Abstract
Background
The purpose of this study was to examine patient characteristics and outcomes in a group of consecutive patients with ruptured globe eye injuries at Kings County Hospital Center, a large, urban, level 1 trauma center.
Methods
A retrospective chart review was performed to identify all patients with ruptured globe eye injuries seen between January 2009 and October 2011. Thirty-eight patients who sustained ruptured globe eye injuries from all causes were investigated for etiology and final visual outcomes
Results
Eight eyes in which vision could be assessed were evaluated as having no light perception at presentation and three of these eyes required primary enucleation. Of the 38 eyes, orbit fractures were found in 15 eyes and an intraocular foreign body was found in six eyes.
Discussion
Our cohort revealed a 37.5% rate of primary enucleation in eyes with no light perception, which we believe to be a reflection of the severity of injury. All three cases were secondary to a gunshot wound. Further, our sample, although small in size, revealed a very high percentage of eyes that were ruptured secondary to violent causes compared with other studies.
Introduction
Ocular trauma remains a major cause of visual impairment in the US nationally. Injuries occur with a broad range of severity and include simple subconjunctival injury, lid laceration, corneal abrasion, traumatic iritis, hyphema, lens injury, vitreous hemorrhage, retinal detachment, traumatic optic neuropathy, retrobulbar hemorrhage, orbit fracture, and ruptured globes. Ruptured globes represent one of the more serious consequences of trauma and often lead to some degree of permanent visual loss.
Kings County Hospital Center differs from other communities where case series on ocular trauma have been published in that previous studies have been focused specifically on the elderly,Citation1 occurred in primarily Asian populations,Citation2 or drawn patients from areas that were much less densely populated than Brooklyn.Citation3 Traumatic injury to the eye in the US occurs at an incidence approaching 2.5 million per year. While estimates by the National Society to Prevent Blindness suggest that 90% of these injuries are preventable, both the number and causes of these injuries remain remarkably stable.
Large population series have demonstrated that, on an epidemiological scale, there are known factors that increase the risk of ocular trauma. In an analysis of blinding trauma from the US Eye Injury Registry containing data for 11,320 eyes, Kuhn et alCitation4 elucidated the risk factors leading to blindness as being age over 60 years, injury by assault, injuries sustained on a street or highway, and trauma from fall injuries and gunshot wounds. They also noted posterior eye injury as a causative risk factor for blindness.
Another series of patients reported at a single hospital found that postoperative endophthalmitis after open globe injury occurred at a rate of 6.8%, and found that delays in primary repair greater than 24 hours, a ruptured lens capsule, and wounds presenting with protein or soil contaminants were each independently associated with the development of post-traumatic endophthalmitis, with the risk being even greater when two or more of these criteria were present.Citation5,Citation6 The present study was undertaken to evaluate the epidemiology of traumatic ruptured globes at Kings County Hospital Center, a level 1 trauma center located in an urban area serving the majority of Kings County in Brooklyn, NY, USA.
Materials and methods
This project focused specifically on ruptured globe repairs that occurred between January 1, 2009 and October 30, 2011. A retrospective review of the operating room logbook identified 39 ruptured globe repair surgeries performed at Kings County Hospital Center during this time period using the Birmingham Eye Trauma Terminology System criteria.Citation7 Exclusion criteria eliminated one patient with Fuchs’ corneal dystrophy. We have adapted the criteria from previous case series to include age, gender, mechanism of injury, zone of injury, time of presentation to the Kings County Hospital Center emergency room, visual acuity before and after surgery, previous ocular surgery, associated bony fracture, and the presence of a foreign body within the globe. Complications during care and postoperatively were also investigated.
While previous studies have been performed using surveys and registry dataCitation4 and have examined the elderlyCitation1 or focused on rupture after keratoplasty,Citation8 we could not find any articles examining this type of injury in a large urban setting with a predominantly African American/Afro-Caribbean population. Given the size and diversity of the patient population served by Kings County Hospital Center, this series would add valuable information to the trauma literature. The data gathered are also compared with data from the most recent American Academy of Ophthalmology Eye Injury Snapshot Project.Citation9 The study was approved by the institutional review board at SUNY Downstate Medical Center and Kings County Hospital Center.
Results
Our study sample included 38 eyes representing 38 individual patients, with 31 (81.5%) being male. At the time of presentation, the average patient age was 36 years, with the oldest being 92 years and the youngest being 3 years. Patients over 65 years of age accounted for three of the 38 cases (7.8%), and two (5.26%) were children under the age of 12 years. The mechanism of injury was identified to be violent in 19 (50%) of the 38 cases, with seven of those 19 (36.8%) resulting from gunshot wounds. Other violent means of injury included bottles to the eye (n = 2), a baseball bat to the eye (n = 1), and a hammer (n = 1).
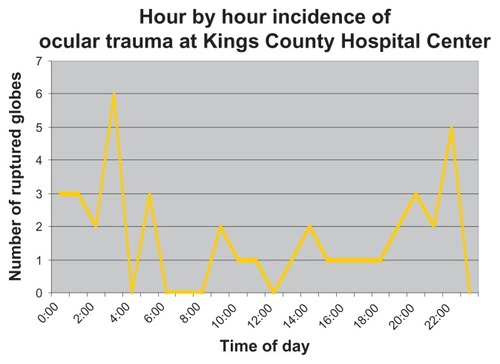
The time of emergency department triage was also recorded, and of 33 patients for whom data were available (transfer patients were excluded from this measure), 17 of 33 cases (51%) presented between the hours of 8 pm and 4 am.
Reporting of wounds involving the eye was standardized to the Birmingham Eye Trauma Terminology SystemCitation7 which has been adopted by major eye organizations worldwide. Ruptured globes fall into the category of open globe injuries, which are injuries resulting in a full-thickness laceration of the cornea and/or sclera. Wounds can be penetrating (with one entry wound and no exit wound),or perforating (a through-and-through injury with both entrance and exit wounds).
Eye injuries are also divided into zones based on anatomical location. Based on the Birmingham Eye Trauma Terminology System, zone I wounds are limited to the cornea and limbus, zone II if they involve the anterior sclera within 5 mm of the limbus, and zone III if they involve the sclera 5 mm posterior from the limbus. The zone of eye injury was determined by examining the operative report of the globe repair, and eyes were grouped according to the above classification into zones I, II, or III (5, 14, and 19 eyes, respectively).
The extent of visual impairment at initial presentation varied greatly in our case series, ranging from normal vision (20/20) to no light perception, with three patients unable to be assessed because of intubation and one patient being uncooperative. Of the 34 remaining patients in whom vision could be assessed, eight presented with no light perception (23.5%), of whom three had a primary enucleation and one had a secondary enucleation. A secondary enucleation was performed in a patient who possessed better than NLP vision at presentation, for a total of five enucleations in the patients studied.
Post-repair complications were also examined. Complications were broken into segments anatomically, ie, corneal, anterior chamber, and retinal. Corneal complications ranged from pyogenic granuloma to an exposure keratopathy eventually requiring a transplant, and the total injuries in this category accounted for 15% of patients. Anterior chamber complications were seen at a rate of 20.5%, and included traumatic recession of the angle, pigment dispersion, and iris irregularities. Retinal complications/reoperations occurred at a rate of 25.6%. Patients were seen to have multiple segment complications on 12.8% of occasions. There was one instance of sympathetic ophthalmia, which occurred 6 weeks after the ruptured globe was repaired in an eye with an initial visual acuity of hand motion; the patient was immediately started on appropriate immunosuppressant therapy (mycophenolate mofetil), but thus far has declined enucleation.
Data for admission via the emergency department were also investigated. The majority of patients (51%) presenting to the emergency department with severe ocular trauma did so between the hours of 8 pm and 4 am (), a time period during which the fewest hospital personnel are available.
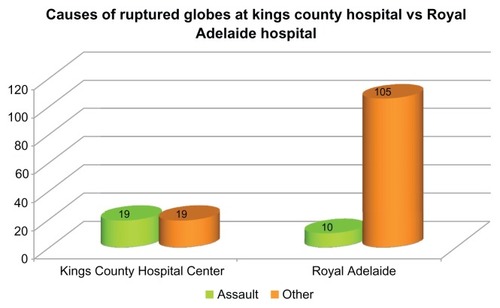
Figure 1 Using data from Casson et al,Citation3 we compared data on the causes of ruptured globes from Kings County, a major urban hospital, to data from the Royal Adelaide Hospital, a hospital in Australia that covers both urban and rural areas.
Discussion
Ruptured globes represent one of the most serious surgical eye emergencies. Outcomes can vary from no change in visual acuity, to a blind painful eye that requires enucleation in order to prevent sympathetic ophthalmia or endophthalmitis. A number of conclusions can be drawn from this retrospective review of patient data from Kings County Hospital Center.
Kings County Hospital Center serves as the main level 1 trauma center in Brooklyn, a borough of New York City with a population that exceeds 2.5 million people. The average age of our patients was 36 years, with an overwhelming majority being African-American or Afro-Caribbean males. This is different from the demographics of Brooklyn as a whole (36.1% African-American or Afro-Caribbean, with an average age of 34.1 years). The population is in line with the areas closest to Kings County Hospital Center,Citation10 and represents a community under-represented in the medical literature.
There is no clear consensus as to the management of eyes with no light perception, although prognostic indicators have been examined previously.Citation2 It is reasonable to consider the factors behind Kings County Hospital Center operative data on eyes with no light perception as causing a rate of 37.5% for primary enucleation and a rate of 50% for eyes with no light perception being enucleated overall. Of the eight eyes that had no light perception on presentation, seven were as a direct result of intentional harm, and were traumatized beyond the ability to reconstruct a useful functional eye. Further, the issue of enucleation in a blind eye is underscored by our one case of sympathetic ophthalmia, an exceedingly rare and dangerous condition affecting the fellow eye after trauma. There may be some benefit from the strategy reported by Savar et al,Citation11 whereby patients were made appointments for one week and one month after discharge, with the opportunity to come in as needed in between. Our Kings County Hospital Center average no-show rate for return visits for all clinic appointments versus that for ruptured globes has not been determined, and perhaps an extensive conversation with patients detailing the risks and benefits of enucleation would improve no-show rates. A recent article by Soni et alCitation12 looking at 73 eyes with open globe ocular trauma that presented with no light perception found that zone III injuries were most likely to develop no light perception and also that eyes that had some recovery at day 1 postoperatively had better final visual acuity.
Current recommendations indicate that primary repair of the globe is most beneficial when performed within the first 24 hours and may even be protective against endophthalmitis. While this review did not assess time from injury to the operating room, the knowledge that time is a predictive factor for the prognosis of ruptured globe injury necessitates an efficient method of diagnosis and triaging of injuries, especially those that occur on overnight shifts when human resources are at their lowest. Further, patients who are sent as transfers from other institutions are subject to much longer delays in transport and triage before being seen by a consulting ophthalmologist. Standardizing the data points necessary for diagnosis could help eliminate some of those delays.
In comparing our causes of injury with those from the American Academy of Ophthalmology’s Eye Injury Snapshot, our incidence of a firearm injury as the etiologic factor was 18.4% as compared with snapshot data for all traumatic injuries which reports firearm injuries to account for 1.9%. Of course the number of violent injuries we saw in our small cohort of 38 patients represents only a small percentage of the total number of emergency injuries we see from all acute emergency department visits, given that many traumas do not cause a ruptured globe. Brooklyn currently has seen the highest number of homicides and shootings in New York City in 2012,Citation13 and clearly our ophthalmology service is treating only a minority of those patients wounded or killed because many may sustain injuries at body sites not involving the eye. It is of note nonetheless that violent purposeful trauma was the cause of ruptured globe injuries in 50% of our patients, with seven of our 38 patients sustaining a gunshot wound. In comparison with a study of patients treated at the Royal Adelaide HospitalCitation3 which examined 109 patients over 4 years, the reported rate of assault as a causative factor in ruptured globes was 9.17%, which was confirmed as a statistically significant difference with Fisher’s Exact test (P < 0.0001, ). In the same study, 50.5% of patients were drawn from rural areas, while Brooklyn’s total population density is 13,839 people/km2.
Disclosure
This research was presented as a poster at the annual meeting of the Association of Research in Vision and Ophthalmology in 2012 in Fort Lauderdale, FL, USA. Otherwise, the authors report no conflicts of interest in this work.
References
- AndreoliMAndreoliCGeriatric traumatic open globe injuriesOphthalmology201111815615920709403
- FengKHuYTMaZPrognostic indicators for no light perception after open-globe injury: eye injury vitrectomy studyAm J Ophthalmol201115265466221726850
- CassonRJWalkerJCNewlandHSFour-year review of open eye injuries at the Royal Adelaide HospitalClin Experiment Ophthalmol20023081511885802
- KuhnFMorrisRWitherspoonDEpidemiology of blinding trauma in the United States Eye Injury RegistryOphthalmic Epidemiol20061320921616854775
- EssexRWLamoureuxECharlesPGProphylaxis for posttraumatic endophthalmitisArch Ophthalmol200812674274418474800
- EssexRWYiQCharlesPGPost-traumatic endophthalmitisOphthalmology20041112015202215522366
- KuhnFMorrisRWitherspoonCDBirmingham Eye Trauma Terminology (BETT): terminology and classification of mechanical eye injuriesOphthalmol Clin North Am20021513914312229228
- KawashimaMKawakitaTShummuraSCharacteristics of traumatic globe rupture after keratoplastyOphthalmology20091162072207619766315
- American Academy of OphthalmologyEye injuries: recent data and trends in the United States Available from: http://www.aao.org/newsroom/guide/upload/Eye-Injuries-BkgrnderLongVersFinal-l.pdfAccessed January 26, 2013
- Quickfacts.census.gov [homepage on the internet]Washington DCUS Department of Commerce2011 Available from: http://quickfacts.census.gov/qfd/states/36/36047.htmlAccessed January 14, 2013
- SavarAAndreoliMTKloekCEEnucleation for open globe injuryAm J Ophthalmol200914759560019181305
- SoniNGBauzaAMSonJHLangerPDZarbinMABhagatNOpen globe ocular trauma: functional outcome of eyes with no light perception at initial presentationRetina20133338038623026847
- ParascandolaRPaddockBConnorTCrosshairsNY Daily News201256