Abstract
Background
Patients with angioid streaks are prone to develop a subretinal hemorrhage after ocular injury, due to fragility of Bruch’s membrane.
Objective
The purpose of this study was to report a patient with angioid streaks in whom subfoveal choroidal neovascularization (CNV) developed after blunt ocular trauma.
Case report
A 60-year-old man was accidentally struck in the left eye with a crowbar handle while engaged in the demolition of wooden building materials in May 2011 and was initially evaluated at our hospital. Corrected visual acuity was 0.3 in the right and 1.2 in the left eye, and relative afferent pupillary defect was negative. Funduscopy revealed choroidal atrophy around the optic papillae and angioid streaks radiating from around the optic discs in both eyes. In the right eye, there was macular atrophy. In the left eye, there was a subretinal hemorrhage around the macular region. Fluorescein angiography of the left eye showed a blockage due to subretinal hemorrhage and increasing hyperfluorescent spots superior to the fovea, suggestive of extrafoveal CNV. Spectral-domain optical coherence tomography showed macular thinning in the right eye and no obvious abnormalities near the subfoveal region in the left eye. Two months later, the patient noticed decreased visual acuity in the left eye and was reevaluated. Visual acuity had decreased to 0.7, and well-defined CNV, one disc diameter in size, was presenting slightly superior to the macula, including the subfoveal region. Two weeks later, anti–vascular endothelial growth factor (anti-VEGF) antibody (bevacizumab) was injected intravitreally; the CNV then regressed, and visual acuity improved to 1.2.
Conclusion
Marked improvement in visual acuity with early treatment has not been reported in angioid streaks with subfoveal CNV after ocular injury. Intravitreal injection of an anti-VEGF antibody should be considered early after the diagnosis of CNV.
Introduction
Angioid streaks (AS) are characterized by linear irregularities radiating from around the optic disc due to a weakening or rupture of Bruch’s membrane, elastic fiber degeneration, or calcium deposition at the same site. If these streaks reach the macular region, choroidal neovascularization (CNV) will occur under the macular region, resulting in severe visual impairment. CNV occurs in 72%–86% of cases of AS,Citation1,Citation2 and the Gass type II CNV seen in exudative age-related macular degeneration is common.
Significant visual impairment reportedly develops in 15% of patients with AS who suffer head trauma,Citation3 and regular examination is required to assess changes before and after injury. As far as we have been able to determine, few reports have described the development of CNV after blunt trauma in AS patients.
We report herein a case in which an AS patient who developed CNV after blunt trauma was treated with intravitreal injection of bevacizumab, an anti–vascular endothelial growth factor (anti-VEGF) antibody, soon after onset of CNV, resulting in improved visual acuity.
Case report
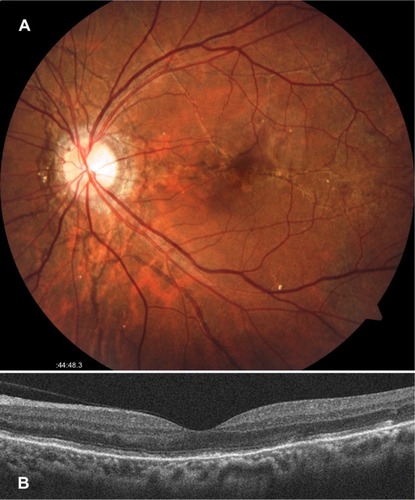
In May 2011, a 60-year-old man was accidentally hit in the left eye with a crowbar handle while engaged in the demolition of wooden building materials and underwent initial examination in our department on the same day. He was not wearing eye protection at the time of the trauma. His medical history included a fundal hemorrhage after having been hit in the right eye 3–4 years earlier. His family history was unremarkable. On initial examination, his best corrected visual acuity (BCVA) was 0.3 (with −1.50 diopters) in the right eye and 1.5 (with −3.00 diopters) in the left eye. The intraocular pressure was 15 mmHg on the right and 22 mmHg on the left. Light reflex was rapid in both eyes, and relative afferent pupillary defect was negative. Examination of the anterior segments showed a slight presence of inflammatory cells only in the left anterior chamber. Fundal examination revealed choroidal atrophy around the optic papillae and AS radiating from around the optic discs in both eyes. Atrophic changes to the macular region were evident in the right eye, and a subretinal hemorrhage was apparent around the macular region in the left eye ( and ).
Figure 1 Fundus findings on initial examination.
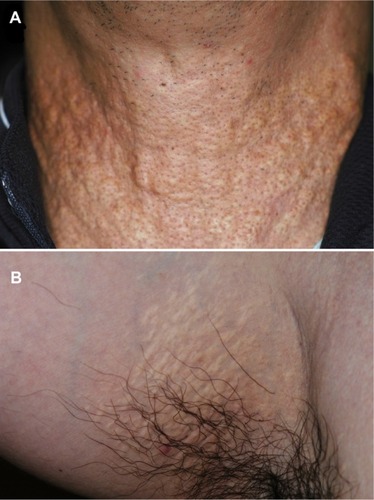
Two weeks later, fluorescein angiography (FA) (VISUCAMNM/FA; Carl Zeiss Meditec AG, Jena, Germany) was performed. The middle phase FA image of the right eye showed tissue staining and a window defect in the macular region (). The early phase FA image of the left eye revealed signs of blocking due to subretinal hemorrhage and hyperfluorescent spots due to early leakage superior to the fovea (). Additionally, the FA images of the middle () and late () phases showed increasing hyperfluorescence due to the leakage, suggestive of extrafoveal CNV. Spectral-domain optical coherence tomography (OCT) (Cirrus™ HD-OCT Model 4000; Carl Zeiss Meditec AG) using the HD 5-line raster scan protocol (horizontal scan of 6 mm) revealed thinning of the central retina with subretinal tissue in the right eye (), but no obvious abnormality was seen in the neighborhood of the fovea in the left eye (). Examination of the skin revealed characteristic skin lesions on the neck () and axillae on both the right () and left side, suggestive of pseudoxanthoma elasticum.
Figure 2 Appearance of the skin.
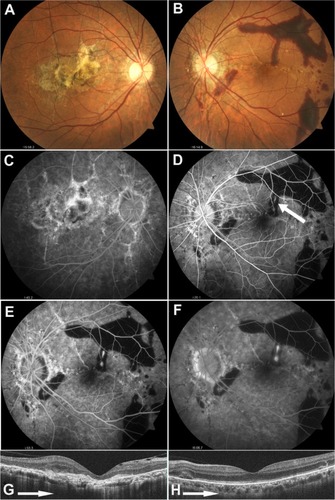
The subretinal hemorrhage in the left eye was subsequently absorbed, but 2 months after the injury, the patient became aware of metamorphopsia in the left eye. One month later (3 months after the injury), BCVA in the patient’s left eye had decreased to 0.7, and well-defined CNV, one disc diameter in size, was evident somewhat above the macular region (). The extrafoveal CNV, which had developed superior to the fovea, progressed to a subfoveal location. OCT demonstrated that CNV was clearly located in the juxtafoveal () and subfoveal () regions, extending across the retinal pigment epithelial line into the retina, resulting in Gass type II CNV. FA revealed well-defined, predominantly classic CNV in the early phase () and a high level of fluorescein leakage coincident with CNV in the late phase (). CNV was also visualized on indocyanine green angiography (VISUCAMNM/FA) from the early phase () to the late phase ().
Figure 3 Left fundus findings 3 months after injury.
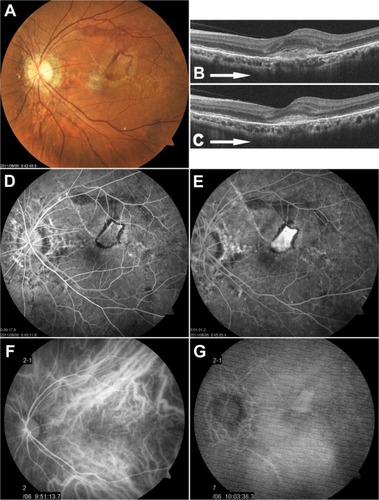
Two weeks later (3.5 months after injury), as visual impairment persisted in the left eye, intravitreal injection of 1.25 mg/0.05 mL bevacizumab (Avastin®; Genentech, South San Francisco, CA, USA) was administered. The offlabel use of bevacizumab was approved by the Institutional Review Board of The Jikei University. Visual acuity gradually improved and by approximately 2 months after starting intravitreal bevacizumab (IVB) had recovered to 1.2 in the left eye, with pronounced regression of the CNV () and disappearance of the subfoveal CNV (). As of 1 year later, no further visual impairment has appeared.
Discussion
In the present patient, who had both AS and pseudoxanthoma elasticum, although visual acuity was excellent immediately after the blunt trauma, extrafoveal CNV appeared within 2 weeks after injury, and visual acuity decreased. No previous case reports have described improvements in visual acuity due to early administration of an anti-VEGF agent for CNV occurring after blunt injury in an AS patient. Pandolfo et alCitation4 reported a case in which the use of laser photocoagulation was attempted to treat extrafoveal CNV that appeared 4 months after blunt trauma, but subfoveal CNV recurred, and a fibrous scar developed. Alpay and CaliskanCitation5 reported that pronounced visual impairment, due to a fibrous lesion in the fovea, occurred 3 weeks after injury in an AS patient who had a macular subretinal hemorrhage and optic disc edema after blunt trauma, despite treatment with oral corticosteroids. De Benedetto et alCitation6 described an AS patient with a loss of visual acuity and extrafoveal CNV originating from choroidal rupture in the left eye, who had suffered from ocular blunt trauma 1 year earlier, and reported that visual acuity in this patient remained unchanged after IVB injection. Although some reports have described the occurrence of subretinal hemorrhage following blunt trauma in AS patients,Citation4,Citation5,Citation7,Citation8 the subsequent incidence of CNV is not necessarily high.
Reported treatment for CNV, as a complication of AS that is unrelated to ocular injury, include photodynamic therapyCitation9–Citation11 and intravitreal injection of the anti-VEGF antibodies bevacizumabCitation12–Citation16 and ranibizumab.Citation17,Citation18 Photodynamic therapy has a short-term effect and may help prevent visual impairmentCitation9,Citation10 but has also been reported to cause enlargement of scarring and loss of vision over the long term.Citation11 According to the majority of reports,Citation12–Citation18 bevacizumab and ranibizumab are effective in maintaining and improving vision over both the short and long terms, but often, repeated injections are needed. In the present case, we administered a single injection of IVB. CNV regressed after the injection, and marked improvements in visual acuity became evident, indicating that a single IVB injection was useful.
Conclusion
In the present case, a subretinal hemorrhage was evident immediately after injury, but extrafoveal CNV, which developed 2 weeks after injury, progressed to a subretinal location within 3 months after injury. It is important that construction workers who suffer from AS always wear goggles or other eye protection to protect their eyes while working because CNV may develop after blunt ocular trauma. When CNV develops, the administration of intravitreal anti-VEGF antibody as soon as possible should be considered.
Acknowledgments
This study was supported by grants from the Ministry of Health, Labor and Welfare of Japan (TH) and the Vehicle Racing Commemorative Foundation (TH and HT).
Disclosure
The authors report no conflicts of interest in this work.
References
- ConnorPJJrJuergensJLPerryHOHollenhorstRWEdwardsJEPseudoxanthoma elasticum and angioid streaks. A review of 106 casesAm J Med19613053754313695083
- ShieldsJAFedermanJLTomerTLAnnesleyWHJrAngioid streaks. I. Ophthalmoscopic variations and diagnostic problemsBr J Ophthalmol19755952572661138852
- GeorgalasIPapaconstantinouDKoutsandreaCAngioid streaks, clinical course, complications, and current therapeutic managementTher Clin Risk Manag200951818919436620
- PandolfoAVerrastroGPiccolinoFCRetinal hemorrhages following indirect ocular trauma in a patient with angioid streaksRetina200222683083112476123
- AlpayACaliskanSSubretinal hemorrhage in a soccer player: a case report of angioid streaksClin J Sport Med201020539139220818200
- De BenedettoUBattaglia ParodiMKnutssonKAIntravitreal bevacizumab for extrafoveal choroidal neovascularization after ocular traumaJ Ocul Pharmacol Ther201228555055222554238
- BrittenMJUnusual traumatic retinal haemorrhages associated with angioid streaksBr J Ophthalmol19665095405425919263
- LevinDBBellDKTraumatic retinal hemorrhages with angioid streaksArch Ophthalmol197795610721073869751
- KaracorluMKaracorluSOzdemirHMatCPhotodynamic therapy with verteporfin for choroidal neovascularization in patients with angioid streaksAm J Ophthalmol2002134336036612208247
- MenchiniUVirgiliGIntroiniUOutcome of choroidal neovascularization in angioid streaks after photodynamic therapyRetina200424576377115492632
- HeimannHGeliskenFWachtlinJPhotodynamic therapy with verteporfin for choroidal neovascularization associated with angioid streaksGraefes Arch Clin Exp Ophthalmol2005243111115112315947939
- TeixeiraAMoraesNFarahMEBonomoPPChoroidal neovascularization treated with intravitreal injection of bevacizumab (Avastin) in angioid streaksActa Ophthalmol Scand200684683583617083556
- PedersenRSolimanWLund-AndersenHLarsenMTreatment of choroidal neovascularization using intravitreal bevacizumabActa Ophthalmol Scand200785552653317511757
- RinaldiMDell’OmoRRomanoMRChiosiFCipolloneUCostagliolaCIntravitreal bevacizumab for choroidal neovascularization secondary to angioid streaksArch Ophthalmol2007125101422142317923555
- BhatnagarPFreundKBSpaideRFIntravitreal bevacizumab for the management of choroidal neovascularization in pseudoxanthoma elasticumRetina200727789790217891014
- WiegandT WRogersAHMcCabeFReichelEDukerJSIntravitreal bevacizumab (Avastin) treatment of choroidal neovascularisation in patients with angioid streaksBr J Ophthalmol2009931475118971238
- FingerRPCharbel IssaPHendigDSchollHPHolzFGMonthly ranibizumab for choroidal neovascularizations secondary to angioid streaks in pseudoxanthoma elasticum: a one-year prospective studyAm J Ophthalmol2011152469570321704964
- ShahMAmoakuWMIntravitreal ranibizumab for the treatment of choroidal neovascularisation secondary to angioid streaksEye (Lond)20122691194119822722486