?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Video abstract
Point your SmartPhone at the code above. If you have a QR code reader the video abstract will appear. Or use:
Purpose
To compare the effects of age and near phoria on interpupillary distance measured at far (FIPD) and near (NIPD) using the Viktorin’s and pupillometer (PD-5) methods.
Methods
Interpupillary distance (IPD) by Viktorin’s method and the corneal reflex pupillometer (PD-5) method, as well as near heterophoria by the Saladin near point card, were each obtained on 133 randomly selected normal subjects aged 20–67 years. Comparison within and between techniques, influence of age on IPD, and near heterophoria were assessed.
Results
The mean FIPD varied significantly from the NIPD (P < 0.001 for both methods). Overall, FIPD ranged from 56–73 mm, and NIPD ranged from 50–70 mm. For FIPDs of 55 mm, 63 mm, and 71 mm, the corresponding NIPDs were less by 3.9 mm, 4.4 mm, and 5.0 mm, respectively, which were measured by Viktorin’s method, and 4.0 mm, 4.6 mm, and 5.2 mm, respectively, measured by the PD-5 method. Between methods, the limits of agreement were: −3.9 mm and 3.2 mm (P > 0.05) for FIPD, and −3.1 mm and 2.9 mm (P > 0.05) for NIPD. Both IPDs varied significantly across age groups (P < 0.0001). Post hoc analysis revealed a significant variation (P < 0.01 in both techniques) only in the comparison between age groups 16–25 years and 41–67 years. The mean difference was −2.2 mm (−4.0 mm to −0.3 mm) and −2.8 mm (−4.7 mm to −1.0 mm) for Viktorin’s method for FIPD and NIPD, respectively. For PD-5, the corresponding values were −1.3 mm (−3.2 mm to 0.4 mm) and −1.7 mm (−4.1 to −0.5 mm). Also, the near phoria differed significantly (P < 0.0001) across age groups and correlated positively with age (r2 = 0.27, P < 0.0001) and NIPD (r2 > 0.04; P < 0.03, both techniques).
Conclusion
The difference between FIPD and NIPD (about 4.4 mm in Arab males) was observed independent of the technique used. The Viktorin’s and the PD-5 methods of IPD assessment resulted in similar values, and therefore, could be interchangeably used. However, caution is advised in cases of high power refractive corrections as the difference could vary from −4 mm to +3 mm (FIPD) and −3 mm to +3 mm (NIPD). Both IPDs have demonstrated an increase until the patients are in their early 40s, and a slight decrease has been observed thereafter. Age and NIPD were significantly associated with heterophoria in our subjects.
Introduction
Interpupillary distance (IPD) is the distance between the centers of the pupils. It determines the stereo separation of the two images, which are combined in the brain to produce stereo perception. It has been shown to correlate with head size, and as such is an important parameter used by the optical industries in the design and manufacture of lenses.Citation1 Knowledge of mean IPD is important in the satisfactory performance of finished spectacles. Ophthalmic lenses are positioned before the eyes such that their optical centers coincide with the centers of the pupils in order to eliminate unwanted prismatic effects.Citation2 Normative values of IPD are also useful in surgery after facial trauma, and have been applied in the selection of artificial teeth.Citation3 Juberg et alCitation4 listed a number of syndromes in which the knowledge of IPD could be helpful in their diagnosis (eg, ocular hypertelorism, Waardenburg syndrome, mongolism, and so on). More recently, it has been applied in the diagnosis of fetal alcohol syndrome.Citation5
Several studies have demonstrated an increase in far IPD (FIPD) with age in both males and females.Citation6–Citation12 A parallel and steady increase was evident for both genders from infancy through to puberty,Citation9 and this increase slows down from the time individuals reach their middle 20s to their late 30s.Citation13 Afterwards, a slight decrease occurs in older subjects.Citation7,Citation9 Fesharaki et alCitation13 showed that mean IPD in an Iranian population increased 4.8 mm during the second decade, 1.7 mm during the third decade, and 0.6 mm during the fourth and fifth decades of life. Another study showed an increase in FIPD and NIPD of female Arabs across age groups (7 years to 40 years).Citation6 Interestingly, Chen and O’LearyCitation8 also showed that IPD changes significantly with age, but that the oculomotor control system for convergence can compensate for these age-related changes in IPD during childhood.
Vernier calipers, video centration devices,Citation14 photographs,Citation15,Citation16 the ruler–Viktorin’s method,Citation6,Citation9 and pupillometers,Citation14,Citation17,Citation18 have all been used in the determination of human IPDs. Essentially, these techniques operate on one of two principles: measuring the distance between the two principal corneal reflexes (physiological IPD), or measuring the distance between common points on each eye (anatomical IPD).Citation18 The Viktorin’s method and pupillometer have been commonly employed in the clinical determination of IPD. While the former measures IPD by determining the distances between appropriate features in each eye (in this case, the temporal and nasal pupil margins in each eye respectively), the latter is able to measure IPD using the corneal reflex, and has been shown to give more repeatable results at far and near IPDs.Citation2,Citation17–Citation19 The anatomical IPD (determined by the Viktorin’s method) locates the line of sight or optical axis of the eye, while the physiological IPD (determined by pupillometer) locates the visual axis. Since these two axes are not coincident,Citation18 the anatomical IPD is usually 0.5–1.0 mm larger than the physiological IPD.Citation17
A search of the published literature revealed that very few studies have evaluated the differences in anatomical and physiological IPD as measured by the Viktorin’s method and pupillometer, respectively. Though the results of these studies have been contradictory, they have also either presented data on a few subjects,Citation2,Citation18,Citation20,Citation21 or have considered only the FIPD while neglecting the NIPD,Citation17,Citation19 which is important during the selection and manufacture of reading glasses, as shown in previous studies.Citation22–Citation24 Elliot and Green’sCitation23 study found a high prevalence of induced horizontal (60%) and vertical prism (32%) beyond the tolerance levels stipulated in the International Organization for Standardization ISO 16034:2002 after examining 322 near-vision ready-made spectacles and strongly recommended that manufacturers use a centration distance for near-vision ready-made spectacles that is similar to an average near (and not distance) IPD. PointerCitation24 also observed that in Caucasians, the NIPD stabilizes across the presbyopic age span (41–80 years), and as such advised the need to specify two lens centration distances in order to cater to the gender of the intended Caucasian wearer: namely 62 mm for male and 59 mm for female presbyopes.
Comparing different methods of IPD measurement, Holland and SiderovCitation17 reported that FIPD measured using the Viktorin’s method did not differ significantly from that obtained by pupillometer on the first measurement, whereas on retest, the former returned an FIPD that was statistically significantly greater than the latter by about 0.40 mm. However, the authors attributed this small difference to a statistical quirk. Another comparative study conducted more than a decade ago reported that both techniques measured FIPDs that were clinically similar, and as such, could be used interchangeably in practice.Citation18 In view of the controversy that exists on the differences in FIPD obtained using the Viktorin’s method and pupillometer; the nonavailability of data comparing the difference between FIPD and NIPD obtained by both devices; and the potential significance of the results in our population, we designed this study using both techniques. The aim of this study was: (1) to compare the differences in far and near anatomical and physiological IPD as measured by the Viktorin’s and pupillometer methods, respectively, so as to be able to predict the FIPD when the NIPD can be measured (for instance, in a case where the examiner is amblyopic in one eye); (2) to assess and compare the limits of agreement (LoA) between anatomical and physiological IPD at both distances as obtained by both devices; and (3) to evaluate the changes in anatomical and physiological FIPD and NIPD across various ages. In addition, we also assessed the influence of age and NIPD on near heterophoria.
Methods
Subjects
A total of 133 Saudi males with a mean age of 30.4 ± 13.0 years (mean ± standard deviation; range: 20 to 67 years) were randomly recruited from a population of students from the College of Applied Medical Sciences, and relatives of subjects visiting the optometry clinic for routine eye examinations between December 2012 and January 2013 for participation in this study. We choose the lower band of the age limit in order to minimize the reported effects of menstruation changes that occur during childhood physical growth changes,Citation6 while the upper band of the age limit was chosen to minimize confounding factors arising from the increased laxity of the soft tissues around the orbit of the elderly subjects.Citation9 However, the decision to include only males was made because data was collected from the College of Applied Medical Sciences Optometry department male-only clinic, and/or to enhance the direct comparison of our findings with those of Osuobeni and al-Gharni,Citation15 which was carried out a decade ago on male samples of a similar population.
Subjects were included if there was no ocular pathology, if they recorded an acuity of 6/6 or better, and had no binocular vision anomalies. Distance refractive correction ≥ ±6.00 diopters sphere and ≥−2.00 diopters cylinder, and anisometropia of −2.00 diopters spherical equivalent, excluded the subjects’ data from inclusion in the sample.
Ethical approval was obtained from the College of Applied Medical Sciences Research Ethics Committee. The purpose of the study was explained, and each subject signed an informed consent sheet. The study adhered to the principles of the 1967 Helsinki declaration (as modified in Edinburgh, UK in 2000).
Data acquisition
IPD was obtained on each subject by the same examiner using two methods: Viktorin’s method and a commercial corneal reflection digital pupillometer, PD-5 (Topcon Corporation, Tokyo, Japan), which has been in everyday use in the clinic. This was followed by determination of near heterophoria using the Saladin Near Point Balance Card version 1.0 (Saladin card; Bernell Corp, Mishawaka, IN, USA). No recalibration of the pupillometer was done specifically for this study. Determination of the IPD measurement methods to be first used was done by randomization via a series of random numbers generated from the Microsoft Word, 2010 (Microsoft Corporation, Redmond, WA, USA). One examiner (SA) obtained all IPD measurements, while a second examiner (UO) who recorded the pupillometer readings (so the first examiner [SA] had no knowledge of the pupillometer readings), obtained measurements of near heterophoria in all subjects.
Methods used to measure IPD and heterophoria
Viktorin’s method
This method was adopted as it has remained the most widely taught and practiced IPD measurement technique,Citation9 and since it was the most widely cited in published data involving the assessment of IPD.Citation7 The FIPD and NIPD were simultaneously measured by one examiner using a millimeter rule, as outlined by Sasieni.Citation25 The subject was seated opposite to, on the same level as, and within arm’s length of the examiner in a well-lit optometry consulting room. A PD rule calibrated in millimeters was laid across the subject’s nose and lightly supported by the examiner’s left hand. The subject was instructed to keep both eyes open and to fixate at the examiner’s open left eye; using this eye, the examiner aligned the “zero” mark on the PD rule with the edge of the temporal limbus of the subject’s right eye, and sighted the point on the ruler that corresponded to the nasal limbus of the subject’s left eye. This measurement is equivalent to the NIPD value. Keeping the ruler still, the examiner then closed his left eye and opened his right eye, while instructing the subject to move fixation across to the examiner’s open right eye. The examiner also sighted the point on the ruler that corresponded to the nasal limbus of the subject’s left eye. This measurement is equivalent to the FIPD. The same procedure was repeated from the right to left, and the averages were recorded.
Pupillometer method
The examiner aligned the crosshairs of the pupillometer, which was set for a 40 cm distance with the corneal reflexes of the subject. This is equivalent to NIPD. The pupillometer was then reset at an infinite distance and realignment of the crosshairs with the subjects’ corneal reflexes was again performed. This is equivalent to FIPD.
Heterophoria measurement
A horizontal dissociated heterophoria test was performed for every participant for near heterophoria; however, vertical heterophoria was not assessed. It is acknowledged that convergence/divergence is an active mechanism, and accommodative vergence refers to a blur-driven change in the horizontal alignment of the two eyes.Citation26 In 2001, the Saladin card was designed by Saladin to provide a quick measurement device for several visual function parameters at near: near VA (logarithm of the minimum angle resolution), horizontal and vertical dissociated heterophoria, horizontal and vertical associated heterophoria, horizontal and vertical fixation disparity, accommodative facility, vergence facility, and monocular estimation method retinoscopy for accommodation lag. The Saladin Near Point Balance Card was adopted for use in this study not only because of its versatility, but also because it is considered to be a faster procedure than the Sheedy disparometer,Citation27 and has a black disk with words surrounding the black discs, possibly acting to control and/or stabilize accommodation during the test; therefore, the print supposedly forms an additional peripheral lock. It has also been found to be the most repeatable subjective dissociated phoria test.Citation28,Citation29 The Saladin card has the advantage of being an inexpensive, small, lightweight, and portable facility,Citation28 making it particularly useful in nontraditional optometric settings such as in schools and nursing homes.Citation30,Citation31
Near heterophoria was recorded using a Maddox rod and Saladin Card placed at eye level at 40 cm with an illumination level of 300 lux measured using a Minolta illuminance meter (Konica Minolta Sensing Singapore Pte Ltd, Shanghai, People’s Republic of China). A light-emitting diode light source was used to produce a spotlight source behind the Saladin card, which was seen through the central pinhole located at the intersection of the horizontal and vertical scales. The subject was instructed to report the position of the vertical red line in relation to the central spot light (left or right), and the number intersected on the scale (measured in prism diopters [pd]), which represented the dissociated heterophoria. Where the subjects reported heterophoria between two line scales, the mid-value was recorded.
Data analysis
All visual data and background information for each subject was entered into a computer database, but only those relevant to the study were exported for each subject for analysis into a Microsoft Excel (Microsoft Corporation) spreadsheet. GraphPad InStat version 3.00 (GraphPad Software Inc, San Diego, CA, USA) statistical software was used for subsequent standardized analysis. To achieve a statistical power of 85% at a significance level of α = 0.05, 123 subjects were required for this study. This sample size calculation was determined from an initial sample of 15 subjects using the statistical freeware G*Power (version 3; Heinrich Heine Universität Düsseldorf, Dusseldorf, Germany).
Mean values of age in years, FIPD and NIPD in millimeters, and heterophoria in pd were all descriptively analyzed. Comparisons of FIPD and NIPD within technique and between techniques in all subjects were performed using repeated measures analysis of variance (ANOVA). The columns analyzed were columns of FIPD versus NIPD (Viktorin’s method) versus FIPD versus NIPD (PD-5 method).
We assessed the agreement at both distances within and between techniques by obtaining the difference between IPD measured at both distances by the same technique (within-technique) and between techniques, and determined the 95% LoA (mean difference ± 1.96 × standard deviation of the differences). The LoA defined the region of IPD measurements within which there was a 95% probability that the differences occurred due to measurement variability and a 5% probability that the difference was real and not due to measurement error.Citation32
To assess the reported differences between age groups in relation to IPD and phoria,Citation8,Citation9,Citation11,Citation16,Citation33–Citation35 subjects were divided into three age groups and further analysis was conducted between age groups using one-way ANOVA. The age groups were: 16–25 years (n = 90); 26–40 years (n = 10) and 40–67 years (n = 33). The association of age with heterophoria and IPD with heterophoria were both tested and analyzed across individuals using a linear regression model to assess the rate of change in each association, as well as the significance level of any existing relationship.
Results
Average values of all measurements and subjects
Descriptive statistics for the mean values (in millimeters) of the two techniques used in the measurement of IPD are given in . In general, the mean FIPD and NIPD in Saudi males ranged between 56–73 mm and 50–70 mm, respectively, in spite of the technique used.
Table 1 Mean values ± SD, range of anatomical and physiological IPDs as measured by the Viktorin’s and Topcon PD-5 pupillometer method, respectively, for FIPD and NIPD in millimeters
Limits of agreement in IPD obtained by same technique (within-technique) and across techniques (between techniques)
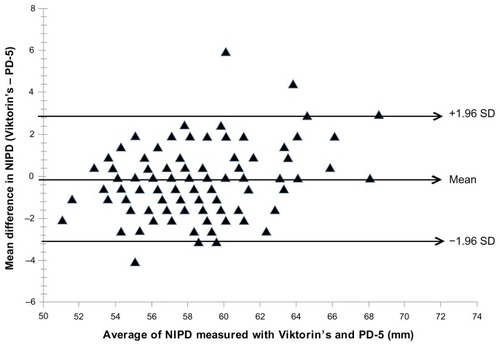
A repeated measures ANOVA conducted using four levels of the factor method of measurement (essentially two corresponding to each technique – one for near and one for far) revealed a significant difference in IPD across the methods of measurement (F3,612.5 = 27.4, P < 0.0001). Bonferroni corrected posttest analysis showed that the measurement of IPD was not dependent on the method of measurement employed (P > 0.05); rather, it was dependent on the distance at which IPD measurement was obtained (P < 0.001). On the average, the FIPD obtained by the Viktorin’s method and the PD-5 methods were, respectively, 4.4 mm and 4.6 mm greater than the NIPD obtained by the same technique. The magnitude of the 95% LoA between FIPD and NIPD is shown in the Bland–Altman plot ( [Viktorin’s method]; [PD-5 method]). Linear regression analysis plot of the differences in FIPD and NIPD as a function of FIPD obtained by each technique () are best explained by the following equations:
Figure 1 Limit of agreement (LoA) in anatomical interpupillary distance (IPD) measured for FIPD and NIPD using the Viktorin’s method, in millimeters.
Abbreviations: LoA, limit of agreement; IPD, interpupillary distance; FIPD, far interpupillary distance; NIPD, near interpupillary distance; SD, standard deviation.
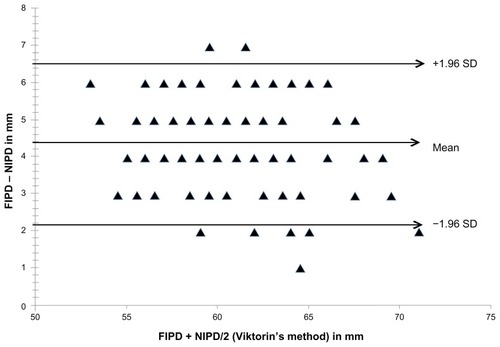
Figure 2 Limit of agreement in physiological interpupillary distance IPD measured for FIPD and NIPD using the pupillometer (PD-5) method, in millimeters.
Abbreviations: IPD, interpupillary distance; FIPD, far interpupillary distance; NIPD, near interpupillary distance; SD, standard deviation.
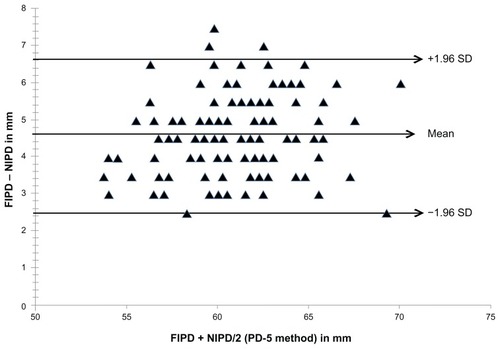
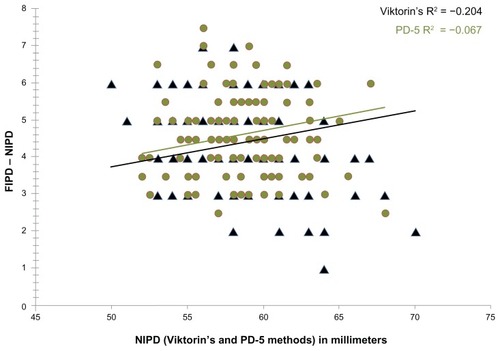
Figure 3 Linear regression plot of the difference in IPD for FIPD and NIPD as a function of NIPD in millimeters.
Between techniques, the width of the 95% LoA was wider for FIPD (7.1 mm; ) than NIPD (5.9 mm; ), with the pupillometer consistently measuring IPDs larger than the Viktorin’s method. However, the differences were not statistically significant at both far and near (P > 0.05, for both).
Figure 4 Limit of agreement between anatomical and physiological IPD as measured by Viktorin’s and PD-5 pupillometer methods, respectively, at FIPD, in millimeters.
Abbreviations: IPD, interpupillary distance; FIPD, far interpupillary distance; SD, standard deviation.
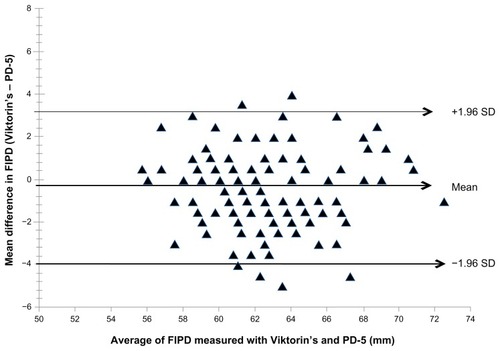
Figure 5 Limit of agreement between anatomical and physiological IPD as measured by Viktorin’s and PD-5 pupillometer methods respectively, for NIPD, in millimeters.
Abbreviations: IPD, interpupillary distance; NIPD, near interpupillary distance; SD, standard deviation.
Comparison of interpupillary distance (IPD) measures between age groups
Subjects were grouped into age groups of 16–25 years, 26–40 years, and 41–67 years, representing young adults, adults, and older adults, respectively. These groupings were selected to enhance the analysis and comparison of the current data with those of other published data on both similar and different populations,Citation6,Citation7,Citation9,Citation10,Citation13 using similar age classification systems.
shows the mean values of FIPD, NIPD in mm, and heterophoria in prism diopters (pd) across the different age groups. The picture emerging from the results of the one-way ANOVA of the age grouped data is shown in . Using the Viktorin’s method, FIPD differed significantly from NIPD across all age groups (F5, 263 = 33.9, P = 0.0001). Post hoc analysis showed statistically significant differences between age groups 16–25 years and 41–67 years with IPD values measured at far (P < 0.05) and near (P < 0.001). All other age group comparisons of mean IPDs measured at both distances by the Viktorin’s method showed nonstatistically significant differences (P > 0.05, for both FIPD and NIPD).
Figure 6 Age-grouped mean values of anatomical and physiological IPDs as measured by the Viktorin’s and PD-5 pupillometer methods, respectively, for FIPD and NIPD in millimeters.
Abbreviations: IPD, interpupillary distance; FIPD, far interpupillary distance; NIPD, near interpupillary distance; SD, standard deviation.
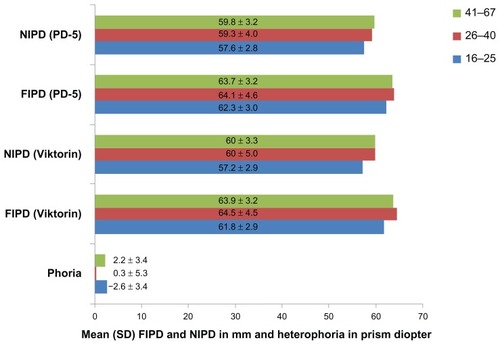
Table 2 Results of age–group comparisons of mean anatomical and physiological IPDs for FIPD and NIPD in millimeters, within-technique (Viktorin’s and PD-5 pupillometer methods)
FIPD and NIPD obtained by the PD-5 method also varied significantly (F5, 263 = 32.8, P = 0.0001) across all age groups. However, post hoc analysis only showed statistically significant differences (P < 0.01) in NIPD when the age group 16–25 years was compared to the 41–67 year age group. The 95% LoA and results of the ANOVA have been presented in .
Influence of age and near interpupillary distance (NIPD) on heterophoria
In the analysis, a negative sign (−) denotes esophoria, a positive sign (+) denotes exophoria, and zero (0) denotes orthophoria. Across all age groups, the difference in the amount of measured heterophoria was statistically significant (F2,131 = 21.9, P < 0.0001). On post hoc analysis between age groups, the difference in measured phoria was statistically significantly different between groups (16–25 years and 26–40 years [mean difference: −2.9, P < 0.05], 16–25 years and 41–67 years [mean difference: −4.8, P < 0.001]). There was no statistically significant difference in the comparison between the 26–40 year and 41–67 year age groups (P > 0.05). The prevalence of near orthophoria, exophoria, and esophoria was 26 participants (19.5%), 38 participants (28.6%), and 69 participants (51.9%), respectively.
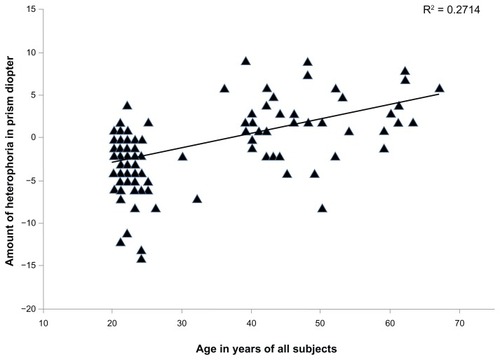
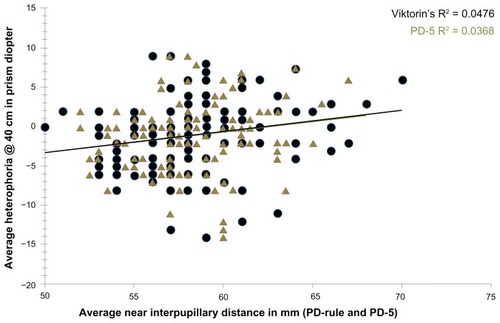
The amount of near heterophoria (in pd) was moderately correlated with the age of subjects (r2 = 0.27, P < 0.0001, ), but was weakly and positively associated with PD-5 measured NIPD (slope: 0.26, r2 = 0.037; P = 0.027; ), and the Viktorin’s method-measured NIPD (slope: 0.27, r2 = 0.0476; P = 0.0116; ). Overall, there was a predominance of exophoria for NIPDs > 63 mm, and esophoria for NIPDs < 62 mm, despite the technique used.
Discussion
Our results show that the mean anatomical FIPD and NIPD in Saudi males ranged from 56–72 mm and 50–70 mm, as well as from 56–73 mm and 52–68 mm for the physiological FIPD and NIPD, respectively. DodgsonCitation33 reported that in a vast majority of adults, FIPD values lie within the range 50 mm to 75 mm. Osuobeni and al-MusaCitation7 reported similar findings for male anatomical FIPD (58–73 mm) and a slightly wider NIPD (56–70 mm) in Arabs aged 26–55 years. Fesharaki et alCitation13 reported the mean IPD in adult Iranian subjects to be 61.1 mm ± 3.5 mm in women, and 63.6 mm ± 3.9 mm in men. HofstetterCitation36 also reported that the mean IPD in 90% of white adults in the United States of America lie between 60 mm and 70 mm, while the majority (99.8%) of his subjects’ IPDs were between 55 mm and 75 mm. More recently, Caucasian male and female mean IPDs have been reported to be 65.3 mm ± 2.8 mm and 62.3 mm ± 2.8 mm (far), and 62.2 mm ± 2.7 mm and 59.3 mm ± 2.8 mm (near), respectively.Citation24 The values reported in the current study fall within the range reported by the cited studies.Citation7,Citation24,Citation33,Citation36 Compared to the study involving Arabs,Citation7 the difference in the measured anatomical NIPD reported in the current study could be attributed to the inclusion of much older subjects (up to 67 years). NIPD decreased slightly (although the difference was not statistically significant) between the 26–40 and 41–67 year age groups in the current study, which could have resulted in the smaller NIPD reported. A similar decrease was also shown in a more recent study where NIPD was shown to decrease from 62.2 mm ± 2.7 mm (at the age of 57 ± 9.6 years) to 59.3 mm ± 2.8 mm (at the age of 55.9 ± 9.7 years) in Caucasian presbyopic males.Citation24
The collation of NIPD data in the present study is important because, over the recent years, there has been an increasing widespread use of relatively inexpensive “ready-made” reading spectacles. This information can be used by manufacturers for horizontal lens centration; distance in such spectacles is intended for this Middle Eastern Arab population, and as such, this can avoid symptoms that may arise as a consequence of misalignment in the horizontal and vertical planes of the positive lenses before the wearer’s eyes.Citation22
Limits of agreement in IPD obtained by same technique (within-technique) and across techniques (between techniques)
IPD measurements obtained using the techniques employed in this study have been previously shown to have good repeatability in the same observer.Citation2,Citation9,Citation18,Citation21 However, AndersonCitation2 claimed that repeated measures of FIPD repeatability was much better in the pupillometer-measured IPDs than in the Viktorin’s method-measured IPDs. The current study did not explore repeatability and as such, verification of this claim was not possible.
The results presented here showed that the mean anatomical FIPD and NIPD obtained using the Viktorin’s method was slightly smaller (although statistically insignificant) than the physiological IPD determined by PD-5 pupillometer by an average of 0.3 mm and 0.1 mm, respectively. McMahon et alCitation19 reported a similarly minimal but significant bias (0.6 mm) in FIPD, with the pupillometer returning larger IPDs. On the other hand, Holland and SiderovCitation17 observed a nonstatistically significant difference (0.08 mm) in FIPD between both techniques when measurements were taken by the same examiner. However, when different observers measured FIPD on the same subject, the difference they observed was statistically significant.
In contrast, a study on Arab subjects reported that the anatomical IPD (determined by Viktorin’s method) was on the average 0.10 mm and 0.30 mm wider than the physiological IPD (determined by PD-5 pupillometer, Essilor Ltd, Thornbury, Bristol, UK) from far and near, respectively.Citation7 Even though the differences in anatomical and physiological IPDs found in the above cited study, and given that the observations in the present study were not statistically significant, the use of different pupillometers in the determination of IPDs has been reported to result in variations larger than 1.5 mm.Citation14 The discrepancy in pupillometer-measured IPDs is not caused by measurement uncertainties or setting errors made by the examiner, but is exclusively due to system-specific calibration differences and differing measuring principles.Citation14
Also, between FIPD and NIPD, the differences were similar in both techniques (4.4 mm ± 1.1 mm and 4.6 mm ± 1.0 mm, P > 0.05; Viktorin’s and PD-5, respectively), and as such, both techniques can be interchangeably used in the clinical determination of male IPDs at both distances by same examiner. This is in agreement with the conclusion reached by a similar study carried out about 2 decades ago.Citation18 Across all subjects, FIPD was consistently significantly larger than NIPD despite the technique used. The average bias was 4.4 mm (Viktorin’s method) and 4.6 mm (PD-5); this is also similar to previous reports.Citation6,Citation7,Citation10,Citation12 PointerCitation24 observed an intragender difference of a slightly lower magnitude (approximately 3 mm) between far and near IPDs obtained by Viktorin’s method in Caucasian presbyopes.
GrossvenorCitation37 calculated the differences between FIPD and NIPD obtained using a corneal reflection method (mm rule) of alignment to be 3.5 mm, 4.0 mm, and 4.5 mm for FIPDs of 55 mm, 63 mm, and 71 mm, respectively. The corresponding differences for the respective FIPDs of 3.9 mm, 4.4 mm, and 5.0 mm (Viktorin’s method); 4.0 mm, 4.6 mm, and 5.2 mm (PD-5 method) observed in the current study were similar to that of Grossvenor.Citation37 This is important in situations where the examiner is amblyopic in one eye. He/she will be able to measure the patients’ NIPD using the normal eye and the appropriate amount based on these differences can be added to obtain the corresponding FIPD and/or the FIPD can be predicted from the linear equation expressed in the results above ().
Influence of age on interpupillary distance
A statistically significant variation was evident in both FIPD and NIPD with advancing age, despite the technique used (P = 0.0001). The FIPD has increased by 2.8 mm and 1.8 mm (Viktorin’s and PD-5, respectively) from the early adulthood years (16 to 25 years) to late adulthood (26–40 years). A decrease of 0.6 mm and 0.4 mm (Viktorin’s and PD-5, respectively) occurred between the adults (26–40 years) and older adults (41–67 years). A similar but slightly different trend was shown in the NIPD (). Between early adulthood (16–25 years) and old age (41–67 years), the FIPD had increased by 2.2 mm and 1.3 mm (Viktorin’s and PD-5, respectively), with the NIPD increasing by 2.8 mm and 2.3 mm (Viktorin’s and PD-5, respectively). This indicates that in line with previous reports,Citation6,Citation9,Citation38–Citation41 the increase in FIPD and NIPD in early adulthood continues towards an individual’s late 30s, and begins to decrease in the fourth decade of life.
Chen and O’LearyCitation8 revealed a significant difference in the IPD growth rate between men and women. Evereklioğlu et alCitation10 postulated that the average total growth increment for NIPD and FIPD in males (7 and 35 years old) were 8.66 mm and 9.31 mm, respectively. Fesharaki et alCitation13 observed an increase in the mean FIPD of 4.8 mm during the second decade, 1.7 mm during the third decade, and 0.6 mm during the fourth and fifth decades of life.
This change in IPD with age can be explained from an anatomical view of the human orbit.Citation9 It is recognized that in infants, the interorbital linear skeletal dimension is small relative to the globe size, which often gives the appearance of a pseudo-squint;Citation9 this increases with the development of the nasal cavity, other sinuses, and the eruption of the teeth. The male continues to develop in the brow region during puberty, showing an increase in the width of the facial bones, which produces a horizontal–rectangular orbital entrance. This is quite different from female development during puberty; thus, the gender difference in the human facial skeleton.Citation9 The fact that the bony orbit itself continues to grow into adulthood and only attains its full dimension at puberty, with subsequent changes occurring around the orbital margin in the elderly as a consequence of bone atrophy, explains the differences in the rate of IPD progression in the age groups reported in the current study. Therefore, the current findings confirm that age can cause bidirectional changes in IPDs, most likely due to the reported effects of menstruation changes that occur during childhood physical growth changes and other changes in body features (leading to a rapid increase in IPD) on the one hand,Citation6 and the increased laxity of the soft tissues in the elderly subjects (leading to a decrease in IPD) on the other.Citation39
Influence of age and near interpupillary distance (NIPD) on near heterophoria
Age has been strongly associated with stereopsis, fusional vergence, and the accommodative convergence/accommodation ratio.Citation35,Citation42 Normality of all of the above visual functions is responsible for comfortable single binocular vision, and has been reported to decrease with increasing age. A significant association has been shown to exist between age and phoria.Citation8,Citation34,Citation35 In one study,Citation8 about 98% of the children below 5 years of age were found to be predominantly exophoric at near. Anderson et alCitation35 assessed different ocular functions including fusional vergences, near point of convergence (NPC), distance and near phoria, and IPD annually, over a period of 10 years in 114 subjects aged 7 to 13 years. They reported that the mean distance phoria at year 1 was 0.1 pd exophoria, and this did not change throughout the study period, whereas a significant (P < 0.001) shift in near phoria over the 10-year study period (2.4 pd esophoria to 4 pd exophoria) occurred. In the present study, heterophoria was positively associated with changes in age and NIPD ( and , respectively) at a significant level. Subjects exhibited near esophoria up until their mid-30s, and beyond this stage, a shift towards exophoria was shown (). A similar trend was also observed in the relationship between NIPD and the amount of near heterophoria (). There was also a tendency for greater near esophoria in subjects with NIPD, which was smaller than 62.5 mm, and greater near exophoria in subjects with larger NIPD. This indicates that, as noted by a previous study,Citation8 there is a reduction in the ability of the oculomotor control system to converge to compensate for age-related changes in IPD. This oculomotor system is responsible for overcoming the increasing demand on total convergence as predicted from IPD during childhood; however, with age, this muscular capability decreases. Again, because the accommodative convergence or proximal convergence (which play a role in maintaining the process of orthophorization at early adulthood) also suffer from a depreciation in function due to aging;Citation35 and with the observed decrease in near base-out ranges (compensating vergence for exophoria) from childhood to early adulthood not being accompanied by significant changes in near base-in ranges over this time period,Citation43 we will therefore expect a predominance of exophoria (as observed in the current study) in the older age group.
On the other hand, the direction of the observed trend in this study may be logical given that individuals with a larger IPD will have a greater convergence demand for near tasks, and with increasing age, they will lose the ability to accommodate, thereby losing the benefit of accommodative convergence. Also, an increase in IPD with age affects the oculomotor function by increasing the amount needed for rotation of the eyes.Citation8 When this happens, the demand on fusional vergence (base-out ranges) becomes greater, and a shift towards exophoria results, as was observed in the older adults. The probability for even greater exophoria, and a greater loss of compensating fusional vergence ability, results in near point symptoms, which is evident in the reading difficulty commonly experienced by the presbyopic subjects.
Accommodation and vergence help maintain single and focused visual experiences while an object moves in depth. Theoretically, the relationship between them requires constant recalibration as the head grows and hyperopia decreases. Jiang and RamamirthamCitation42 showed that the accommodative convergence/accommodation and convergence accommodation/convergence ratios of adults change when their IPD is artificially increased or decreased by wearing periscopic spectacles for 30 minutes. Again, the accommodative demand for a typical infant is larger than for an adult as a result of their hyperopic refractive error,Citation44 while the vergence demand is smaller because of their narrow IPD.Citation11 This effect is likened to the observation in the current study where the propensity to be esophoric at near was observed in subjects with smaller NIPDs, and a greater exophoria in subjects with larger NIPDs. Previous studies have observed similar age variations as in interocular distance,Citation15 intercanthal distances, head circumference,Citation12 axial length, and eyeball size and shape.Citation45 Osuobeni and al-GharniCitation15 showed that interocular distance was wider in older subjects than in younger subjects, due to soft tissue changes resulting from aging. Osunwoke et alCitation12 reported that intercanthal distances and head circumference were significantly smaller in both males and females of 3–7 years of age in relation to subjects aged 18–21 years. In another study,Citation45 axial length, as well as eyeball size and shape were shown to increase with age. The study also observed that, in all subjects, the axial length increased rapidly from infancy until about age 10, after which no significant change occurred, whereas the change in eye shape (from oval to spherical or vice versa) was dependent on the refractive error of the subject.
Since all these parameters increase with age including NIPD, while accommodation depletes,Citation42 it can then be deduced that, the farther away the eyes are from each other, the greater the demand on accommodation and fusional vergence (which are required to maintain single binocular vision). The tendency for the eyes to deviate outward (exophoria) as observed in the current study, may then not be unexpected.
While the current study has strength in the protocol of selection of our subjects; the visual functions hereby assessed; and the wider age range of subjects, which could enable generalization of the results in subjects of various age groups; it is also limited by the gender selection of the study. There is the need for further studies evaluating these ocular functions in both genders to assess the rate of change with increasing age.
In conclusion, the study offers population-specific data on anatomical and physiological FIPDs and NIPDs that can be used to aid in the development of spectacles, frames, and over-the-counter ready-made reading spectacles in this region to ensure a better fit and to ameliorate problems associated with misalignment. It is also useful in syndrome diagnosis. The study showed that: (1) FIPD and NIPD increases with age; (2) between FIPD and NIPD, differences as much as 6.6 mm and as low as 2.2 mm in Arab males should be expected; and (3) the mean anatomical FIPD and NIPD obtained using the Viktorin’s method and the mean physiological IPD determined by PD-5 pupillometer in a clinic setting could be interchangeably used, insofar as both measurements are obtained by the same examiner. However, in such situations, caution should be exercised, especially in patients requiring high power refractive corrections as this difference could vary from −4 mm to +3 mm (FIPD) and −3 mm to +3 mm (NIPD). Such variations might be intolerable as a result of the induced prismatic effects. Also, NIPDs significantly influenced the phoria position of the eyes, as subjects exhibited greater near esophoria in smaller NIPDs, and greater near exophoria in larger NIPDs.
Acknowledgments
The authors extend their appreciation to the Research Centre, College of Applied Medical Sciences, and the Deanship of Scientific Research at King Saud University for funding this research.
Disclosure
The authors report no conflicts of interest in this work. No competing financial interests exist.
References
- QuantJRWooGCNormal values of eye position in the Chinese population of Hong KongOptom Vis Sci19926921521581584554
- AndersonALAccurate clinical means of measuring intervisual axis distanceAMA Arch Ophthalmol195452334935213188477
- CesarioVAJrLattaGHJrRelationship between the mesiodistal width of the maxillary central incisor and interpupillary distanceJ Prosthet Dent19845256416436593457
- JubergRCSholteFGTouchstoneWJNormal values for intercanthal distances of 5- to 11-year-old American blacksPediatrics19755534314361143983
- GrobbelaarRDouglasTSStereo image matching for facial feature measurement to aid in fetal alcohol syndrome screeningMed Eng Phys200729445946416904364
- OsuobeniEPFadenFKInterpupillary distance of females of Arab originOptom Vis Sci19937032442478483587
- OsuobeniEPal-MusaKAGender differences in interpupillary distance among ArabsOptom Vis Sci19937012102710308115125
- ChenAHO’LearyDJChanges in the interpupillary distance with the age and its effect on the near fusion free positionAust N Z J Ophthalmol1997251S6S89267612
- PointerJSThe far interpupillary distance. A gender-specific variation with advancing ageOphthalmic Physiol Opt199919431732610645388
- EvereklioğluCDoğanaySErHGündüzADistant and near interpupillary distance in 3448 male and female subjects: final resultsTurgut Özal Tıp Merkezi Dergisi1999628491
- MacLachlanCHowlandHCNormal values and standard deviations for pupil diameter and interpupillary distance in subjects aged 1 month to 19 yearsOphthalmic Physiol Opt200222317518212090630
- OsunwokeEADidiaBCOlotuEJYerikemaAHA study on the normal values of inner canthal, outer canthal, interpupillary distance and head circumference of 3–21 years ijawsAmerican Journal of Scientific and Industrial Research201236441445
- FesharakiHRezaeiLFarrahiFBanihashemTJahanbkhshiANormal interpupillary distance values in an Iranian populationJ Ophthalmic Vis Res20127323123423330061
- WesemannWComparison of PD measuring devices. Part 2Optician20102228
- OsuobeniEPal-GharniSSOcular and facial anthropometry of young adult males of Arab originOptom Vis Sci199471133378145995
- PackiriswamyVKumarPRaoKGPhotogrammetric analysis of palpebral fissure dimensions and its position in malaysian South Indian ethnic adults by genderN Am J Med Sci201241045846223112966
- HollandBJSiderovJRepeatability of measurements of interpupillary distanceOphthalmic Physiol Opt1999191747810615442
- OsuobeniEPal-FahdiMDifferences between anatomical and physiological interpupillary distanceJ Am Optom Assoc19946542652718014368
- McMahonTTIrvingELLeeCAccuracy and repeatability of self-measurement of interpupillary distanceOptom Vis Sci201289690190722581116
- BackmanHInterpupillary distance measurementsAm J Optom Arch Am Acad Optom19724932642664502360
- Mattison-ShupnickMComparing methods and techniques for interocular distance measurements-part 1Optometric Monthly1980711012
- JonassonFThordarsonKRefraction and interpupillary distance measurements of adult Icelanders with special reference to presbyopes possible use of supermarket standard spectaclesActa Ophthalmol Suppl198718244472837060
- ElliottDBGreenAMany ready-made reading spectacles fail the required standardsOptom Vis Sci2012894E446E45122327798
- PointerJSThe interpupillary distance in adult Caucasian subjects, with reference to ‘readymade’ reading spectacle centrationOphthalmic Physiol Opt201232432433122587807
- SasieniLSPrinciples and Practice of Optical Dispensing and Fitting3rd edLondon, UKButterworths197545185
- SchorCCiuffredaKVergence Eye Movements: Basic and Clinical AspectsLondon, UKButterworths1983492
- GossDAPatelJComparison of fixation disparity curve variables measured with the Sheedy Disparometer and the Wesson Fixation Disparity CardOptom Vis Sci19957285805888539027
- CorbettAMaplesWCTest-retest reliability of the Saladin cardOptometry2004751062963915508864
- FrantzKAElstonPMichalikETemplemanCDZoltoskiRKComparison of fixation disparity measured by saladin card and disparometerOptom Vis Sci2011886E733E74121423065
- MaplesWCOptometry’s paradigm shiftOptometry200172956756911575692
- ZabaJNJohnsonRAReynoldsWTVision examinations for all children entering public school – the new Kentucky lawOptometry200374314915812645848
- BlandJMAltmanDGStatistical methods for assessing agreement between two methods of clinical measurementLancet1986184763073102868172
- DodgsonNAVariation and extrema of human interpupillary distanceWoodsAJMerrittJOBentonSABolasMJProceedings of the SPIE Stereoscopic Displays and Virtual Reality XI conferenceJanuary 19–22, 2004San Jose, CA200452913646
- LeoneJFCornellEMorganIGPrevalence of heterophoria and associations with refractive error, heterotropia and ethnicity in Australian school childrenBr J Ophthalmol201094554254619850581
- AndersonHStuebingKKFernKDMannyRETen-year changes in fusional vergence, phoria, and nearpoint of convergence in myopic childrenOptom Vis Sci20118891060106521623250
- HofstetterHWNormal values of interpupillary distanceJ Am Optometric Assoc19724311511155
- GrosvenorTPrimary Care Optometry5th edSt. LouisButterworth2007183208
- PryorHBObjective measurements of interpupillary distancePediatrics19694469739775365062
- FledeliusHCStubgaardMChanges in eye position during growth and adult life as based on exophthalmometry, interpupillary distance, and orbital distance measurementsActa Ophthalmol (Copenh)19866454814863492853
- BrücknerRBatscheletEHugenschmidtFBasal longitudinal study on aging (1955–1978). Ophthalmo-gerontological research resultsDoc Ophthalmol19876432353103622222
- LakshminarayanaPJanardhanKDavidHSAnthropometry for syndromologyIndian J Pediatr19915822532581879907
- JiangBCRamamirthamRThe adaptive effect of narrowing the interocular separation on the AC/A ratioVision Res200545202704270915890382
- ScheimanMWickBPrimary care of binocular vision, accommodative, and eye movement disordersClinical Management of Binocular Vision: Heterophoric, Accommodative, and Eye Movement Disorders2nd edPhiladelphia, PALippincott Williams & Wilkins2002118121
- AslinRNJacksonRWAccommodative-convergence in young infants: development of a synergistic sensory-motor systemCan J Psychol1979334222231546490
- SongHTKimYJLeeSJMoonYSRelations between age, weight, refractive error and eye shape by computerized tomography in childrenKorean J Ophthalmol200721316316817804923