Abstract
This case report describes a case of Alagille syndrome with developing intraocular lens subluxation and rhegmatogenous retinal detachment 4 years after cataract surgery. A 15-year-old female patient with Alagille syndrome-associated cataracts in both eyes underwent phacoemulsification aspiration and intraocular lens implantation. Four years postoperative, intraocular lens subluxation developed in her left eye. For treatment, extraction of the dislocated intraocular lens, anterior vitrectomy, and intraocular lens fixation was performed. Three weeks later, the patient developed rhegmatogenous retinal detachment, which was well-treated by pars plana vitrectomy. Cataract surgery needs to be performed carefully in patients with Alagille syndrome due to the weakness of the zonule of Zinn. Careful postoperative observation is necessary for patients with Alagille syndrome who have undergone intraocular surgery in order to facilitate early detection of a possible rhegmatogenous retinal detachment.
Keywords:
Introduction
Alagille syndrome is an autosomal dominant multiple malformation disorder associated with hypoplasia of intrahepatic bile ducts, a characteristic facial appearance, and abnormalities of the cardiovascular system and vertebra.Citation1 Variable ocular anomalies also occur with this syndrome, most commonly comprising posterior embryotoxon, chorioretinal degeneration, and cataract.Citation2–Citation5 In this case report, we performed phacoemulsification aspiration and intraocular lens implantation for a case of Alagille syndrome causing cataracts in both eyes. Postoperative complications such as intraocular lens subluxation and rhegmatogenous retinal detachment developed 4 years after surgery.
Case presentation
Case
A 15-year-old female.
Chief complaint
Visual impairment in both eyes.
Clinical history
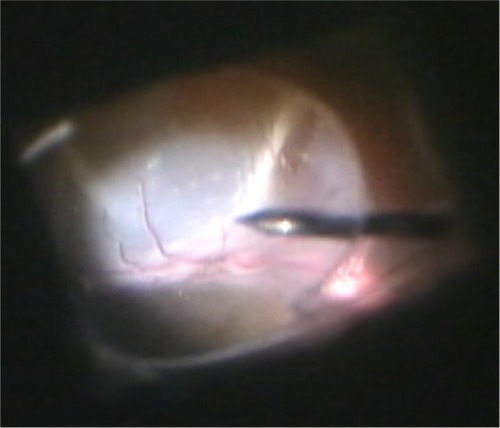
A 15-year-old female patient with Alagille syndrome was referred from the pediatric hepatology department of our Osaka Medical College for investigation of visual loss that had occurred in both eyes. Examination of the patient’s anterior segment revealed bilateral posterior subcapsular cataracts (), and examination of the dilated fundus revealed the existence of a giant optic disc and mild chorioretinal atrophy (). The patient’s corrected visual acuity (VA) was 20/200 in her right eye and 30/200 in her left eye. The axial lengths in the patient’s right and left eye were 22.94 mm and 23.07 mm, respectively. The patient did not report any diplopia, and the movement of both eyes was found to be normal.
Figure 1 Slit lamp microscopy images of the patient’s left eye obtained prior to cataract surgery.
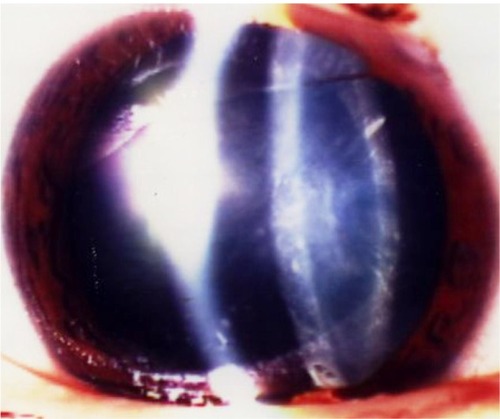
Figure 2 Color fundus photograph of the patient’s left eye, obtained prior to cataract surgery.

In March 2000, we performed phacoemulsification aspiration and intraocular lens implantation for both of her eyes. Postoperatively, VA in the patient’s right and left eyes improved to 20/70 and 20/30, respectively.
In-the-bag fixation of the intraocular lens was achieved without damage of the capsule or zonule of Zinn, but fragility of the zonule was apparent. Following surgery, serial observations were performed in our department. The patient became aware of decreased VA in the left eye beginning in January 2004 and returned to our hospital. Upon examination of the patient, subluxation of the intraocular lens was diagnosed in her left eye (), and she was hospitalized for surgery on March 19, 2004.
Previous history
Serial observations were performed under a diagnosis of intrahepatic bile duct hypoplasia with Alagille syndrome, in the pediatric section of our hospital from October 1988.
Family history
The patient’s mother had also been diagnosed with Alagille syndrome.
Clinical course after hospitalization
Extraction of a dislocated intraocular lens, anterior vitrectomy, and intraocular lens fixation at the ciliary sulcus were performed on March 19, 2004. The operation was concluded without any particular complications, and the patient’s postoperative VA recovered to 20/30. However, she noted decreased VA again on June 7, 2004 and subsequently presented to our hospital. Upon examination, her left eye showed bullous retinal detachment, and we performed vitreous surgery on June 11, 2004. Surgical procedures comprised subtotal vitrectomy, pneumatic replacement of the retina, endophotocoagulation, transscleral cryopexy, peripheral encircling with a silicone band (#240; MIRA, Inc, Waltham, MA, USA), and gas tamponade with 14% C3F8 gas. During the operation, a small retinal tear was detected in the peripheral area of the upper quadrant. As for the vitreous humor, hydropic degeneration was marked in comparison with the patient’s age (). Postoperatively, the patient’s retina was well-attached and her corrected VA improved to 20/50.
Discussion
Posterior embryotoxon, chorioretinal degeneration, optic disk abnormality, posterior subcapsular cataract, microphthalmia, keratoconus, and corneal opacity have been reported as ocular complications associated with Alagille syndrome.Citation2–Citation5 Traboulsi et al described keratoconus and corneal opacity being caused by systemic collagen abnormality in Alagille syndrome.Citation6 In this case, fragility of the zonule of Zinn may have caused subluxation of the intraocular lens. These findings suggest that collagen abnormality is present in various parts of the eye, including the zonule of Zinn, in patients with Alagille syndrome. Thus, surgeons should be careful when determining whether to perform intraocular lens implantation for cataract surgery in Alagille syndrome due to weakness of the zonule of Zinn. Moreover, abnormal vitreous liquefaction, in comparison with the patient’s age, observed in this case may have caused the rapid progression of retinal detachment.
Conclusion
Ocular surgery in the case of Alagille syndrome reported in this present study was performed with a sufficient understanding of the anatomical characteristics as described above, and the postoperative serial observations were considered necessary.
Disclosure
The authors report no conflicts of interest in this work.
References
- TurnpennyPDEllardSAlagille syndrome: pathogenesis, diagnosis, and managementEur J Hum Genet201220325125721934706
- HingoraniMNischalKKDaviesAOcular abnormalities in Alagille syndromeOphthalmology199910623303379951486
- BrodskyMCCunniffCOcular anomalies in the Alagille syndrome (arteriohepatic dysplasia)Ophthalmology199310012176717748259273
- KimBJFultonABThe genetics and ocular findings of Alagille syndromeSemin Opthalmol2007224205210
- WellsKKPulidoJSJudischGFOphthalmic features of Alagille syndrome (arteriohepatic dysplasia)J Pediatr Ophthalmol Strabismus19933021301358501619
- TraboulsiEILustbaderJMLempMAKeratoconus in Alagille’s syndromeAm J Ophthalmol198910833323332774044