Abstract
A young patient who showed rhegmatogenous retinal detachment with preoperatively undetected retinal break was successfully treated by scleral buckling using a noncontact wide-angle viewing system.
Introduction
Traditionally, rhegmatogenous retinal detachments with undetectable breaks have been managed using circumferential buckling and cryopexy of suspicious areas, providing a success rate of 53%–85%.Citation1–Citation5 Recently, the effectiveness of primary pars plana vitrectomy or combined pars plana vitrectomy and scleral buckling procedures has been reported.Citation6–Citation8 It has been reported that endoscope-assisted vitrectomy seems promising in the management of pseudophakic and aphakic retinal detachments with undetected retinal breaks because of the ability to diagnose retinal breaks.Citation9
Here, the case of a young phakic patient who presented showing rhegmatogenous retinal detachment with an undetected retinal break preoperatively and was successfully treated with scleral buckling using a noncontact wide-angle viewing system is reported.
Case presentation
A 16-year-old Japanese boy was referred to the authors’ clinic with retinal detachment of the right eye. At the time of the first visit to the clinic, the best corrected visual acuity was 0.7, with myopia of 9 D in the right eye. Axial length was 26.95 mm. Intraocular pressure was within the normal range. Slit-lamp examination revealed intact anterior segments.
Fundus examination showed retinal detachment in the two inferior quadrants associated with multiple lattice degenerations and subretinal strands in the right eye. Despite careful fundus examination, retinal breaks could not be identified. The macula remained attached in the right eye. The patient had no history of trauma or atopy.
The patient subsequently underwent repair of the retinal detachment in the right eye with scleral buckling procedure using a noncontact wide-angle viewing system.
Surgical procedures for the right eye
Following conjunctival peritomy 360 degrees around the limbus, four rectus muscles were isolated for encircling buckling. A trocar for a 25-gauge light fiber (Alcon Laboratories, Fort Worth, TX, USA) was placed 4.0 mm behind the limbus at the 8 o’clock position. The noncontact wide-angle viewing system (Resight™; Carl Zeiss Meditec AG, Jena, Germany) was activated after the light fiber was inserted through the trocar and the light was turned on.
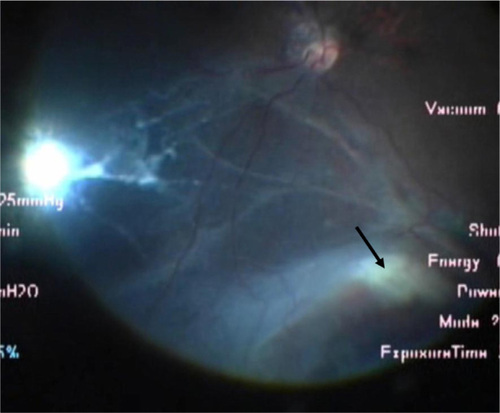
Dynamic scleral compression with a cryoprobe was performed to identify the retinal breaks. A tiny retinal hole was found at the 4 o’clock position (). The retinopexy with cryopexy and diathermy to the break and to the area of lattice degeneration was applied.
Figure 1 Intraoperative view using the wide-angle viewing system.
After the light fiber was pulled off and a plug was inserted into the trocar, the encircling buckling procedure using a silicone tire and belt (numbers 277, 240, and 270; MIRA Inc, Waltham, MA, USA) and external drainage of subretinal fluid through the sclerotomy at the 5 o’clock position were performed under the surgical microscope. The fundus was checked, if necessary, under panoramic view using the noncontact wide-angle viewing system with 25-gauge light fiber during surgery.
No intra- or postoperative complications were encountered. At the 6-month follow-up, the retina remained attached, and best corrected visual acuity was 0.9 in the right eye. The lens showed neither subcapsular opacity nor nuclear sclerosis.
Discussion
In rhegmatogenous retinal detachments, one of the prognostic factors for poor surgical outcomes is the inability to detect retinal breaks. Various strategies, including endoscopic-assisted vitrectomy, have been proposed to manage retinal detachments without detected breaks preoperatively.Citation2,Citation3,Citation6–Citation13
Traditionally, scleral buckling has been considered the procedure of choice for rhegmatogenous retinal detachment in young patients. During scleral buckling procedures, visualization of the fundus is performed using an indirect ophthalmoscope. The image is inverted and small, and cannot be readily shared with medical staff, representing a disadvantage for identifying tiny retinal breaks.
Recently, use of a wide-angle viewing system in vitrectomy surgery has become popular, as this option can easily provide a panoramic view of the surgical field. Two types of the wide-angle viewing system exist, with both contact and noncontact types available. The noncontact type is more popular because of the stability of the image against the tilt of the eyeball and the ease of manipulation. A few reports demonstrated that simultaneous use of a noncontact wide-angle viewing system combined with light fiber illumination for fundus visualization is also feasible for scleral buckling procedures for retinal detachment with preoperatively detected retinal breaks.Citation14,Citation15 The advantages of this method are that the clear images of the retina are directed through the surgical microscope, and can thus be enlarged and seen even with the small pupil. This allows easier detection of retinal breaks using dynamic scleral compression with a cryoprobe under the wide-angle viewing system. In this system, all procedures of scleral buckling can be performed under surgical microscopy, improving the ease of operation for surgeons with refractive errors, especially presbyopia. Images of the fundus can be shared during retinopexy, which will undoubtedly prove useful in surgical education.
Caution should be taken due to the possible risks of surgical complications including vitreous wick from the scleral wound, endophthalmitis, lens damage, and light toxicity. The smaller gauge fiber illumination could be ideal for preventing complications.
Conclusion
Scleral buckling with a noncontact wide-angle viewing system seems promising for the management of rhegmatogenous retinal detachments, not only with preoperatively detected retinal breaks but also those with undetected retinal breaks.
Disclosure
The authors report no conflicts of interest in this work.
References
- NortonEWRetinal detachment in aphakiaAm J Ophthalmol19645811112414177964
- GriffithRDRyanEAHiltonGFPrimary retinal detachments without apparent breaksAm J Ophthalmol19768144204271266920
- WongDBillingtonBMChignellAHPars plana vitrectomy for retinal detachment with unseen retinal holesGraefes Arch Clin Exp Ophthalmol198722542692713653720
- CriswickVGBrockhurstRJRetinal detachment. 360 degree scleral buckling as a primary procedureArch Ophthalmol19698256416504900067
- GrizzardWSHiltonGFHammerMETarenDA multivariate analysis of anatomic success of retinal detachments treated with scleral bucklingGraefes Arch Clin Exp Ophthalmol19942321178119596
- DevenyiRGde Carvalho NakamuraHCombined scleral buckle and pars plana vitrectomy as a primary procedure for pseudophakic retinal detachmentsOphthalmic Surg Lasers199930861561810507563
- BrazitikosPDD’AmicoDJTsinopoulosITStangosNTPrimary vitrectomy with perfluoro-n-octane use in the treatment of pseudophakic retinal detachment with undetected retinal breaksRetina199919210310910213234
- RosenPHWongHCMcLeodDIndentation microsurgery: internal searching for retinal breaksEye (Lond)19893Pt 32772812612671
- KitaMYoshimuraNEndoscope-assisted vitrectomy in the management of pseudophakic and aphakic retinal detachments with undetected retinal breaksRetina20113171347135121358462
- TewariHKKedarSKumarAGargS PVermaLKComparison of scleral buckling with combined scleral buckling and pars plana vitrectomy in the management of rhegmatogenous retinal detachment with unseen retinal breaksClin Experiment Ophthalmol200331540340714516427
- SaliconeASmiddyWEVenkatramanAFeuerWManagement of retinal detachment when no break is foundOphthalmology2006113339840316406538
- JacksonTLKwanASLaidlawAHAylwardWIdentification of retinal breaks using subretinal trypan blue injectionOphthalmology2007114358759017123612
- WongRGuptaBAylwardGWLaidlawDADye extrusion technique (DE-TECH): occult retinal break detection with subretinal dye extrusion during vitrectomy for retinal detachment repairRetina200929449249619262427
- ArasCUcarDKoytakAYetikHScleral buckling with a non-contact wide-angle viewing systemOphthalmologica2012227210711022076572
- ShibaHShibaTKodakaRKamizuruMShibaKRetinal reattachment surgery using wide-angle viewing systems and chandelier illuminationFolia Japonica de Ophthalmologica Clinica2010232301304 Japanese