Abstract
Purpose
To report the effect of wavefront-guided photorefractive keratectomy and corneal collagen cross-linking (CXL) on visual problems after Ferrara ring segment placement.
Materials and methods
A 32-year-old male patient was treated with a Ferrara ring segment for keratoconus. One year later, the ring was removed due to severe glare complaints. After 6 months, wavefront-guided photorefractive keratectomy and CXL were applied simultaneously to correct high order aberration and refractive error.
Results
Six months after the wavefront-guided photorefractive keratectomy and CXL, the uncorrected distance visual acuity was 20/25, and there was a 30% decrease in coma aberrations. The glare complaint regressed.
Conclusion
Wavefront-guided surface ablation and CXL may reduce high order aberrations and glare complaints after intrastromal corneal ring implantation.
Introduction
Intrastromal corneal ring segments (ICRS), which were initially designed to correct mild to moderate myopia, have been demonstrated as a surgical option to manage keratoconus.Citation1–Citation3 Its therapeutic effects are based on the induction of remodeling of the corneal anterior and posterior surface’s topography, which improves the optical quality of the cornea and reduces the optical aberrations, with consequent improvement in visual acuity.Citation4,Citation5
Currently there are many types of commercially available ICRSs, such as Intacs® (Addition Technologies, Des Plaines, IL, USA), Keraring (Mediphacos, Belo Horizonte, Brazil), and Ferrara ring (Ferrara Ophthalmics, Belo Horizonte, Brazil). The Ferrara intrastromal ring segment used in this study has a small radius of curvature and a triangular anterior surface.Citation6 The unique triangular shape with a flat posterior surface is purported to induce a prismatic effect on the cornea which reduces glare and halo.Citation7 However these complaints were reported in 10% of the Ferrara cases followed over a 5-year period.Citation8 Although these symptoms may disappear over time, pilocarpine or brimonidine tartrate drops are recommended for persistent cases. In addition, increase in high order aberrations (HOAs) after ICRS implantation is another problem that may affect visual quality.Citation9,Citation10
The photorefractive keratectomy (PRK) plus corneal collagen cross-linking (CXL) procedure is an effective treatment option for progressive keratoconus. This procedure was found to be associated with stable refractive and topographic outcomes and with a reduction in corneal aberrations.Citation11 Herein, we describe a case of visual complaint after Ferrara ring segment placement, which was treated successfully with wavefront-guided PRK and CXL procedures after the ring was extracted.
Case report
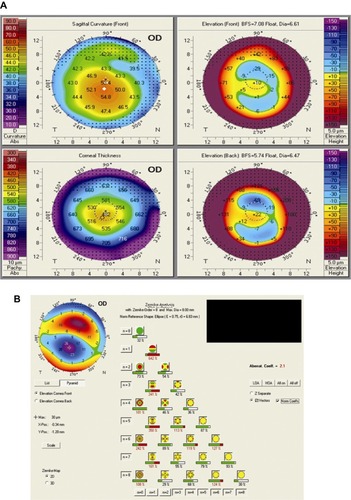
A 32-year-old male patient was referred to our department from an ophthalmology clinic, with bilateral keratoconus. He worked with heavy metals and could not use contact lenses or eyeglasses on the job. His uncorrected distance visual acuity was 20/200 and corrected distance visual acuity was 20/100 with −5.00 −2.50 × 30° in the right eye. The uncorrected distance visual acuity was 20/70 and corrected distance visual acuity was 20/40 with −2.50 −2.00 × 175° in the left eye. The slitlamp examination and intraocular pressure and examination were normal for both eyes. Corneal topographical findings measured with Pentacam corneal topography system (Oculus Opticgerate GmbH, Wetzlar, Germany) revealed a keratoconus pattern in both eyes (). In the corneal wavefront map, measured with the WaveScan WaveFront™ System (Abbott Medical Optics, Santa Ana, CA, USA), primary and secondary vertical coma dominance was observed (). The aberrometry analyses under scotopic condition were based on a pupil diameter of 6 mm. The scotopic pupil diameter, measured with the Colvard pupilometer (Oasis Medical Inc, San Dimas, CA, USA), was 6 mm.
Figure 1 Corneal topography and wavefront aberration measurements prior to the ring placement.
Abbreviation: OD, right eye.
In an attempt to improve vision, Ferrara ICRS implantation was planned for the correction of the corneal steepening and irregularity. Two Ferrara ring segments with 250 μm thickness and 160° arch-length were to be placed temporally and nasally using a 30 kHz femtosecond laser (IntraLase™ FS Laser, Abbott Medical Optics,) in compliance with the Ferrara nomogram in the right eye. The Purkinje reflex was chosen as the central point. The patient rejected treatment of the left eye. After Ferrara ring segment implantation, the corrected distance visual acuity was 20/40 with optimal centralization of the ring segments ( and ). However the patient had severe light glare complaints under photopic conditions in his right eye. Corneal topography revealed diminishing keratometric values (), and the Zernike analysis with Pentacam (Oculus Opticgerate GmbH) showed an increase in vertical coma and trefoil (). Twelve months use of brimonidine drops did not eliminate this complaint. After 1 year, the rings were removed but the glare persisted. The aberrometric measurements taken from the right eye by WaveScan demonstrated that HOA root mean square error was 0.75 μm and coma domination was 0.404 μm (). Based on these results, wavefront-guided PRK along with CXL was planned to correct refractive errors and aberrations of the right eye.
Figure 2 Imaging of cornea after ring implantation.
Abbreviation: OD, right eye.
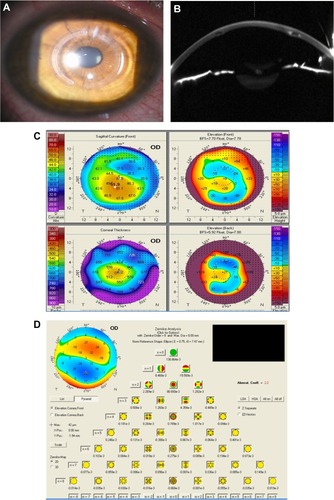
Figure 3 Wavefront analyses shows HOAs and total coma aberration continues 1 year after the ring segment removal (A). Six months after wavefront-guided PRK and CXL, wavefront analyses shows reduction in HOAs and coma aberrations (B). One year after wavefront-guided PRK and CXL, corneal topography (C) and wavefront analyses (D) show stability in keratometric and aberrometric values.
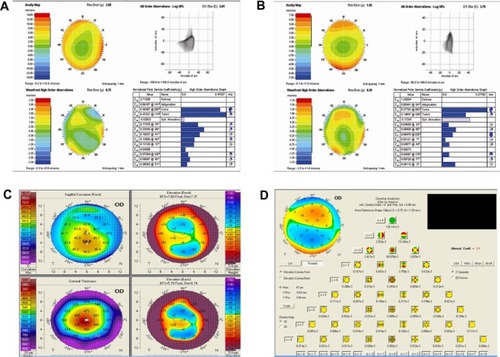
The wavefront-guided ablation pattern was prepared using a WaveScan aberrometer and transferred to a VISX S4 IR device (Abbott Medical Optics, Santa Ana, California, USA). Estimated ablation depth was 50 μm. Mitomycin-c (Onko Ecza Sanayi ve Tic. Ltd., Sti., Istanbul, Turkey) at 0.02% was applied for 20 seconds to impede haze and regression. Following PRK, CXL was applied in compliance with the Dresden protocol.Citation12 A 6.5 mm optical zone was used with a transition zone of 8.5 mm. Six months after Wavefront-guided PRK and CXL procedures, the uncorrected distance visual acuity was 20/25. The high order root mean square score was drawn back to 0.39 μm, and coma aberration was reduced to 0.277 μm (). The patient’s glare complaints ceased, and no haze was seen. At the 12 month visit, refractive status, visual acuity, wavefront analyses, and topograpgical measurements were unchanged ( and ).
Discussion
Visual problems such as glare and halo are two of the expected complications after ICRS implantation, and it may adversely affect daily activities. Although no comprehensive studies have been conducted on glare and halo after ICRS implantation, one study showed that 10% of the Ferrara cases had halo complaint after surgery, and it has been associated with pupil size.Citation8 In our case, glare complaint could not be explained by pupil size, which was 6 mm. We hypothesized that the cause of glare might be HOAs, and studies have shown increases in HOAs after ICRS implantation.Citation9,Citation10 HOAs can also have a significant impact on one’s quality of vision and are often linked to visual glare and halos.
Glare symptom tends to get better over time. In severe cases, nighttime application of pilocarpine or brimonidine tartrate drops may be prescribed in order to constrict the pupil and alleviate undesired reflexes. Also Torquetti et al developed segments with a yellow filter in the matrix to avoid blue light at night, which can significantly decrease the incidence of glare and halos.Citation8 In our study, after ICRS had been extracted, a combination treatment including wave-front guided PRK and CXL was applied to the patient. We achieved a reduction in HOAs and an improvement in glare symptom.
A few studies have reported the use of CXL along with topography-guided PRK in order to provide better visual rehabilitation in patients with keratoconus.Citation13–Citation17 Moreover, only one study, carried out by Kremer et al, has reported the use of wavefront-guided PRK along with CXL in keratoconic eyes.Citation18 As we considered that our patient’s glare symptom was associated with HOAs, we performed wavefront-guided PRK.
In summary, this report contributes new information to the literature. First, a severe glare complaint that is resistant to medical therapy may present after ICRS implantation. Second, symptoms of glare and HOAs may persist after the removal of ICRS. Lastly, wavefront guided PRK and CXL treatment may yield a reduction in HOA and an improvement of glare symptom in a keratoconic eye that has undergone ICRS extraction.
Disclosure
No financial support was provided for this study. This manuscript has been read and approved by all the authors. The authors report no conflicts of interest in this work.
References
- ColinJCochenerBSavaryGMaletFHolmes-HigginDINTACS inserts for treating keratoconus; one-year resultsOphthalmology200110881409141411470691
- ColinJCochenerBSavaryGMaletFCorrecting keratoconus with intracorneal ringsJ Cataract Refract Surg20002681117112211008037
- SiganosCSKymionisGDKartakisNTheodorakisMAAstyrakakisNPallikarisIGManagement of keratoconus with IntacsAm J Ophthalmol20031351647012504699
- ShabayekMHAlióJLIntrastromal corneal ring segment implantation by femtosecond laser for keratoconus correctionOphthalmology200711491643165217400293
- AlióJLShabayekMHArtolaAIntracorneal ring segments for keratoconus correction: long-term follow-upJ Cataract Refract Surg200632697898516814056
- KwitkoSSeveroNSFerrara intracorneal ring segments for keratoconusJ Cataract Refract Surg200430481282015093643
- SiganosDFerraraPChatzinikolasKBessisNPapastergiouGFerrara intrastromal corneal rings for the correction of keratoconusJ Cataract Refract Surg200228111947195112457667
- TorquettiLBerbelRFFerraraPLong-term follow-up of intrastromal corneal ring segments in keratoconusJ Cataract Refract Surg200935101768177319781474
- PiñeroDPAlióJLEl KadyBRefractive and aberrometric outcomes of intracorneal ring segments for keratoconus: mechanical versus femtosecond-assisted proceduresOphthalmology200911691675168719643498
- ChalitaMRKruegerRRWavefront aberrations associated with the Ferrara intrastromal corneal ring in a keratoconic eyeJ Refract Surg200420682383015586766
- AlessioGL’abbateMSborgiaCLa TegolaMGPhotorefractive keratectomy followed by cross-linking versus cross-linking alone for management of progressive keratoconus: two-year follow-upAm J Ophthalmol20131551546523022158
- SpoerlEMrochenMSlineyDTrokelSSeilerTSafety of UVA-riboflavin cross-linking of the corneaCornea200726438538917457183
- KrumeichJHKezirianGMCircular keratotomy to reduce astigmatism and improve vision in stage I and II keratoconusJ Refract Surg200925435736519431926
- KanellopoulosAJBinderPSCollagen cross-linking (CCL) with sequential topography-guided PRK: a temporizing alternative for keratoconus to penetrating keratoplastyCornea200726789189517667633
- KymionisGDKontadakisGAKounisGASimultaneous topography-guided PRK followed by corneal collagen cross-linking for keratoconusJ Refract Surg2009259S807S81119772256
- KanellopoulosAJComparison of sequential vs same-day simultaneous collagen cross-linking and topography-guided PRK for treatment of keratoconusJ Refract Surg2009259S812S81819772257
- Al-TuwairqiWSinjabMMIntracorneal ring segments implantation followed by same-day topography-guided PRK and corneal collagen CXL in low to moderate keratoconusJ Refract Surg2013291596323311743
- KremerIAizenmanILichterHShayerSLevingerSSimultaneous wavefront-guided photorefractive keratectomy and corneal collagen crosslinking after intrastromal corneal ring segment implantation for keratoconusJ Cataract Refract Surg201238101802180722858060