 ?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Purpose
Our goal was to evaluate the influence of optic disc size on the progression of visual field damage in patients with normal-tension glaucoma (NTG).
Subjects and methods
Eighty-two eyes of 82 NTG patients who had been receiving topical antiglaucoma medications and followed-up for more than 4 years were enrolled in this study. The patients were allocated to two groups, according to the mean size of their optic discs. The data were analyzed using regression analysis, based on the Cox proportional hazard model.
Results
The probability of visual field stability was significantly lower in eyes with large discs than in those with small discs (log rank test, P = 0.007). Progression of visual field damage was significantly associated with the optic disc area (hazard ratio [HR]: 1.812, P = 0.018), occurrence of disc hemorrhage (HR: 2.116, P = 0.028), and intraocular pressure reduction ratio (HR: 0.957, P = 0.014).
Conclusion
The optic disc area correlates with progression of visual field damage in patients with NTG.
Introduction
Optic disc size is reportedly a possible risk factor for glaucomatous optic nerve damage.Citation1–Citation5 However, some groups have reported no difference in susceptibility between large and small discs.Citation6–Citation11 Thus, the relationship between the size of the optic disc and glaucomatous optic nerve damage is still controversial.
Most previous studies based assessment of optic disc size on fundus photographs. Measurement of optic disc size by planimetry is inaccurate because it is subjective and, therefore, varies among observers. As for the progression of visual field damage, Chauhan et alCitation12 reported that the detection of small gradual changes requires lengthy follow-up. In addition, frequent examinations per year are required for accurate assessment. Thus, both lengthy and frequent follow-ups are necessary to evaluate progressive changes in visual fields accurately. To the best of our knowledge, there are no published clinical reports evaluating the relationship between optic disc size as determined by confocal scanning laser ophthalmoscopy and progression of visual field damage in patients with normal-tension glaucoma (NTG). The purpose of this study was to investigate the relationship between the size of the optic disc and progression of visual field damage in patients with NTG.
Subjects and methods
Subjects
We retrospectively reviewed the records of 313 patients with NTG attending the Glaucoma Clinic of the Department of Ophthalmology, Nihon University Hospital, to identify patients suitable for inclusion in this study. We defined NTG as normal open angle; peak intraocular pressure (IOP) ≤21 mmHg at all times, including 24-hour phasing; presence of typical glaucomatous visual field damage associated with glaucomatous optic nerve changes; and the presence of optic neuropathy not attributable to other ocular or systemic disease.Citation13 The Ethics Review Committee of the Nihon University School of Medicine approved the protocol of the study. All patients selected for this study gave written informed consent.
Inclusion criteria
From 313 patients with NTG whose records we reviewed, we selected patients for further assessment according to the following criteria: (1) best-corrected visual acuity ≥ 20/25 at the beginning and end of the follow-up period; (2) spherical equivalent ≥ −6 diopters; (3) no history of intraocular or laser surgery; (4) no tilted disc and vertical/horizontal ratio of the optic disc < 6/5; (5) initial mean deviation of −20 dB or better; and (6) a follow-up period of at least 4 years after the diagnosis with reliable results of the visual field examinations at least nine times in addition to the initial examination. If the patient had undergone surgical treatment, we analyzed only the preoperative data. When both eyes of a patient met the above criteria, we selected the findings for the right eye. We included 82 eyes of 82 NTG patients in the current study.
Ophthalmic examinations
After washing out topical antiglaucoma medications for 4 weeks, all enrolled patients were hospitalized to undergo testing for diurnal IOP variations with a Goldmann applanation tonometer (Haag-Streit, Koeniz, Switzerland). We took IOP measurements every 2 hours from 06.00 to 24.00 hours. Ophthalmological examinations included assessment of refraction, axial-length, central corneal thickness, and visual field examinations using the central 30-2 program with the Humphrey Field Analyzer (HFA 30-2; Carl Zeiss Meditec, Dublin, CA, USA). The criteria for a reliable visual field examination were ≤33% for both false-positive and false-negative findings and <20% for fixation loss. We took optic disc stereo photographs with a stereo fundus camera (3-DX, NIDEK, Gamagori, Japan) and performed three-dimensional topographic analysis of the optic disc with a Heidelberg Retina Tomograph (HRT) (HRT version 2.01; Heidelberg Engineering GmbH, Heidelberg, Germany) when appropriate. We constructed mean topographic images obtained from more than five images using the HRT. While viewing the optic disc stereo photograph, two experienced operators (YY, FH) drew the contour line of the optic disc margin at the inner edge of the scleral ring on the HRT screen using a computer mouse. The mean HRT topographic images with standard deviation < 40 μm were used in the present study.
Follow-up
After the above-described initial assessment, all patients visited the clinic for IOP measurement and evaluation of optic disc changes every 8–12 weeks. We performed visual field examinations with the HFA 30-2 program every 6 months.
Criteria for progression of visual field damage
We defined progression of visual field damage according to the criteria of the Collaborative Normal Tension Glaucoma Study Group (CNTGS).Citation14 These criteria are as follows: (1) two or more points that have deteriorated by at least 10 dB from the average baseline values for those points. These two progressing points must be adjacent, both cannot be peripheral, and they are not to cross the nasal meridian; and (2) at least one of the innermost four points shows at least a 10 dB deterioration from the average baseline value. We considered progression to be confirmed when four of five consecutive follow-up fields showed progression relative to baseline fields, with at least one nonperipheral progressing point (or the one central point) being common to all four fields.
Analysis of findings
We divided the enrolled subjects into two groups, according to the mean size of their optic discs as assessed by HRT. We compared the clinical background data of patients’ eyes with small versus large disc areas and of those with progressive versus without progressive visual field damage. We also compared visual field stability in the two groups using the Kaplan–Meier life-table analysis.
In addition, we analyzed the influence of various clinical factors on the progression of visual field damage by regression analysis of patient data based on the Cox proportional hazards model. The factors thus analyzed included patient age, sex, mean deviation, and corrected pattern standard deviation, refraction, central corneal thickness, axial length, disc size, occurrence of disc hemorrhage (DH), combination of antiglaucoma agents, mean IOP of diurnal variation, mean IOP during follow-up, and the IOP reduction ratio. We defined the IOP reduction ratio as:
Differences between the means were considered to be significant at P < 0.05, determined using the Statistical Package for the Social Sciences 17.0 (SPSS, IBM Corporation, Armonk, NY, USA). We did not evaluate details of compliance with medications.
Results
shows the clinical background data. Because the mean optic disc area as determined by HRT was 2.41 mm2 overall, we set the cut-off value for optic disc area at 2.41 mm2. shows the distribution curve of the optic disc area of the 82 eyes. The mean value for optic disc area in this study corresponded to previously reported values for normal eyes.Citation15,Citation16 The mean follow-up time for all patients was 103 ± 30 months (mean ± standard deviation). Of the 82 patients enrolled in this study, 43 reached the end-point during follow-up, and the probability of visual field stability was 47% ± 6% in all patients.
Figure 1 Distribution of optic disc area for all subjects.
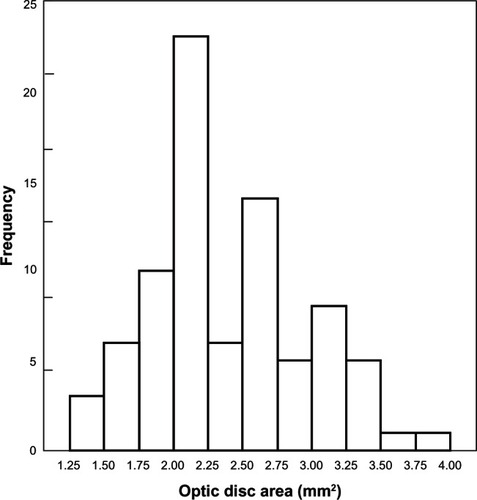
Table 1 Clinical data for all enrolled subjects (n = 82)
We divided the 82 enrolled patients into the following two groups, according to the mean optic disc area (2.41 mm2); 38 patients with large discs and 44 with small discs. shows clinical background data for eyes with large versus small disc areas. There were no statistically significant differences in these data apart from optic disc area. There were no significant differences in the number of patients receiving topical antiglaucoma medications during follow-up. Of the 38 eyes with large disc areas, 26 (68%) showed progression of visual field damage and 12 (32%), no progression. Of the 44 eyes with a small disc area, 17 (39%) showed progression of visual field damage, whereas 27 (61%) showed no progression. shows the Kaplan-Meier curve for the probability of visual field stability. The probability of visual field stability was 36% ± 8% for eyes with large disc areas and 56% ± 8% for those with small disc areas. There was a statistically significant difference in the probability of visual field stability between eyes with large versus small disc areas (log rank test, P = 0.007).
Figure 2 The probability of visual field stability, according to optic disc size.
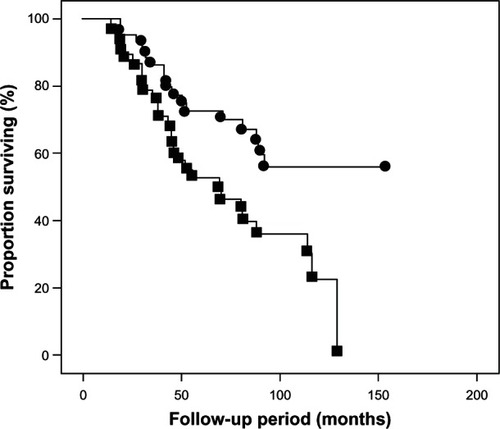
Table 2 Clinical data for eyes with large versus small discs
shows clinical background data for eyes with and without progressive visual field damage. There were statistically significant differences in the sizes of the disc areas (P = 0.009, unpaired Student’s t-test) and occurrence of DH (P = 0.010, Fisher’s exact test). There were no significant differences in the number of patients receiving topical antiglaucoma medications during follow-up.
Table 3 Clinical data for eyes with and without progressive visual field damage
In the 82 eyes in this study, the Cox proportional hazards model indicated that the optic disc areas (hazard ratio [HR]: 1.812, P = 0.018), occurrence of DH (HR: 2.116, P = 0.028), and IOP reduction ratio (HR: 0.957, P = 0.014) were significantly correlated with progression of visual field damage ().
Table 4 Factors identified as associated with progression of visual field damage in patients with NTG (n = 82)
Discussion
Our study demonstrated that eyes with large disc areas have a significantly greater incidence of progressive visual field defects than do those with small disc areas. This finding suggests that large optic discs within the normal range of IOP are susceptible to glaucomatous damage, in accordance with previous reports.Citation13 Nesterov and Egorov documented that the size of the optic disc has a sensitive relationship with IOP, because the lamina cribrosa has a multilayer spring system.Citation17 Recently, researchers reported that eyes with NTG have a significantly thinner lamina cribrosa than do those with primary open-angle glaucoma and matched visual field defects as assessed by the enhanced depth-imaging mode of optical coherence tomographyCitation18 These findings suggest that large optic discs are structurally weak. This may increase their susceptibility for the development of glaucomatous damage at any given level of IOP.
Based on the membrane theory of a mathematical model, Chi et alCitation19 reported that the lamina cribrosa of large discs undergoes significant displacement in the presence of a high IOP. Bellezza et alCitation20 have categorized the optic disc as a biomechanical structure. Their paradigm suggests that mechanical failure of the connective tissue of the lamina cribrosa underlies glaucomatous cupping, and they postulate that larger discs are more susceptible to IOP-related stress, in accordance with Laplace’s law.Citation20 These reports suggest that, in eyes with NTG, the organizational structure of optic discs determines their susceptibility to increased IOP. Because larger optic discs have structures that are more vulnerable to the deleterious effects of increased IOP, they are more susceptible to glaucomatous optic neuropathy.
The present study shows that progression of visual field damage correlates significantly with the IOP reduction ratio. IOP is probably the only treatable factor in glaucoma. Many investigators have reported a relationship between increased IOP and the progression of visual field damage. The CNTGSCitation14 demonstrated that the probability of visual field stability at 5 years was 80% in a treated group that had filtering surgery and 35% in an untreated group. Our study showed that the probability of visual field stability is 63% at 60 months and 47% at 103 months in patients receiving topical antiglaucoma medication. Thus, topical medication to reduce IOP is useful for preventing progression of visual field damage, even though the IOP reduction it achieves is not as great as that following filtration surgery.
Occurrence of DH is a well known predictor of progression of visual field damage in patients with NTG.Citation21–Citation23 The precise mechanism of DH has not been determined; however, it may result from regressive vascular changes after expansion of the width of retinal nerve fiber layer defects.Citation24 Previously, Yamazaki et alCitation13 reported that circulatory factors in the retrobulbar vessels may be associated with worsening of visual field damage in NTG patients. In our study, we found that the occurrence of DH, which may be related to structural weakness or vascular disorders in the lamina cribrosa, correlates significantly with progression of visual field damage. However, we did not clarify the mechanism of DH in this study.
This study has some limitations. First, it is based on retrospective data; however, there were no significant differences in clinical background data, including the severity of visual field damage and IOP levels, between eyes with large and small disc areas during follow-up. Neither were there any differences between eyes with or without progressive visual field damage. Therefore, the size of the optic disc is a determinant of deterioration in glaucomatous optic neuropathy. Second, to obtain reliable data about optic disc configuration using HRT, we excluded patients with highly myopic eyes or oblique discs from this study because their range of refractive error was from −8 D to +4 D.Citation25 In HRT software version 2.01, the reference plane is automatically set at 50 μm posterior to the mean peripapillary retinal height along the contour line at the temporal sector between 350° and 356°. However, because myopic discs are characteristically tilted from the nasal to the temporal side with the nasal margin elevated relative to the temporal margin, it is possible that this choice of reference plane accounts for the decreased capability of the HRT program in eyes with oblique discs.Citation26 Therefore, we excluded highly myopic eyes and those with oblique discs from this study.
In conclusion, the present study revealed that the size of the optic disc is a definite risk factor for visual field deterioration in patients with NTG. Measurement of the optic disc area may be useful for predicting progressive visual field damage in patients with NTG. Further longitudinal studies are needed to investigate the relationship between the optic disc area and the progression of visual field damage in patients with glaucoma.
Disclosure
The authors report no conflicts of interest in this work.
References
- BurkRORohrschneiderKNoackHVölckerHEAre large optic nerve heads susceptible to glaucomatous damage at normal intraocular pressure? A three-dimensional study by laser scanning tomographyGraefes Arch Clin Exp Ophthalmol199223065525601427140
- TomitaGNymanKRaittaCKawamuraMIntraocular asymmetry of optic disc size and its relevance to visual field loss in normal-tension glaucomaGraefes Arch Clin Exp Ophthalmol199423252902968045438
- TuulonenAAiraksinenPJOptic disc size in exfoliative, primary open angle, and low-tension glaucomaArch Ophthalmol199211022112131736870
- HealeyPRMitchellPOptic disc size in open-angle glaucoma: the Blue Mountains Eye StudyAm J Ophthalmol1999128451551710577600
- WangLDamjiKFMungerRIncreased disk size in glaucomatous eyes versus normal eyes in the Reykjavik eye studyAm J Ophthalmol2003135222622812566030
- JonasJBFernandezMCNaumannGOCorrelation of optic disc size to glaucoma susceptibilityOphthalmology19919856756802062501
- JonasJBStürmerJPapastathopoulosKIMeier-GibbsonsFDichtlAOptic disc size and optic nerve damage in normal pressure glaucomaBr J Ophthalmol19957912110211058562544
- ZangwillLMWeinrebRNBeiserJMBaseline topographic optic disc measurements are associated with the development of primary open-angle glaucoma: the Confocal Scanning Laser Ophthalmoscopy Ancillary Study to the Ocular Hypertension Treatment StudyArch Ophthalmol200512391188119716157798
- QuigleyHAVarmaRTielschJMKatzJSommerAGilbertDLThe relationship between optic disc area and open-angle glaucoma: the Baltimore Eye StudyJ Glaucoma19998634735210604292
- JonasJBXuLZhangLWangYWangYOptic disc size in chronic glaucoma: the Beijing eye studyAm J Ophthalmol2006142116817016815273
- JonasJBMartusPHornFKJünemannAKorthMBuddeWMPredictive factors of the optic nerve head for development or progression of glaucomatous visual field lossInvest Ophthalmol Vis Sci20044582613261815277484
- ChauhanBCGarway-HeathDFGoñiFJPractical recommendations for measuring rates of visual field change in glaucomaBr J Ophthalmol200892456957318211935
- YamazakiYDranceSMThe relationship between progression of visual field defects and retrobulbar circulation in patients with glaucomaAm J Ophthalmol199712432872959439354
- [No authors listed]Comparison of glaucomatous progression between untreated patients with normal-tension glaucoma and patients with therapeutically reduced intraocular pressures. Collaborative Normal-Tension Glaucoma StudyAm J Ophthalmol199812644874979780093
- JonasJBNaumannGOHThe optic nerve: its embryology, histology, and morphologyVarmaRSpaethGLParkerKWThe Optic Nerve in GlaucomaPhiladelphia, PALippincott1993326
- UchidaHYamamotoTAraieMTopographic characteristics of the optic nerve head measured with scanning laser tomography in normal Japanese subjectsJpn J Ophthalmol200549646947616365792
- NesterovAPEgorovEAPathological physiology of primary open-angle glaucoma. The optic nerve changesCairnsJEGlaucomaOrlando, FLGrune and Stratton1986369393
- ParkHYJeonSHParkCKEnhanced depth imaging detects lamina cribrosa thickness differences in normal tension glaucoma and primary open-angle glaucomaOphthalmology20121191102022015382
- ChiTRitchRSticklerDPitmanBTsaiCHsiehFYRacial differences in optic nerve head parametersArch Ophthalmol198910768368392730402
- BellezzaAJHartRTBurgoyneCFThe optic nerve head as a biomechanical structure: initial finite element modelingInvest Ophthalmol Vis Sci200041102991300010967056
- IshidaKYamamotoTSugiyamaKKitazawaYDisk hemorrhage is a significantly negative prognostic factor in normal-tension glaucomaAm J Ophthalmol2000129670771410926977
- DranceSAndersonDRSchulzerMCollaborative Normal-Tension Glaucoma Study GroupRisk factors for progression of visual field abnormalities in normal-tension glaucomaAm J Ophthalmol2001131669970811384564
- NakagamiTYamazakiYHayamizuFPrognostic factors for progression of visual field damage in patients with normal-tension glaucomaJpn J Ophthalmol2006501384316453186
- NittaKSugiyamaKHigashideTOhkuboSTanahashiTKitazawaYDoes the enlargement of retinal nerve fiber layer defects relate to disc hemorrhage or progressive visual field loss in normal-tension glaucoma?J Glaucoma201120318919520577114
- LeungCKChengACChongKKOptic disc measurements in myopia with optical coherence tomography and confocal scanning laser ophthalmoscopyInvest Ophthalmol Vis Sci20074873178318317591887
- YamazakiYYoshikawaKKunimatsuSInfluence of myopic disc shape on the diagnostic precision of the Heidelberg Retina TomographJpn J Ophthalmol199943539239710580661