712824834
- GaucherDSebahCErginayAOptical coherence tomography features during the evolution of serous retinal detachment in patients with diabetic macular edemaAm J Ophthalmol2008145228929618054885
- CatierATadayoniRPaquesMCharacterization of macular edema from various etiologies by optical coherence tomographyAm J Ophthalmol2005140220020615992752
- OzdemirHKaracorluMKaracorluSSerous macular detachment in diabetic cystoid macular oedemaActa Ophthalmol Scand2005831636615715559
- YamaguchiYOtaniTKishiSSerous macular detachment in branch retinal vein occlusionRetina20062691029103317151490
- ShroffDMehtaDKAroraRNarulaRChauhanDNatural history of macular status in recent-onset branch retinal vein occlusion: an optical coherence tomography studyInt Ophthalmol200828426126817668149
- TsujikawaASakamotoAOtaMSerous retinal detachment associated with retinal vein occlusionAm J Ophthalmol2010149229130120103055
- FinkelsteinDPatzADistant effect of peripheral branch vein occlusion on the maculaTrans Am Ophthalmol Soc1988863803882979024
- OtaniTYamaguchiYKishiSSerous macular detachment secondary to distant retinal vascular disordersRetina200424575876215492631
- TakiWOohiraAHirakataAMacular edema from distant branch retinal vein occlusion improved after vitrectomyJpn J Ophthalmol200953218418619333707
- UedaTGomiFSuzukiMUsefulness of indocyanine green angiography to depict the distant retinal vascular anomalies associated with branch retinal vein occlusion causing serous macular detachmentRetina201232230831321869614
- HagimuraNSutoKIidaTKishiSOptical coherence tomography of the neurosensory retina in rhegmatogenous retinal detachmentAm J Ophthalmol2000129218619010682971
- LeeSYJoeSGKimJGChungHYoonYHOptical coherence tomography evaluation of detached macula from rhegmatogenous retinal detachment and central serous chorioretinopathyAm J Ophthalmol200814561071107618374302
- IidaTHagimuraNSatoTKishiSEvaluation of central serous chorioretinopathy with optical coherence tomographyAm J Ophthalmol20001291162010653407
- WiseGNWangvivatYThe exaggerated macular response to retinal diseaseAm J Ophthalmol1966615 Pt 2135913635938021
- NaumannGOHAppleDJPathology of the EyeNew York, NYSpringer-Verlag1980