Abstract
Purpose
To report a case of retained Descemet’s membrane following penetrating keratoplasty in a patient suffering from Fuchs’ endothelial corneal dystrophy. The use of confocal microscopy, histopathological tissue analysis, and treatment options are discussed.
Methods
Case report of an 85-year-old man with a past ophthalmic history of atrophic macular degeneration, underwent a penetrating keratoplasty for Fuchs’ endothelial corneal dystrophy. Postoperative review revealed a retained retrocorneal membrane within the anterior chamber. Further surgery was performed to excise the membrane, with a subjective and objective postoperative improvement in visual acuity and without subsequent complications of the corneal graft.
Results
Histopathological assessment confirmed the clinical suspicion of a retained Descemet’s membrane, marrying with the initial histology from the corneal button excised during the penetrating keratoplasty, which showed only a very thin Descemet’s layer.
Conclusion
Retention of the Descemet’s membrane following penetrating keratoplasty is a rare but potential complication of this surgery, particularly in cases of Fuchs’ endothelial corneal dystrophy due to the thickened and abnormal histological nature of the endothelium and high index of suspicion is required.
Introduction
Fuchs’ endothelial corneal dystrophy (FECD) is a condition characterized by loss of corneal endothelial cells, thickening of Descemet’s membrane (DM), and deposition of extracellular matrix in the form of guttae. Disease progression results in corneal edema and visual loss secondary to accelerated loss of endothelial cells and reduced function in those present. In severe cases where the visual acuity is markedly decreased, a corneal graft may be performed. This may be either in the form of a penetrating keratoplasty (PK) or Descemet’s stripping automated endothelial keratoplasty (DSAEK).Citation1 Retention of DM is a rare potential complication associated with corneal grafting and there are a number of indications for removal of such membrane. We report a case of surgical removal of retained DM without compromise of corneal graft integrity and with resultant improvement in visual acuity.
Case report
An 85-year-old man was referred to the Aberdeen Royal Infirmary in September 2011 for consideration of corneal grafting due to his poor visual acuity and increasing difficulty with his activities of daily living. He had a history of dry age-related macular degeneration, and FECD. He underwent bilateral phacoemulsification with intraocular lens implants in 1996, and 4 years later was diagnosed with bullous keratopathy. On clinical examination, his best-corrected visual acuities (BCVAs) were OD hand movement and OS 20/200. He had bilateral bullous keratopathy, which was more marked in the right eye. The cornea was edematous with pannus and multiple scars. There was no fundal view but B-scan ultrasonography excluded gross vitreoretinal pathology. The patient was given a guarded prognosis as to the outcome as pre-operative retinal examination was not possible.
In November 2011, he underwent an uncomplicated right PK under general anesthetic using a 7.5 mm donor and recipient punch. A vacuum trephine was used to cut through the cornea in a controlled rotatory manner until the anterior chamber was penetrated, confirmed by evidence of aqueous eruption at the wound site. Scissors were used to separate and remove the button and 10.0 nylon interrupted and continuous sutures were placed. Sub-conjunctival dexamethasone and cefuroxime were administered intra-operatively, along with chirocaine in the sub-Tenon’s space. Dexamethasone Minims® 0.1% and chloramphenicol Minims® 0.5% (Bausch + Lomb, Rochester, NY, USA) were prescribed four times daily for the post-operative period. On day 1 and 2 postoperatively, his BCVA OD was hand movement and postoperative anterior chamber inflammation of 3+ cells was found, based on the standard uveitis classification system.Citation2 At that stage, his steroid treatment was increased to six times a day, along with a Maxitrol® ointment (dexamethasone, neomycin sulphate, polymyxin B sulphate; Alcon Eye Care UK Ltd, Surrey, UK) at night. Fundal examination revealed atrophic age-related macular degeneration, which was expected to affect his visual outcome.
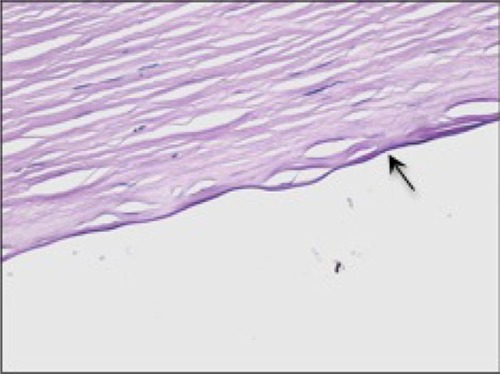
On the ninth post-operative day, BCVA remained hand movement only in the right eye. A clear gap was apparent between the healthy graft and a thin, transparent sheet of tissue in the anterior chamber. The graft was otherwise clear and this sheet was presumed to be retained DM, as confirmed on histopathology (, arrow). Steroid drops were tapered on a monthly basis and his review was arranged for two months with in vivo confocal microscopy testing.
Figure 1 Microscopy of host cornea showing the presence of a thin but distinct Descemet’s membrane (arrow). The specimen was stained with periodic acid-Schiff.
At the next clinical review, the graft had remained clear and in vivo confocal microscopy (IVCM) testing, confirmed the presence of DM and healthy endothelial cell count. This was diagnosed as retention of the host’s DM rather than a detachment of the donor’s DM () as the latter would have been associated with endothelial loss and corneal decompensation. The patient underwent a further uneventful operation for extraction of the retrocorneal membrane under local anesthetic in April 2012.
Figure 2 In vivo confocal microscopy enables high resolution imaging of the cornea and conjunctiva. This image reveals a clear image of the corneal endothelium with healthy cell count and thickness of 502 microns.

Post-operative recovery was uneventful and 2 weeks later, a clear healthy graft with an improved BCVA of OD 20/200 was noted, with the limited acuity more likely related to his atrophic macular degeneration rather than the graft. Further clinical reviews have shown that the graft has remained clear and healthy without any signs of rejection.
Results
By the time of the first review, the microscopy results were available and revealed an opaque keratoplasty specimen and the epithelium showed variability both in thickness and regularity of the contour. Furthermore, there was a very thick layer of sparsely cellular fibrous pannus between the epithelium and Bowman’s membrane, with occasional epithelial downgrowths. Bowman’s membrane was intact and the corneal stroma did not show any definite abnormality. In addition, DM was very thin and extremely difficult to identify in most of the sections examined and virtually no endothelial nuclei were visible on the posterior surface of the cornea. The histological appearances were consistent with the diagnosis of bullous keratopathy with particularly severe formation of subepithelial fibrous pannus ().
Histopathology samples from the second procedure included two very thin membranous structures, 4 mm and 5 mm in size, respectively. These were stained with Paragon and precipitated in a fibrin clot and processed to resin. Structureless, glassy tissue was identified with some periodic acid-Schiff positivity in keeping with DM. No endothelial nuclei were visible on its surface. The other tissue sample appeared to consist only of fibrous tissue ().
Discussion
Retention of DM is a rare potential complication associated with corneal grafting and, although there are limited cases reported in the literature, it has been associated with both PK and DSAEK.
The DM structure consists of two layers of type IV collagen, an anterior embryonic layer, and a thicker posterior layer that increases with age.Citation3 This explains the thin layer of DM noted on the host cornea histopathology and demonstrates the benefit of histopathology in highlighting the possibility of intraocular retained residual tissue. Histological analyses of corneas affected by FECD have shown stretching and thinning of endothelial cells in areas of guttata.Citation4 As the endothelial count decreases, an abnormally wide spaced collagen develops in the DM, resulting in its thickening. The abnormal corneal structure increases the risk of separation of the DM from the stroma during PK, therefore increasing the potential for retaining this layer post-operatively.
During corneal graft surgery, viscodissection of the host DM may occur during insertion of the ophthalmic viscoelastic device into the anterior chamber prior to trephine use. Incomplete trephination followed by use of scissors for excision of the host tissue may result in residual adhesions of the DM between the tissue for extraction and the peripheral cornea due to placement of the scissor blade anterior to the DM. Therefore, careful examination of the open anterior chamber and gentle elevation of the iris with forceps following excision of the host graft will reveal any residual overlying material within the anterior chamber.Citation5 Alternatively, a dye such as trypan blue or indocyanine green may be used intraocularly to highlight the DM.Citation6
Previous cases of DM retention have reported decreased visual acuity from 3 months post-operatively secondary to membrane opacification.Citation7 It is likely that this is due to a minimal amount of stroma remaining adherent to the DM, which subsequently activates the fibroblastic activity of keratocytes leading to opacification.Citation7
In the current literature, DM excision is recommended if the potential BCVA is limited in three circumstances: (a) if the membrane begins to opacify, (b) if the graft viability is compromised by contact with the retained tissue and, (c) if there is reduced diffusion and sequestration of aqueous between the DM and cornea resulting to an increased rate of endothelial cell loss.Citation5,Citation8
The treatment options available include the use of the neodymium-doped yttrium aluminum garnet (Nd:YAG) laser or surgical excision. The Nd:YAG laser is used to perform descematorhexis; ie, opening the membrane over the visual axis to improve visual acuity, encouraging aqueous circulation and the subsequent nutrient supply to the endothelial graft.Citation8 Surgical excision can be easily performed under local anesthetic. In our case, the graft endothelium was protected with viscoelastic and the membrane was easily removed with forceps. Surgical intervention proved successful as the graft remained healthy and clear and the patient achieved a mild improvement in BCVA. Care must be taken to minimize any further damage to the graft endothelial cells during surgical excision of retained DM. If the presence of a retained DM induces graft failure, DSAEK following membrane extraction will allow the donor tissue to adhere directly over the recipient endothelium and DM and a further PK could be avoided.Citation9
In conclusion, this case highlights the importance of considering the possibility of a retained DM as a differential diagnosis if there is poor visual acuity post-PK. It emphasizes the significance of informing the patient about this potential complication pre-operatively and the need of a high index of suspicion for the reviewing clinician when examining the anterior segment post-operatively. Techniques that help to minimize risks of this complication should be considered at the time of surgery. Histopathological evaluation as well as the use of IVCM in assessing graft adherence and endothelial integrity help in detecting and analyzing any retrocorneal membranes and graft detachments post DSAEK. Prompt extraction of the retained DM is not a commonly reported treatment and can be performed safely and easily with good results. Prophylactic surgical extraction is an important treatment option to be considered in these patients.
Acknowledgments
We would like to thank Dr James Mackenzie for his valuable help with the histopathological slides and the explanation that he offered.
Disclosure
The authors report no conflicts of interest in this work.
References
- SundaramVTraining in OphthalmologyOxfordOxford University Press2009
- JabsDANussenblattRBRosenbaumJTStandardization of uveitis nomenclature for reporting clinical data. Results of the First International WorkshopAm J Ophthalmol2005140350951616196117
- LevinLANilssonSFEver HoeveJWuSKaufmanPLAlmaAAdler’s physiology of the EyeNew YorkElsevier2011
- ElhalisHAziziBJurkunasUVFuchs endothelial corneal dystrophyOcul Surf20108417318420964980
- ChenYPLaiPCChenPYLinKKHsiaoCHRetained Descemet’s membrane after penetrating keratoplastyJ Cataract Refract Surg20032991842184414522313
- MondlochMCGiegengackMTerryMAWilsonDJHistologic evidence of retained fetal layer of the descemet membrane after presumed total removal for endothelial keratoplasty: a possible cause for graft failureCornea200726101263126618043188
- ThyagarajanSMearzaAAFalconMGInadvertent retention of Descemet Membrane in penetrating keratoplastyCornea200625674874917077674
- ChoiJSOhJYWeeWRA case of corneal endothelial deterioration associated with retained Descemet’s membrane after penetrating keratoplastyJpn J Ophthalmol200953665365520020249
- PriceFWPriceMOEndothelial keratoplasty to restore clarity to a failed penetrating graftCornea200625889589917102663
