Abstract
Purpose
To report the outcomes of different therapies in patients with conjunctival mucosa-associated lymphoid tissue (MALT) lymphoma.
Patients and Methods
This retrospective study included patients diagnosed with conjunctival MALT lymphoma between August 2000 and April 2022. Patients were classified into three groups according to their treatment: an observation group, a radiation therapy (RT) group, and a rituximab group (rituximab with or without chemotherapy). We analyzed overall survival (OS), overall, local, and systemic relapse-free survival (RFS), and adverse events after treatment.
Results
This study included 15 patients (22 eyes). The 10-year OS was 100%. The 2-, 5-, and 10-year overall RFS rates were 80.1%, 41.2%, and 41.2% in all patients, respectively. The 2- and 5-year local RFS rates in the observation group were 100% and 0%, respectively. The 2-, 5-, and 10-year local RFS rates were 87%, 87%, and 87% in the RT group and 83%, 67%, and 67% in the rituximab group, respectively. The 2- and 5-year systemic RFS rates in the observation group were both 100%, and the 2-, 5-, and 10-year systemic RFS rates were 92%, 55%, and 55% in the RT group, and 100%, 60%, and 60% in the rituximab group, respectively. After RT, 53.3% of the eyes developed cataracts and 75% of these were treated with cataract surgery. In addition, 53.3% of the eyes developed dry eyes and were treated with eye drops. Rituximab with or without chemotherapy resulted in some systemic adverse events, but these improved following symptomatic therapies.
Conclusion
RT resulted in good local control of conjunctival MALT lymphoma; however, systemic relapse may occur during long-term follow-up. Local and/or systemic relapse may also occur during long-term follow-up in patients treated by observation or rituximab with or without chemotherapy. Patients with conjunctival MALT lymphoma should be followed-up carefully for as long as possible after treatment.
Introduction
Mucosa-associated lymphoid tissue (MALT) lymphoma occurs in the stomach, lungs, thyroid, salivary glands, mammary glands, and ocular adnexa.Citation1 Conjunctival lymphomas account for 25%–30% of the lymphomas of the ocular adnexa.Citation2,Citation3 Most conjunctival lymphomas are B-cell non-Hodgkin lymphomas (98%), and the most frequent subtype of conjunctival B-cell lymphomas is MALT lymphoma (81%).Citation4 MALT lymphoma is an indolent type of lymphoma, and patients with conjunctival MALT lymphoma usually have good overall survival (OS).Citation5,Citation6 Close observation, surgical resection, or radiation therapy (RT) are generally recommended for patients with Ann Arbor stage I lymphoma with a single lesion, while close observation, surgical resection, or rituximab monotherapy or rituximab with chemotherapy are recommended for non-stage I lymphoma with involvement of two or more sites.Citation1,Citation7 Several studies have explored the treatment outcomes of patients with MALT lymphoma of the ocular adnexa, including the conjunctiva. Treatment outcomes may differ between conjunctival MALT lymphoma and MALT lymphoma of ocular adnexa other than conjunctiva because of difference in the anatomical location and histological type is different among ocular adnexa. Furthermore, we consider that it is easier to detect relapse in conjunctival MALT lymphoma than in other ocular adnexal lymphomas. In conjunctival MALT lymphoma, relapse can be detected on slit-lamp examination due to its location, while imaging such as computer tomography or magnetic resonance imaging (MRI) is required to detect relapse in other ocular adnexal lymphomas. The timing of relapse detection may affect treatment outcome. We believe that there is a need for study on the treatment outcomes specific to conjunctival MALT lymphoma because there have been only a few such reports,Citation5,Citation6 but these reported overall outcomes of various treatments, rather than the specific outcomes of each treatment. There is thus a need to gather data on the outcomes of different treatments in patients with conjunctival MALT lymphoma. This study aimed to analyze the outcomes of specific treatments and the adverse events in patients with conjunctival MALT lymphoma.
Methods
Patients
This retrospective study included 15 Patients (22 eyes) diagnosed with conjunctival MALT lymphoma at Kurume University Hospital between August 2000 and April 2022. Only patients who were followed for at least 1 year after the diagnosis of conjunctival MALT lymphoma were included in this study. Patients with other ocular tumors were excluded from this study. This study was approved by the Ethics Committee of Kurume University (No. 22154) and conformed to the tenets of the Declaration of Helsinki. The need for individual patient consent was waived due to the retrospective nature of the study. All patient data were anonymized to ensure patient confidentiality.
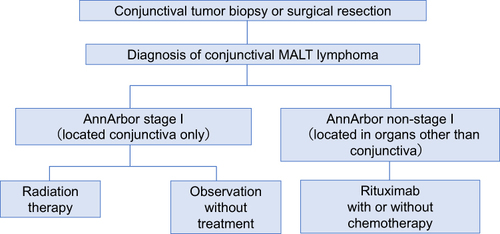
Diagnosis and Treatment
Conjunctival MALT lymphoma was diagnosed and staged according to the Ann Arbor staging system using the following procedures. Patients with conjunctival salmon-pink lesions on slit-lamp examination, suspicious of conjunctival malignant lymphoma, underwent MRI to determine the extent of the tumor before biopsy or surgical resection. A diagnosis of conjunctival MALT lymphoma was made by pathological examination, including immunohistochemical staining after biopsy or surgical resection. After a diagnosis of conjunctival MALT lymphoma, patients were referred to the hematology department for staging and determination of treatment strategy. Positron emission tomography-computed tomography or whole-body computed tomography, bone marrow aspiration, and biopsy were performed to determine the clinical stage, according to the Ann Arbor staging system. Patients with stage I lymphoma localized to the conjunctiva received close observation or RT, and patients with non-stage I lymphoma involving the conjunctiva and other sites received rituximab with or without chemotherapy, according to the Japanese Society of Hematology guidelinesCitation1,Citation7 (). In the past, patients with MALT lymphoma were treated with rituximab with chemotherapy, but since 2010 those patients have been treated with rituximab monotherapy. Conjunctival MALT lymphomas in patients with a prior history of MALT lymphoma in sites other than the conjunctiva, and complete remission of the lymphoma on the first visit were treated as primary conjunctival MALT lymphomas in our study. Patients were classified into three groups according to their treatment: an observation group (observation only), RT group, and rituximab group (rituximab with or without chemotherapy).
Statistical Analysis
OS and relapse-free survival (RFS) were estimated using Kaplan–Meier curves. OS was defined as the time from initiation of treatment to death from any causes or the time of last visit. Relapse was classified as overall, local, or systemic, and RFS was defined as the time from initiation of treatment to relapse. RFS was evaluated in all patients and in each group and compared among groups using the Log rank test. All tests were two-tailed and p<0.05 was considered to indicate a significant difference. All statistical analyses were performed using JMP version 15 and SAS 9.4 (SAS Institute Inc., Cary, NC, USA).
Results
Patient Characteristics
The patient characteristics are shown in . The mean (± standard deviation) age at diagnosis was 54.7±16.7 years (range, 28–76 years) and the mean follow-up period after diagnosis was 77.0±47.5 months. Three patients (5 eyes) were men and 12 patients (17 eyes) were women. Thirteen patients (18 eyes) were diagnosed with MALT lymphoma for the first time, referred as primary conjunctival MALT lymphoma. Two patients (4 eyes) with a history of MALT lymphoma in other sites (small intestine and lung) with complete remission developed MALT lymphoma in the conjunctiva, and these patients were treated as having primary conjunctival MALT lymphoma. Eleven patients (16/22 eyes; 72.7%) were stage I. One patient (1 eye) was closely observed after complete tumor resection. Ten patients (15 eyes) were treated with RT, with a mean radiation dose of 30.7 Gy (range, 30–36 Gy). Four patients (6/22 eyes; 27.3%) were stage II because they had MALT lymphomas in other sites (stomach, cervical lymph nodes, mediastinal lymph nodes, and lung), and were treated with rituximab. Chemotherapy (cyclophosphamide, doxorubicin, vincristine, prednisolone [CHOP] + cyclophosphamide, vincristine, prednisolone [CVP]) was combined in one patient. Rituximab with chemotherapy was a standard treatment strategy when the patient was diagnosed.
Table 1 Characterisitics of Patients Diagnosed with Conjunctival MALT Lymphoma
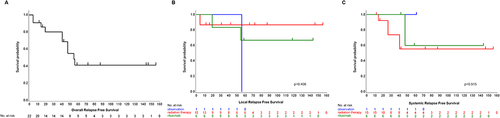
OS and Patterns of Relapse and RFS
All patients remained alive during the follow-up period, and the10-year OS was 100% (). The 2-, 5-, and 10-year overall RFS rates were 80.1%, 41.2%, and 41.2% in all patients, respectively (). The 2- and 5-year local RFS rates in the observation group were 100% and 0%, respectively, and the 2-, 5-, and 10-year local RFS rates were 87%, 87%, and 87% in the RT group, and 83%, 67%, and 67% in the rituximab group, respectively (). The 2- and 5-year systemic RFS rates in the observation group were both 100%, and the 2-, 5-, and 10-year systemic RFS rates were 92%, 55%, and 55% in the RT group, and 100%, 60%, and 60% in the rituximab group, respectively (). There was no significant difference in local or systemic RFS rates among the groups (Log rank test, p=0.40, p=0.51, respectively). One patient (1 eye) in the observation group, one patient (2 eyes) in the RT group, and two patients (2 eyes) in the rituximab group relapsed locally. The one patient (1 eye) in the observation group did not relapse systemically, and three patients (5 eyes) in the RT group and two patients (2 eyes) in the rituximab group relapsed systemically.
Figure 2 Kaplan–Meier curve of overall survival (OS) in patients with conjunctival MALT lymphoma. Ten-year OS was 100%.
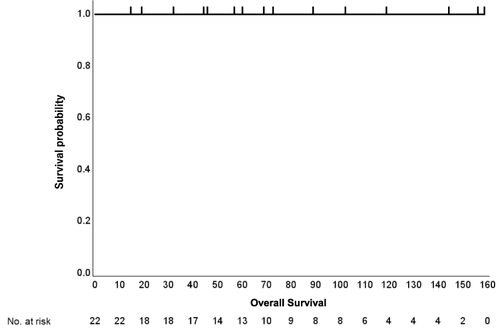
Figure 3 Kaplan–Meier curve of relapse-free survival (RFS) in patients with conjunctival MALT lymphoma. (A) Overall RFS. Two-, 5-, and 10-year overall RFS rates were 80.1%, 41.2%, and 41.2% in all patients, respectively. (B) Local RFS in radiation, rituximab, and observation groups. Two- and 5-year local RFS rates in the observation group were 100% and 0%, respectively. Two-, 5-, and 10-year local RFS rates were 87%, 87%, and 87% in the radiation group and 83%, 67%, and 67% in the rituximab group, respectively. (C) Systemic RFS in the radiation, rituximab, and observation groups. Two- and 5-year systemic RFS rates in the observation group were both 100%. Two-, 5-, and 10-year systemic RFS rates were 92%, 55%, and 55% in the radiation group, and 100%, 60%, and 60% in the rituximab group, respectively.
Relapsed Cases
The clinical characteristics of the patients with local and/or systemic relapse are shown in . Case 1 in the observation group relapsed at the same site as the primary tumor 56 months after complete surgical resection and then opted for observation, with no progression until the end of follow-up period. Case 2 in the RT group relapsed at the same site as the primary tumor 4 months after treatment initiation and was initially observed; however, treatment with rituximab and chemotherapy was subsequently started because of relapse in the cervical lymph nodes at 26 months after initiation of RT. Cases 6 and 7 in the RT group relapsed systemically at 14 and 41 months after treatment initiation, respectively. Both of these cases were treated with rituximab and chemotherapy after systemic relapse, with additional RT in Case 6 because of relapse in the pharynx. Cases 12 and 15 in the rituximab group relapsed locally at 55 and 19 months after treatment initiation, respectively, and were treated with RT for local relapse because they had no systemic relapse. Case 14 in the rituximab group relapsed in the lung at 47 months after treatment initiation, but opted for subsequent observation.
Table 2 Summary of Relapsed Patients
Adverse Events
Five of the 10 patients (8/15 eyes; 53.3%) in the RT group developed cataracts, and four patients (6/8 eyes; 75%) underwent cataract surgery. Six patients (8/15 eyes; 53.3%) developed dry eye, which was improved by eye drops in all patients. Of four patients (6 eyes) in the rituximab group, one patient (1 eye) treated with rituximab monotherapy developed fever and general malaise, and one patient (2 eyes) treated with rituximab with CHOP and CVP had numbness of the hands and fingers, abdominal pain, and pancytopenia. All cases improved with symptomatic therapies.
Case Report (Case 14)
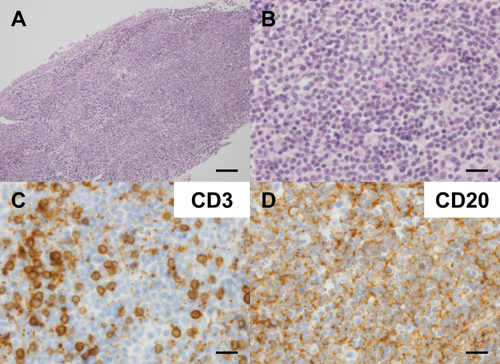
Case 14 was a 73-year-old woman who visited our hospital with conjunctival tumors in both eyes. Conjunctival malignant lymphoma was suspected because of the presence of salmon-pink lesions in both eyes on slit-lamp examination (). She underwent surgical resection of the lesions and conjunctival MALT lymphoma was confirmed by pathological examination of the resected specimen (). The lymphoma was classified as Ann Arbor Stage II, because she had completed RT for MALT lymphoma in the right lung a few months before visiting our hospital. She was treated with rituximab alone with no adverse events, and had complete remission, but subsequently relapsed in the left lung 47 months after treatment initiation. She then opted for observation without treatment.
Figure 4 Slit-lamp images of conjunctival MALT lymphoma in Case 14. Slit-lamp images of conjunctival MALT lymphoma (arrows) in the right (A) and left eyes (B) in Case 14. Conjunctival salmon-pink lesions were found at the lower palpebral conjunctival fornix in the right eye and in the superior and medial bulbar conjunctiva in the left eye.
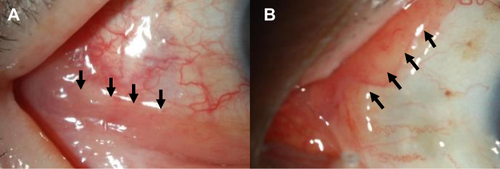
Figure 5 Histological images of conjunctival MALT lymphoma in the left eye in Case 14 (A and B) Hematoxylin and eosin staining. (A) Atypical lymphocytes were diffusely increased. Scale bar = 100 µm. (B) Chromatin was heavily stained and there was infiltration of small atypical lymphocytes with swollen nuclei. Scale bar = 20 µm. (C and D) Immunohistochemical staining for (C) CD3 and (D) CD20. Scale bar = 20 µm.
Discussion
There have been a few reports on overall treatment outcomes of conjunctival MALT lymphoma.Citation5,Citation6 Nam et al reported that patients with conjunctival MALT lymphoma without systemic involvement underwent RT (median radiation dose: 30.0 Gy, range: 20.0–45.0 Gy), and patients with systemic involvement received rituximab + CVP or CHOP. The 5- and 10-year overall RFS rates were 89.6% and 72.9%, respectively.Citation5 In the study by Saul et al, patients with conjunctival MALT lymphoma were treated with observation, RT, RT + immunochemotherapy (median radiation dose, 33 Gy; range, 25.5–45 Gy), immunochemotherapy alone after biopsy or surgical resection, with 5- and 10-year overall progression-free survival (PFS) rates were 81.8% and 68.4%.Citation6 In our study, the 2-, 5-, and 10-year overall RFS rates were 80.1%, 41.2%, and 41.2% in all patients, respectively. In our study, the treatment results were good at 2 years, but those at 5 and 10 years were poorer compared with previous reports. It might be because of the difference in the percentage of non-I stage patients (1.23% in study by Nam et al;Citation5 13.5% in Saul et al;Citation6 26.7% in our study).
To the best of our knowledge, there have been no previous reports on the outcomes of specific treatments for MALT lymphoma limited to the conjunctiva. In contrast, several studies have reported the outcomes of treatments in patients with ocular adnexal MALT lymphoma (OAML), including conjunctival MALT lymphoma. Fung et al reported 5- and 10-year local control rates of 96% and 86%, respectively, and systemic RFS rates of 75% and 45%, respectively, in 39 patients with stage I OAML treated with RT.Citation8 In addition, Shirota et al reported a 5-year local PFS rate of 100% and 5-year disease PFS of 93.3% in patients with OAML treated with RT (mean radiation dose, 30 Gy).Citation9 The 2-, 5-, and 10-year local RFS rates in the RT group in the current study were 87%, 87%, and 87%, respectively, and the 2-, 5-, and 10-year systemic RFS rates were 92%, 55% and 55%, respectively. Local RFS in our study was good, consistent with previous reports.Citation8,Citation9 Systemic control at 2 years was good in the current study, but decreased 5 years after RT, while previous studies showed that systemic control decreased 10 years after RT.Citation8 This apparent difference in time to systemic relapse may be related to the differences in clinical characteristics between conjunctival MALT lymphoma and OAML. Nevertheless, the results suggest that long-term follow-up after RT is necessary to detect systemic relapse.
Mino et al reported a 2-year event-free survival rate, defined as survival without evidence of disease progression or relapse, of 100% in patients with OAML treated with rituximab.Citation10 Song et al reported the treatment outcomes of 21 patients with OAML treated with CVP, and found 2- and 5-year PFS rates, defined as survival without evidence of local or systemic relapse or disease progression, of 90% and 66%, respectively, with most relapses occurring locally (5/7 relapse patients).Citation11 In the present study, the 2-, 5-, and 10-year local RFS rates in the rituximab group were 83%, 67%, and 67%, respectively, and the systemic RFS rates were 100%, 60%, and 60%, respectively. The 2-year local and systemic RFS rates in this group were similar to those in previous reports.Citation10,Citation11 Local or systemic relapse occurred 5 or more years after treatment initiation in our study. In previous studies, patients with OAML of all stages, including stage I, were treated with rituximab or chemotherapy,Citation10,Citation11 while stage I patients in our study were not treated with rituximab or chemotherapy. Jeon et al reported that patients with advanced stage were more likely to relapse.Citation12 Long-term follow-up of at least 5 years would be necessary to detect local and/or systemic relapse in patients with non-stage I MALT lymphoma of the conjunctiva after rituximab with or without chemotherapy.
Tanimoto et al reported a 10-year PFS rate of 46.1% in patients with OAML observed without treatment.Citation13 The treatment outcome following observation in our study could not be compared with previous studies, because the group only included one patient (Case 1, 1 eye). Case 1, who was observed after complete surgical resection, relapsed at the same site as the primary lesion 56 months after treatment initiation. Conjunctival MALT lymphoma is not life-threatening and has an indolent clinical course, and observation is thus a valid treatment option after biopsy or surgical resection, according to patient preference. Notably however, observation without treatment may possibly be associated with a higher relapse rate compared with RT or rituximab with or without chemotherapy.
Conjunctival MALT lymphoma generally has a good prognosis. Nam et al reported that the 5- and 10-year OS rates of conjunctival MALT lymphoma were both 98.2% and the disease-specific survival rates were both 98.2%.Citation5 Saul et al reported that the 5- and 10-year OS rates of conjunctival MALT lymphoma were 91.9% and 89.4%, respectively.Citation6 Similarly, the 10-year OS rate in the current study was excellent (100%), in accord with previous reports.
To the best of our knowledge, there have been no previous reports of the adverse effects of RT for conjunctival MALT lymphoma; however, RT-related adverse events have been reported in patients with OAML, including conjunctival MALT lymphoma. The incidence of cataract after RT for OAML was previously estimated to be 22%–52.4%,Citation12,Citation14–17 compared with 53.3% of eyes with conjunctival MALT lymphoma treated with RT in the current study. Previous studies also reported that radiation dose, lens shielding, age, and patient sex were associated with cataract formation after RT.Citation14,Citation15,Citation17,Citation18 Notably, although cataract surgery improves visual acuity, it causes early loss of accommodation, and may thus be an important issue for young patients.
Dry eye after RT is considered to be caused by damage to the meibomian glands, resulting in reduction or absence of the lipid layer of the tear film and evaporation, or damage to the acinar cells of the lacrimal glands.Citation19 Previous studies reported that 31.5%–59% of patients with OAML developed dry eye (radiation dose range, 22–45 Gy),Citation12,Citation14,Citation16 compared with 53.3% of patients treated with RT (mean radiation dose, 30.7 Gy; range, 30–36 Gy) in the present study.
Rituximab is known to have systemic adverse effects, including pancytopenia, infection, cardiac disease, and decreased blood pressure. However, Annibali et al reported that, among seven eyes in six patients with OAML, one patient had varicella zoster virus reactivation (Ramsay Hunt syndrome) and herpetic keratitis,Citation20 while Tuncer et al reported no systemic or ocular adverse events.Citation21 Regarding chemotherapy, Song et al reported systemic adverse events such as neutropenia, anemia, elevated alanine aminotransferase, and paresthesia in patients with ocular adnexal MALT lymphoma treated with CVP.Citation11 In our study, fever and general malaise were noted as systemic adverse events after rituximab monotherapy (Case 15), while Case 12, who was treated with rituximab and CHOP+CVP, had numbness of the hands and fingers, abdominal pain, and pancytopenia. All adverse events in the current study were systemic, and no ocular adverse events occurred.
This study was limited by the small number of patients. Further studies with larger numbers of patients are therefore needed to verify the results.
Conclusion
The results of this study indicated that RT generally results in good local control of conjunctival MALT lymphoma, but systemic relapse may still occur during long-term follow-up. Local and/or systemic relapse may occur during long-term follow-up after observation or treatment with rituximab with or without chemotherapy. It is therefore necessary to follow up patients with conjunctival MALT lymphoma carefully for as long as possible after treatment.
Disclosure
The authors report no conflicts of interest in this work.
Acknowledgments
The authors thank Kazuko Arima for English editing. We also thank Susan Furness, PhD, from Edanz (https://jp.edanz.com/ac) for editing a draft of this manuscript.
Additional information
Funding
References
- Kobayashi Y. JSH practical guidelines for hematological malignancies, 2018. II. Lymphoma-2. Marginal zone lymphoma (MALT lymphoma/extranodal marginal zone lymphoma of mucosa-associated lymphoid tissue and splenic marginal zone lymphoma). Int J Hematol. 2019;110(4):393–405.
- Sjö LD. Ophthalmic Lymphoma: epidemiology and Pathogenesis. Acta Ophthalmol. 2009;87:1–20. doi:10.1111/j.1755-3768.2008.01478.x
- Kirkegaard MM, Rasmussen PK, Coupland SE, et al. Conjunctival Lymphoma—An International Multicenter Retrospective Study. JAMA Ophthalmology. 2016;134(4):406–414. doi:10.1001/jamaophthalmol.2015.6122
- Kirkegaard MM, Coupland SE, Prause JU, Heegaard S. Malignant lymphoma of the conjunctiva. Surv Ophthalmol. 2015;60(5):444–458. doi:10.1016/j.survophthal.2015.05.001
- Nam SW, Woo KI, Kim YD. Characteristics of primary extranodal marginal zone B-cell lymphoma in Korea: conjunctiva versus other ocular adnexa. Br J Ophthalmol. 2018;102(4):502–508. doi:10.1136/bjophthalmol-2017-310741
- Saul EE, Alderuccio JP, Reis IM, et al. Long-term outcomes of patients with conjunctival extranodal marginal zone lymphoma. Am J Haematol. 2023;98(1):148–158. doi:10.1002/ajh.26591
- Izutsu K. JSH practical guidelines for hematological malignancies, 2018: II. Lymphoma-1. Follicular lymphoma (FL). Int J Hematol. 2019;110(1):11–19. doi:10.1007/s12185-019-02655-5
- Fung CY, Tarbell NJ, Lucarlli MJ, et al. Ocular Adnexal lymphoma: clinical behavior of distinct world health organization classification subtypes. Int J Radiat Oncol Biol Phys. 2003;57(5):1382–1391. doi:10.1016/S0360-3016(03)00767-3
- Shirota N, Nakayama H, Shiraishi S, et al. Target volume dose and clinical outcome in radiotherapy for primary marginal zone lymphoma of the ocular adnexa. Mol Clin Oncol. 2017;6(6):833–838. doi:10.3892/mco.2017.1241
- Mino T, Mihara K, Yoshida T, Takihara Y, Ichinohe T. Monthly administration of rituximab is useful for patients with ocular adnexal mucosa-associated lymphoid tissue lymphoma. Blood Cancer J. 2014;4(9):e245–e245.
- Song EK, Kim SY, Kim TM, et al. Efficacy of chemotherapy as a first-line treatment in ocular adnexal extranodal marginal zone B-cell lymphoma. Ann Oncol. 2008;19(2):242–246. doi:10.1093/annonc/mdm457
- Jeon YW, Yang HJ, Choi BO, et al. Complication of selection and long-term clinical outcomes betweeen chemotherapy and radiotherapy as primary therapeutic modality for ocular adnexal MALT lymphoma. EClin Med. 2018;4-5:32–42. doi:10.1016/j.eclinm.2018.10.001
- Tanimoto K, Kaneko A, Suzuki S, et al. Primary ocular adnexal MALT lymphoma: a long-term follow-up study of 114 patients. Jpn J Clin Oncol. 2007;37(5):337–344. doi:10.1093/jjco/hym031
- Goda JS, Le LW, Lapperriere NJ, et al. Localized orbital mucosa-associated lymphoma tissue lymphoma managed with primary radiation therapy: efficacy and toxicity. Int J Radiat Oncol Biol Phys. 2011;81(4):e659–666. doi:10.1016/j.ijrobp.2011.03.050
- Harada K, Murakami N, Kitaguchi M, et al. Localized ocular adnexal mucosa-associated lymphoid tissue lymphoma treated with radiation therapy. A long-term outcome in 86 patients with 104 treated eyes. Int J Radiat Oncol Biol Phys. 2014;88(3):650–654. doi:10.1016/j.ijrobp.2013.11.235
- Park HH, Lee WL, Sung SY, Choi BO. Treatment outcome and risk analysis for cataract after radiotherapy of localized ocular adnexal mucosa-associated lymphoid tissue (MALT) lymphoma. Radiat Oncol J. 2017;35(3):249–256. doi:10.3857/roj.2017.00374
- Fukutsu K, Kase S, Ishijima K, et al. The clinical features of radiation cataract in patients with ocular adnexal mucosa-associated lymphoid tissue lymphoma. Radiat Oncol. 2018;13(1):95. doi:10.1186/s13014-018-1045-7
- Lee J, Yoon JS, Kim JS, et al. Long-term outcome, relapse patterns, and toxicity after radiotherapy for orbital mucosa-associated lymphoid tissue lymphoma: implications for radiotherapy optimization. Jpn J Clin Oncol. 2019;49(7):664–670. doi:10.1093/jjco/hyz044
- Nuzzi R, Trossarello M, Bartoncini S, et al. Ocular complications after radiation therapy: an observational study. Clin Ophthalmol. 2020;14:3153–3166. doi:10.2147/OPTH.S263291
- Annibali O, Chiodi F, Sarlo C, et al. Rituximab as single agent in primary MALT lymphoma of the ocular adnexa. Biomed Res Int. 2015;2015:895105. doi:10.1155/2015/895105
- Tuncer S, Tanyildiz B, Basaran M, et al. Systemic rituximab immunotherapy in the management of primary ocular adnexal lymphoma: Single institution experience. Curr Eye Res. 2015;40(8):780–785. doi:10.3109/02713683.2014.959605