Abstract
Purpose
To compare Barrett TK Universal II and Barrett Universal II TCRP calculations in the power calculations for 3 presbyopia-correcting intraocular lenses (PC-IOL).
Methods
This observational study involved 64 eyes from 64 patients who prepared to undergo extraction of crystalline lenses combined with PC-IOL (Symfony ZXR00, PanOptix TFNT00, or AT LISA tri 839MP) implantation. All eyes underwent ocular biometric measurements with IOLMaster 700 and Pentacam HR, and the interdevice agreement of measurements including total keratometry (TK, IOLMaster 700) and total corneal refractive power (TCRP, Pentacam HR) was evaluated. IOL power calculations were performed using TK-based Barrett TK Universal II and TCRP-based Barrett Universal II calculations, respectively.
Results
Paired t-tests showed that the differences in white-to-white diameter, central corneal thickness, anterior chamber depth, and mean TK between IOLMaster 700 and Pentacam HR were slight but significant (all P<0.05), and the differences in recommended IOL power for emmetropia between two Barrett calculations were also significant in 3 PC-IOLs (all P<0.05). The ROC curve showed that the AUC was 0.917 (95% CI, 0.820–0.971) for the absolute value of the difference between TK and TCRP in discriminating the difference of ≥ ±0.5 D in predicted IOL power with best cutoff values of 0.4 D.
Conclusion
The novel Barrett TK Universal II formula built in IOLMaster 700 is comparable to TCRP-based Barrett Universal II calculation for IOL power calculation of PC-IOLs, and the convenience of using the Barrett TK Universal II formula should be founded on measurement consistency between devices.
Introduction
Presbyopia is characterized by loss in physiological accommodation and causes an inability to focus on nearby objects, which affects over a billion people worldwide.Citation1 One current therapeutic option is the extraction of crystalline lenses combined with the implantation of a presbyopia-correcting intraocular lens (PC-IOL).Citation2 In response to increasing demand for spectacle independence, new-generation PC-IOLs are designed to provide more focus for all near, intermediate, and distance vision compared with traditional diffractive or refractive bifocal IOLs. Consequently, the precision of surgery grows in importance. Apart from advanced surgical techniques, modern biometry and the new generation of formulas are two other crucial determinants. Novel IOL calculation formulas have emerged to improve the accuracy of predicted refraction, among which the Barrett Universal II formula is outstanding because of its overall reliability and universality in eyes with axial length (AL) of not shorter than 22.0 mm, and special keratometry,Citation3–7 so it has become an optimal choice for some surgeons when PC-IOL implantation is performed.Citation8
In Barrett Universal II formula version, AL and keratometry are the essential measurements,Citation9 while the anterior chamber depth (ACD), the white-to-white corneal diameter (WTW) and the lens thickness (LT) are also recommended for the more accurate results, especially in short eyes.Citation10 Therefore, in clinical practice, a whole set of preoperative measurements with several combined devices might be the preferred strategy. It increases chances to obtain the parameters as comprehensive as possible, and approximate parameters from different devices could also corroborate each other. The development of measuring techniques makes results more accurate and brings more options; however, it inevitably aggravates the workload and the burden on both physicians and patients. On the other hand, a problem is that the measurement results might not be interchangeable between devices, and much work has been done in previous studies to interpret the measurement errors of different types of devices.Citation11,Citation12
In recent years, total keratometry (TK) has become a new function of IOL Master 700, and the Barrett TK Universal II formula is the built-in formula of IOLMaster 700 designed for use only with the TK value.Citation13 Studies showed that the Barrett TK Universal II formula would be more precise, or at least comparable in IOL power calculation than the built-in Barrett Universal II formula, which employs standard anterior keratometry.Citation13–16 There were also documents about Barrett Universal II formula that employs Scheimpflug tomography-based total corneal refractive power (TCRP) for IOL power calculation provided excellent outcomes.Citation17–19 To our knowledge, the agreement and accuracy in IOL power calculation between the novel Barrett TK Universal II formula and Barrett Universal II formula using TCRP is unclear. Thus, we conducted the present study to evaluate the total corneal power of IOLMaster 700 and Pentacam HR and compare Barrett TK Universal II and Barrett Universal II TCRP power calculations for 3 classical PC-IOLs.
Methods
Ethics
This observational study was conducted at Shanghai Aier Eye Hospital. All study procedures were performed in accordance with the tenets of the Declaration of Helsinki and its amendments. The ethics committee of Aier Eye Hospital Group Co. Ltd. approved this study (IRB-SHAIER202205). Written informed consent was obtained from all participants for the usage and publication of their clinical data.
Data and Eligibility
Patients who prepared to undergo the extraction of crystalline lenses combined with the implantation of a PC-IOL between January 2022 and December 2022 in Shanghai Aier Eye Hospital were screened for possible inclusion. Some patients were excluded from the data analysis according to the criteria described below:
1) History of corneal refractive surgery, keratoconus, or dystrophies;
2) History of ocular trauma or intraocular surgery;
3) Possible zonular dehiscence or crystalline lens subluxation;
4) Poor compliance with ocular examinations.
Only one randomly assigned eye was included per patient, even if both eyes fit for inclusion. After enrolling in this study, eyes received complete preoperative measurements, including biometry with the IOLMaster (Model 700, Carl Zeiss Meditec Ltd, Jena, Germany, Software Version 1.88.1.64861) and Scheimpflug device imaging (Pentacam HR, Oculus Optikgeräte GmbH, Wetzlar, Germany, Software Version 1.21r43). Data acquisition was according to the user guidelines of each device, and effective measurements (measurement quality checklist items were assessed as “OK” for Pentacam HR, and all readings were normal for IOLMaster 700) were used in the final analysis.
A trifocal IOL, AT LISA tri (model 839MP, Carl Zeiss Meditec AG), a trifocal/quadrifocal IOL, AcrySof IQ PanOptix (model TFNT00, Alcon Laboratories Inc., Fort Worth, USA), and an extended depth of focus (EDOF) IOL, Tecnis Symfony (model ZXR00, Johnson & Johnson Surgical Vision Inc., Santa Ana, USA), were used as the candidate PC-IOLs for power calculation. The lens factor (LF) values were +1.83, +1.94, and +2.09, respectively, according to the manufacturers. Barrett TK Universal II calculations were obtained using the IOLMaster 700 system built-in Barrett Suite. The Barrett Universal II calculations using TCRP were obtained via an online calculator (http://calc.apacrs.org/barrett_universal2105/). In the Barrett Universal II calculations, AL, ACD, LT, and WTW were according to the measurements in IOLMaster 700, and K1 (flat K of cornea) and K2 (steep K of cornea) were based on the TCRP of a central 4 mm in Pentacam HR. The recommended IOL power for emmetropia was compared.
Statistical Analysis
The Kolmogorov‒Smirnov test was used to assess data normality. To assess the interdevice agreement between IOLMaster 700 and Pentacam HR, Bland‒Altman plots with 95% limits of agreement (LoA) and paired t-tests were performed using MedCalc Statistical Software (version 15.2.2; MedCalc Software, Inc., Mariakerke, Belgium). A univariable linear regression model was used to determine factors associated with the absolute value of the difference in the recommended IOL power for emmetropia. The receiver operating characteristic (ROC) curve and area under the curve (AUC) were used as indices to test the predictive ability to detect a significant difference (greater than 0.5 D) in the recommended IOL power for emmetropia between Barrett TK Universal II calculations and Barrett Universal II TCRP calculations. The level of statistical significance was set at a P value of less than 0.05.
Results
Demographic Data
As presented in , a total of 64 eyes from 64 consecutive patients were included in the final study. Their mean age was 58.0±11.1 years, and 31 of the patients were female. Among the eyes, there were 32 right eyes and 32 left eyes. The average AL measured with IOLMaster 700 was 24.59±1.96 mm, the average central corneal thickness (CCT) was 540.48±34.09 μm, the average ACD was 3.11±0.43 mm, the average LT was 4.38±0.42 mm, the average WTW was 11.92±0.46 mm, and the average total spherical equivalent of cornea (TSE) was 43.51±1.52 D, respectively.
Table 1 The Demographic Data and Biometric Parameters (N = 64, Measured with IOLMaster 700)
Agreement Between IOLMaster 700 and Pentacam HR Measurements
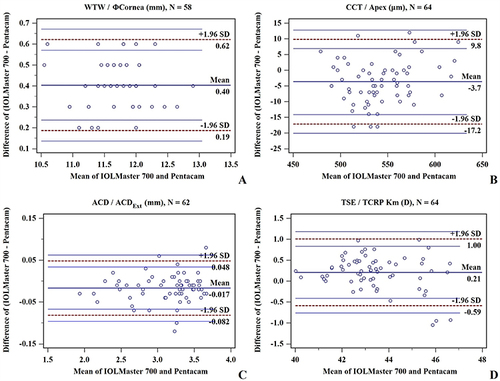
In the Pentacam HR measurements, the average corneal thickness at the apex was 544.17±32.70 μm (range, 476–620, N = 58), the average ACDExt was 3.13±0.43 mm (range, 1.95–3.68, N = 62), the average corneal diameter was 11.51±0.45 mm (range, 10.3–12.7, N = 64), and the average TCRP Km was 43.31±1.62 D (range, 39.9–47.1, N = 64), respectively. shows the Bland‒Altman plots (mean difference vs average) of measurements between IOLMaster 700 and Pentacam HR, and the pairwise agreements of all parameters were high for at least 95% of cases contained in 95% LoA. Paired t-tests showed that the differences in CCT, ACD, WTW, and TSE between IOLMaster 700 and Pentacam HR were slight but significant (all P < 0.05, ).
Table 2 The Comparison of Measurements Between IOLMaster 700 and Pentacam HR
Barrett TK Universal II Vs Barrett Universal II TCRP
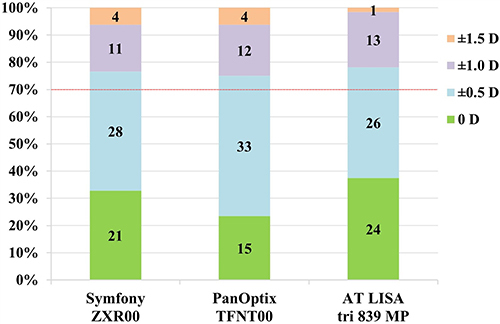
For all three PC-IOLs, the Bland‒Altman plots showed that agreement of recommended IOL power for emmetropia between Barrett TK Universal II and Barrett Universal II TCRP calculations was high (61/64 in 95% LoA). Paired t-tests revealed that the differences in the recommended IOL power for emmetropia between the two calculations were significant (all P < 0.05), and the recommended IOL power for emmetropia of Barrett TK Universal II calculations was lower than that of Barrett Universal II TCRP calculations for all three PC-IOLs (). To evaluate the associated factors for the absolute value of the difference in the recommended IOL power for emmetropia between Barrett TK Universal II and Barrett Universal II TCRP calculations, univariable linear regression was applied, and a model showed that CCT and TSE were positively correlated with the absolute value of the difference in the recommended IOL power for emmetropia (both P < 0.05, ). Considering that keratometry was the only variable between the two calculations, the univariable linear regression model showed that the absolute value of the difference between TSE and mean TCRP was strongly correlated with the absolute value of the difference in the recommended IOL power for emmetropia (r = 0.87, P < 0.05, ). We set an absolute value of the difference in the recommended IOL power for emmetropia between Barrett TK Universal II and Barrett Universal II TCRP calculations of less than 0.5 D as insignificant, and the ROC curve showed excellent discriminating performance of the absolute value of the difference between TSE and mean TCRP (). The AUC was 0.917 (P < 0.001, 95% CI, 0.820–0.971), with best cutoff values of 0.4 D for the absolute value of the difference in the recommended IOL power for emmetropia of ≥0.5 D. We further tested the correlations between CCT, TSE and the absolute value of the difference between TSE and mean TCRP, only TSE (r = 0.39, P < 0.05) but not CCT (r = 0.25, P > 0.05) was significantly correlated with the absolute value of the difference between TSE and mean TCRP ( and ). As shown in , more than 70% of cases finally received a difference of ±0.5 D or 0 D in the actually selected IOL power between Barrett TK Universal II and Barrett Universal II TCRP calculations.
Figure 2 Comparison of the recommended IOL power for emmetropia between Barrett TK Universal II and Barrett Universal II TCRP calculations. Bland–Altman plots showing agreement of the recommended IOL power for (A) Symfony ZXR00; (B) PanOptix TFNT00; and (C) AT LISA tri 839MP. (D) Paired t-tests showed that the differences in the recommended IOL power for emmetropia between Barrett TK Universal II and Barrett Universal II TCRP calculations for all three PC-IOLs were significant (* all P < 0.05).
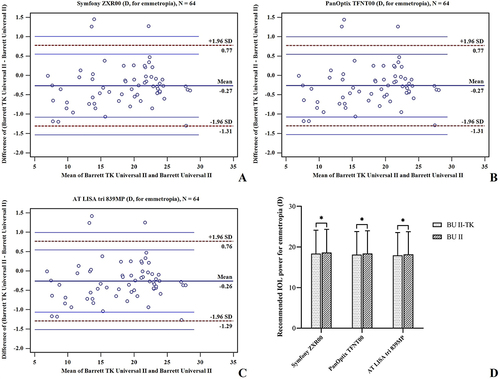
Figure 3 Correlation of the ocular measurements and the absolute value of the difference in the recommended IOL power for emmetropia between Barrett TK Universal II and Barrett Universal II TCRP calculations. (A) AL, r = 0.09, P > 0.05. (B) ACD, r = 0.11, P > 0.05. (C) LT, r = 0.04, P > 0.05. (D) WTW, r = −0.23, P > 0.05. (E) CCT, r = −0.29, P < 0.05. (F) TSE, r = 0.42, P < 0.05.
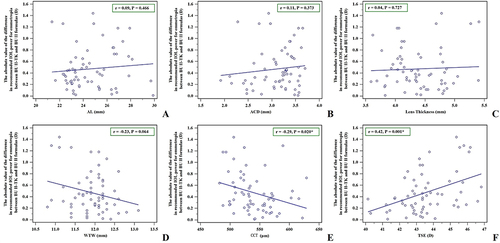
Figure 4 (A) The correlation of the absolute value of the difference between TSE and TCRP Km and the absolute value of the difference in the recommended IOL power for emmetropia between Barrett TK Universal II and Barrett Universal II TCRP calculations was significantly positive (r = 0.87, P < 0.05). (B) ROC curve of the absolute value of the difference between TSE and mean TCRP in discriminating the absolute value of the difference in the recommended IOL power for emmetropia of ≥ 0.5 D, and the AUC was 0.917 (P < 0.05, 95% CI, 0.820–0.971) with best cutoff values of 0.4 D. (C) Correlation of CCT and the absolute value of the difference between TK and TCRP (r = −0.25, P > 0.05). (D) Correlation of TSE and the absolute value of the difference between TK and TCRP (r = 0.39, P < 0.05).
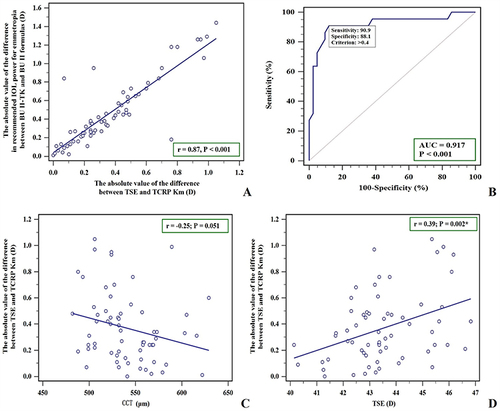
Figure 5 Stacked histogram comparing the percentages of eyes (N = 64) within differences of 0 D, ±0.5 D, ±1.0 D, and ±1.5 D in IOL power selection between Barrett TK Universal II and Barrett Universal II TCRP calculations among 3 PC-IOLs. More than 70% of cases finally received a difference of ±0.5 D or 0 D in the actually selected IOL power between Barrett TK Universal II and Barrett Universal II TCRP calculations.
Discussion
PC-IOLs have allowed correction not only for sphero-cylindrical refractive errors but also for presbyopia errors. They aim to improve uncorrected near and intermediate visual acuity without compromising uncorrected distance visual acuity. AT LISA tri 839MP, PanOptix TFNT00, and Symfony ZXR00 are representative of current PC-IOLs. Many studies have shown that all 3 frequently used PC-IOLs can achieve good visual performance and high patient satisfaction.Citation20,Citation21 However, their advantages are widely based on precise implantation and accurately determined IOL power. As reported by Melles, up to 81% and 98% of eyes using new-generation IOL calculation formulas finally obtained a prediction error within ±0.5 D and ±1.0 D, respectively, and in this work, the Barrett Universal II formula had the lowest postoperative refraction prediction error.Citation3 Zhao et al also reported that the Barrett Universal II has the best refractive prediction outcomes comparing with SRK/T, Haigis and Holladay 2 formulas.Citation16 Therefore, Shajari et al recommended the Barrett Universal II formula for PC-IOLs because of its accurate prediction.Citation9
In the last decade, TCRP has taken special importance and been regarded as the optimal choice for IOL power calculation due to the advent of Scheimpflug equipment, which enabled us to physically measure the posterior corneal curvature.Citation22 Traditional Placido-disc corneal topographer devices measure the curvature radius of the anterior corneal surface and convert it into refractive power of the whole cornea by estimating the power of the posterior corneal surface.Citation22 It was found that the standard keratometric corneal power, usually calculated using the keratometric index of 1.3375, and TCRP, measured by ray tracing, show discrepancies and are not interchangeable.Citation23 At the same time, neglecting the effects of posterior corneal curvature may lead to inaccuracies in actual corneal power and significant postoperative overcorrection or undercorrection.Citation24,Citation25
Recently, IOLMaster 700 introduced a novel parameter, TK, which provides another method to assess the posterior corneal surface. Then, the built-in new Barrett TK Universal II formula of IOLMaster 700 was developed to be used with this new TK methodology, offering convenience in clinical practice. Some studies have reported that total corneal astigmatism based on TK is consistent with that based on TCRP;Citation26 however, TK and TCRP are not the same thing in theory. Assessment of the posterior corneal surface in TK is achieved by combining the data from the anterior corneal surface obtained by telecentric keratometry with the pachymetry data obtained by swept-source optical coherence tomography,Citation12 and there is no actual measured tomographic image of the posterior corneal surface in TK. This distinction could be an explanation to the present results. Although Bland‒Altman plots showed acceptable agreement of measurements between IOLMaster 700 and Pentacam HR, the differences in all parameters between the two devices were significant.
Since the manufacture of IOL steps in units of 0.5 D, we considered that an error of more than 0.5 D should be given clinical attention. It showed that the difference between TK and TCRP accounts for the difference in recommended IOL power between the novel Barrett TK Universal II and Barrett Universal II TCRP calculations, and a difference of 0.4 D between TK and TCRP would lead to a significant difference of 0.5 D in IOL power selection. Thus, a larger TSE from IOLMaster 700 need be noted, for it positively correlates with the difference between TK and TCRP, and we suggest performing a Scheimpflug measurement for prudential reasons.
The accuracy of the Barrett Universal II TCRP formula using Scheimpflug tomography-based TCRP has been widely reported in studies,Citation17–19 and since our results showed that more than 70% cases receive a difference of less than ±0.5 D in selected IOL power between the novel Barrett TK Universal II and Barrett Universal II TCRP calculations, it could be inferred that the predicted refraction outcome of the novel Barrett TK Universal II calculations would be likewise excellent. We can be sure that the novel Barrett TK Universal II and Barrett Universal II TCRP formulas are both accurate in PC-IOLs power calculation.
There were two main limitations of this study that should be interpreted. The first is the relatively small sample size limited a stratification analysis. Second, as an observational study, we could not directly indicate which the two Barrett methods result in less prediction errors, and this should be noted and compared in future randomized controlled trial studies.
In conclusion, the present study provides evidence of the agreement between the novel built-in Barrett TK Universal II formula and Barrett Universal II formula using TCRP, although the TK measurement of IOLMaster 700 and TCRP measurement of Pentacam HR are not interchangeable. The convenience of using the novel Barrett TK Universal II formula for IOL power calculation should be founded on measurement consistency between devices.
Disclosure
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The abstract of this paper was presented at the 35th APACRS Meeting (2023, Singapore) as a poster presentation with interim findings.
Additional information
Funding
References
- Wolffsohn JS, Davies LN. Presbyopia: effectiveness of correction strategies. Prog Retin Eye Res. 2019;68:124–143. doi:10.1016/j.preteyeres.2018.09.004
- Torky MA, Nokrashy AE, Metwally H, Abdelhameed AG. Visual performance following implantation of presbyopia correcting intraocular lenses. Eye. 2022. doi:10.1038/s41433-022-02188-y
- Melles RB, Holladay JT, Chang WJ. Accuracy of intraocular lens calculation formulas. Ophthalmology. 2018;125(2):169–178. doi:10.1016/j.ophtha.2017.08.027
- Chang P, Qian S, Wang Y, et al. Accuracy of new-generation intraocular lens calculation formulas in eyes with variations in predicted refraction. Graefes Arch Clin Exp Ophthalmol. 2023;261(1):127–135. doi:10.1007/s00417-022-05748-w
- Li H, Ye Z, Luo Y, Li Z. Comparing the accuracy of the new-generation intraocular lens power calculation formulae in axial myopic eyes: a meta-analysis. Int Ophthalmol. 2023;43(2):619–633. doi:10.1007/s10792-022-02466-4
- Voytsekhivskyy OV, Hoffer KJ, Savini G, Tutchenko LP, Hipolito-Fernandes D. Clinical accuracy of 18 IOL power formulas in 241 short eyes. Curr Eye Res. 2021;46(12):1832–1843. doi:10.1080/02713683.2021.1933056
- Voytsekhivskyy OV, Tutchenko L, Hipolito-Fernandes D. Comparison of the Barrett Universal II, Kane and VRF-G formulas with existing intraocular lens calculation formulas in eyes with short axial lengths. Eye. 2023;37(1):120–126. doi:10.1038/s41433-021-01890-7
- Rocha-de-Lossada C, Colmenero-Reina E, Flikier D, et al. Intraocular lens power calculation formula accuracy: comparison of 12 formulas for a trifocal hydrophilic intraocular lens. Eur J Ophthalmol. 2021;31(6):2981–2988. doi:10.1177/1120672120980690
- Shajari M, Kolb CM, Petermann K, et al. Comparison of 9 modern intraocular lens power calculation formulas for a quadrifocal intraocular lens. J Cataract Refract Surg. 2018;44(8):942–948. doi:10.1016/j.jcrs.2018.05.021
- Vega Y, Gershoni A, Achiron A, et al. High agreement between Barrett Universal II calculations with and without utilization of optional biometry parameters. J Clin Med. 2021;10(3):542. doi:10.3390/jcm10030542
- Shin MC, Chung SY, Hwang HS, Han KE. Comparison of two optical biometers. Optom Vis Sci. 2016;93(3):259–265. doi:10.1097/OPX.0000000000000799
- Savini G, Taroni L, Schiano-Lomoriello D, Hoffer KJ. Repeatability of total Keratometry and standard Keratometry by the IOLMaster 700 and comparison to total corneal astigmatism by Scheimpflug imaging. Eye. 2021;35(1):307–315. doi:10.1038/s41433-020-01245-8
- Fabian E, Wehner W. Prediction accuracy of total keratometry compared to standard keratometry using different intraocular lens power formulas. J Refract Surg. 2019;35(6):362–368. doi:10.3928/1081597X-20190422-02
- Srivannaboon S, Chirapapaisan C. Comparison of refractive outcomes using conventional keratometry or total keratometry for IOL power calculation in cataract surgery. Graefes Arch Clin Exp Ophthalmol. 2019;257(12):2677–2682. doi:10.1007/s00417-019-04443-7
- Qin Y, Liu L, Mao Y, et al. Accuracy of intraocular lens power calculation based on total keratometry in patients with flat and steep corneas. Am J Ophthalmol. 2022;247:103–110. doi:10.1016/j.ajo.2022.11.011
- Zhao H, Chen X, Liu B, Liu X, Liu Y. Accuracy of refractive outcomes using standard or total keratometry for intraocular lens power formulas in conventional cataract surgery. BMC Ophthalmol. 2023;23(1):346. doi:10.1186/s12886-023-03094-x
- Taroni L, Hoffer KJ, Barboni P, Schiano-Lomoriello D, Savini G. Outcomes of IOL power calculation using measurements by a rotating Scheimpflug camera combined with partial coherence interferometry. J Cataract Refract Surg. 2020;46(12):1618–1623. doi:10.1097/j.jcrs.0000000000000361
- Wang KM, Jun AS, Ladas JG, et al. Accuracy of Intraocular Lens Formulas in Eyes With Keratoconus. Am J Ophthalmol. 2020;212:26–33. doi:10.1016/j.ajo.2019.11.019
- Danjo Y. Modification of the Barrett Universal II formula by the combination of the actual total corneal power and virtual axial length. Graefes Arch Clin Exp Ophthalmol. 2023;261(7):1913–1921. doi:10.1007/s00417-023-05988-4
- Kohnen T, Lwowski C, Hinzelmann L, et al. Presbyopia correction in astigmatic eyes using a toric trifocal intraocular lens with quadrifocal technology. J Refract Surg. 2020;36(10):638–644. doi:10.3928/1081597X-20200729-04
- Lwowski C, Pawlowicz K, Petermann K, et al. Visual and patient-reported factors leading to satisfaction after implantation of diffractive extended depth-of-focus and trifocal intraocular lenses. J Cataract Refract Surg. 2022;48(4):421–428. doi:10.1097/j.jcrs.0000000000000780
- Savini G, Hoffer KJ, Lomoriello DS, Ducoli P. Simulated keratometry versus total corneal power by ray tracing: a comparison in prediction accuracy of intraocular lens power. Cornea. 2017;36(11):1368–1372. doi:10.1097/ICO.0000000000001343
- Ozyol P, Ozyol E. Agreement between swept-source optical biometry and scheimpflug-based topography measurements of anterior segment parameters. Am J Ophthalmol. 2016;169:73–78. doi:10.1016/j.ajo.2016.06.020
- Tonn B, Klaproth OK, Kohnen T. Anterior surface-based keratometry compared with Scheimpflug tomography-based total corneal astigmatism. Invest Ophthalmol Vis Sci. 2014;56(1):291–298. doi:10.1167/iovs.14-15659
- Savini G, Naeser K. An analysis of the factors influencing the residual refractive astigmatism after cataract surgery with toric intraocular lenses. Invest Ophthalmol Vis Sci. 2015;56(2):827–835. doi:10.1167/iovs.14-15903
- Li X, Cao X, Bao Y. Comparison of total corneal astigmatism between IOLMaster and pentacam. Biomed Res Int. 2022;2022:9236006. doi:10.1155/2022/9236006