Abstract
Purpose
We describe an alternative automated technique that consists of simultaneous anterior capsule puncture and decompression of the capsular bag by using an insulin needle attached to the aspiration tubing of the phacoemulsification device to prevent the occurrence of the “Argentinian Flag sign” during capsulorhexis in intumescent cataract.
Setting
Instituto de Olhos de Assis and Center of Specialties Hoftalmed, located in the state of São Paulo, Brazil.
Design
Prospective interventional study.
Methods
Eighty-eight eyes of 88 patients with white or intumescent cataracts were included in this study. Routine clear cornea incision, capsule staining with trypan blue, intracameral anesthesia, and ophthalmic viscoelastic device were used before the procedure. A 26-gauge needle was connected to the phacoemulsification aspiration tubing using a double male Luer connector for irrigation, and aspiration was inserted into the anterior chamber through a new paracentesis incision with the bevel facing down. Immediately after insertion, automated aspiration of the liquefied cortex was performed to remove anterior intralenticular material and achieve capsular decompression. Compression of the nucleus with the needle tip was performed to remove any liquefied material trapped between the posterior surface of the nucleus and the posterior capsule. All surgeries were performed using the same phacoemulsification and parameters. The rate of complete continuous capsulorhexis was observed and noted.
Results
No complications were observed in any of the cases. A single-stage, continuous, and well-centered capsulorhexis was achieved in 100% of cases.
Conclusion
We conclude that a simultaneous puncture and decompression of the capsular bag using an insulin needle attached to the aspiration tubing of the phacoemulsification machine effectively avoided the “Argentinian Flag sign” in intumescent cataract surgery.
Introduction
White cataract is a term used to describe a certain type of mature cortical cataract, which may present zonular weakness and a fragile capsule with alterations in its metabolism. We believe that intumescent white cataracts can suffer from fluid influx and high intralenticular pressure (ILP) due to the dysfunction of lens epithelial cells.
Continuous curvilinear capsulorhexis (CCC) becomes a challenging step with a high risk of rupture or radial tear in a capsule. Its radial tear stained with trypan blue simulates the Argentinian national flag. The incidence of an incomplete capsulorhexis in these cases ranged from 3.85%, according to Jacob et alCitation1 to 28.3%, according to Chakraborty et al.Citation2
Several techniques have been described to achieve a successful capsulorhexis in intumescent white cataracts.
In a study by Figueiredo et al,Citation3 the “Brazilian technique” described using a bimanual irrigation/aspiration cannula to maintain the anterior chamber stable while decompression of the liquefied material from the posterior intralenticular space reduces the pressure of the capsular bag. The capsulorhexis is then completed in two stages.
Kara-Jose et al have mentioned a technique in which a small capsulorhexis is made and then subsequently enlarged after capsular aspiration and decompression.Citation4
Performing femtosecond laserCitation5 or Nd:Yag laser before surgery can also be an effective option to avoid the occurrence of Argentinian Flag sign in intumescent cataracts.Citation6
Fluid drainage using a 30-gauge needle through a limbal stab incision seems to be the most used technique in these cases.Citation7
Phacocapsulotomy involves puncturing the anterior capsule with the tip of the phacoemulsification probe and removing the material from the lens.Citation8
Detection of subcapsular fluid using anterior segment ocular coherence tomography (AS-OCT) allows for better planning and management.Citation9
All technique mentioned above can have their advantages that will be mentioned further.
The purpose of this study is to describe an alternative automated technique that consists of simultaneous anterior capsule puncture and decompression of the capsular bag using an insulin needle attached to the aspiration tubing of the phacoemulsification device to prevent the occurrence of the “Argentinian Flag sign” during capsulorhexis in intumescent cataracts.
Materials and Methods
For this analysis, a prospective interventional study was performed. The Institutional Review Board of Instituto Suel Abujamra approved this study under the following file: CAAE 71051423.2.0000.5477. Informed consent was obtained from all the patients before the surgery. All the procedures followed the ethical standards the responsible human experimentation committee set forth and the principles outlined in the revised Helsinki Declaration of 1983.
Eighty-eight eyes of 88 patients with white or intumescent cataracts were included in this study. Twenty-seven eyes were operated in the Instituto de Olhos de Assis (IOA) in the city of Assis (Sao Paulo State) by one experienced surgeon. Sixty-one eyes were operated on in the Center of Specialties Hoftalmed, located in the city of São José dos Campos (Sao Paulo State), by another experienced surgeon.
This study included patients with white or intumescent cataracts according to the LOCS III classification. Patients with previous ocular trauma, retinal detachment or vitreous hemorrhage, anterior or posterior synechiae, pseudoexfoliation, zonular abnormality, dislocated lens, glaucoma, corneal abnormality, and a history of uveitis were excluded from the study.
Complete ophthalmological evaluation, including full medical history, best-corrected visual acuity, anterior slit-lamp examination, intraocular pressure, ocular ultrasound (Compact Touch, Quantel medical, Rockwall, USA), corneal specular microscopy (Topcon SP-2000P, Topcon, Tokyo, Japan), corneal tomography (Pentacam HR, Oculus, Wetzlar, Germany), posterior segment tomography (Ivue-SD- Optovue, Fremont, USA), and immersion biometry for intraocular lens calculation (Ocuscan (Alcon, Fort Worth, USA), was performed.
All surgeries were performed using the same phacoemulsification (Constellation Vision System, Alcon Laboratories, Fort Worth, USA) using the following parameters and devices: Ozil hand piece, 45-degree, 0.9-mm ABS Kelman mini-flared tip or Balanced tip.
All surgeries were performed under topical anesthesia. A clear corneal incision was performed using 2.2 mm keratome (Alcon Laboratories, Fort Worth, Texas). The anterior lens capsule was stained with 0.03% trypan blue dye (Ophthalmos, São Paulo, Brazil), intracameral anesthetic solution (2% isobaric lidocaine without preservatives), and a 2% sodium hyaluronate (20 mg/mL) ophthalmic viscoelastic device (OVD) (Ophthalmos, São Paulo, Brazil) was injected into the anterior chamber. Two 1.0mm paracentesis were made in the usual manner.
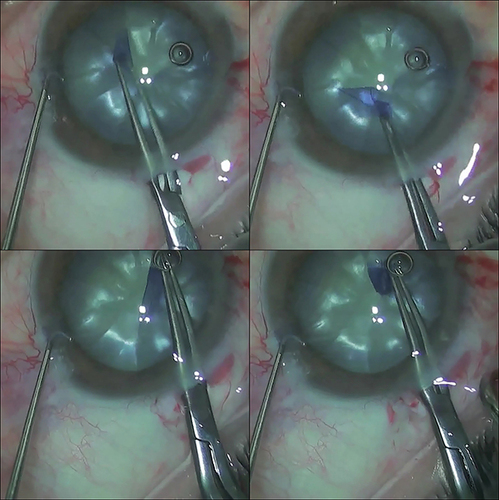
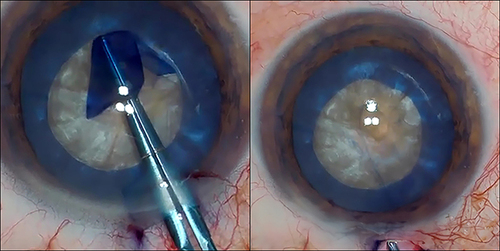
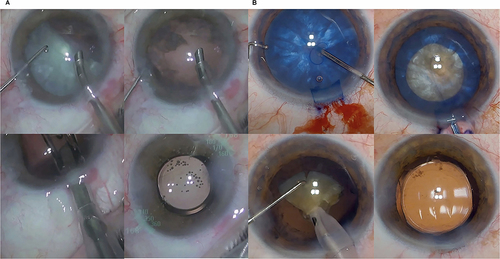
A 26-gauge needle connected to the phacoemulsification aspiration tubing using double male Luer connectors for irrigation and aspiration (Alcon Laboratories, Fort Worth, Texas) was inserted into the anterior chamber through a new paracentesis incision with the bevel facing down (). Immediately after insertion, automated aspiration of the liquefied cortex was performed to remove anterior intralenticular material and achieve capsular decompression (). Compression of the nucleus with the needle tip was performed to remove any liquefied material trapped between the posterior surface of the nucleus and the posterior capsule (Video 1).
Figure 1 Illustration of instrument assembly before starting the surgery. (A) A 13 mm long 26G needle, with the bevel facing down. (B) The needle being connected to the double male Luer adapter. (C) Phacoemulsifier aspiration pathway. (D) Aspiration line being connected to the double male Luer adapter. (E) Completed instrument assembly.
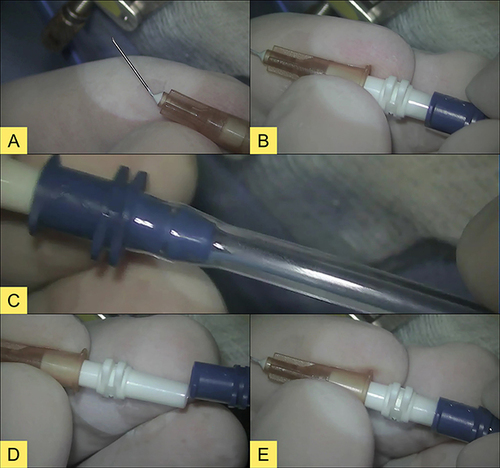
Figure 2 (A) Illustration of the automated instrument being inserted into the anterior chamber through a new paracentesis with the bevel facing down moments before the central perforation of the anterior lens capsule is performed. (B) Illustration of the liquefied cortex moments after capsular puncture. (C) Illustration of the anterior capsule after automated aspiration of the liquefied material.
Some caution must be taken regarding the details of the technique. The surgeon must not perform the aspiration with the bevel facing upward, and the needle should not be inserted into the anterior chamber through the main incision.
All I/A parameters of the device were as follows: Irrigation 110cm; Linear vacuum 0–650mmHg, Aspiration/Flow rate 0–40cc/min).
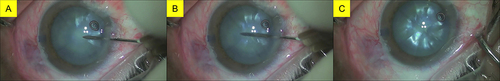
Capsular decompression was followed by OVD injection to compensate for intracapsular volume loss and to flatten the anterior capsule (). OVD was injected in a centrifugal and circumferential manner from the periphery so that the fluid trapped at the periphery under the capsule exits through the center. A regular-size capsulorhexis was then completed in a single stage using a micro capsulorhexis forceps (Haldipurkarÿ Masket Capsulorhexis, PlusSurgicals, Kolkata) under the guidance of the Verion-assisted capsulorhexis system (Alcon Laboratories, Fort Worth, Texas), with the outer circle was defined at 5.3 mm and the inner circle at 5.0 mm to achieve a capsulorhexis size of approximately 5 mm in the IOL plane ( and ). Routine phacoemulsification was then performed in the usual manner ().
Figure 5 (A and B) Phacoemulsification performed in the usual manner, after using the automated technique and with the intraocular lens inside the capsular bag.
The rate of complete continuous capsulorhexis was observed and noted.
Results
No complication was observed in any of the cases performed by both surgeons. A single-stage, continuous, and well-centered capsulorhexis was achieved in 100% of cases.
Discussion
From all techniques described, there is probably one that the surgeon can adopt to avoid Argentinian Flag sign in cases of high intralenticular pressure. Each technique has advantages and disadvantages. Unfortunately, there is no quantitative statistical analysis comparing these various techniques.
The “Brazilian technique” described by Figueiredo et alCitation3 using a bimanual irrigation/aspiration (I/A) cannula to maintain a stable anterior chamber followed by decompression of the liquefied material from the posterior intralenticular space can protect from Argentinian Flag sign. However, the border of the capsulorhexis can run toward the periphery before using bimanual I/A or before AC stability. The same observation applies to the technique described by Kara-Jose et al in which a small capsulorhexis is initially made and then enlarged after aspiration is performed and decompression achieved.Citation4
We believe that the moment of greatest risk of capsulorhexis run out (and the occurrence of the Argentinian Flag sign) is when the capsulorhexis tear approaches the opposite side of its beginning. If the surgeon traverses this point faster, capsulorhexis run out might be avoided. Analysis of the anterior chamber depth and degree of swelling of the lens is important data to be studied before surgery for better planning. Further studies are being performed to clarify if these data can have any influence on the capsular integrity in intumescent cataracts.
Performing femtosecond laserCitation5 or Nd:Yag laser before surgery is a two-step procedure, and we suggest monitoring the interval between the two procedures since capsular tear can run out during head movement even with a closed anterior chamber.
Fluid drainage using a 30-gauge needle through a limbal stab incision seems to be the most used technique in these cases.Citation7 However, capsulorhexis can get out of control during aspiration if the cortex pushes the anterior capsule anteriorly. Continuous and constant aspiration is suggested for less turbulence and capsular integrity.
Some key points of this technique must be remembered at all times. The surgeon must not perform the aspiration with the bevel facing upward, and the needle should not be inserted into the anterior chamber through the main incision due to the risk of sudden anterior chamber decompression and instability.
Automated capsular decompression has shown better aspiration personalized control using the foot pedal. It also enables the surgeon to better control the amplitude and duration of the needle’s aspiration within the capsule. The surgeon feels free to concentrate on the movement of the needle’s tip during the decompression process.
This study included two experienced surgeons to help reduce the potential for individual bias in surgical outcomes and support the technique’s reproducibility.
Conclusion
We conclude that a simultaneous puncture and decompression of the capsular bag using an insulin needle attached to the aspiration tubing of the phacoemulsification machine effectively avoided the “Argentinian Flag sign” in intumescent cataract surgery.
What was Know
Continuous curvilinear capsulorhexis becomes a challenging step in intumescent cataracts, with a high risk of rupture or radial tear of the capsule.
Fluid drainage using a 30-gauge needle through a limbal stab incision seems to be the most used technique in these cases.
What this Paper Adds
Simultaneous puncture and decompression of the capsular bag using an insulin needle attached to the aspiration tubing of the phacoemulsification machine effectively avoided the “Argentinian Flag sign” in intumescent cataract surgery.
Disclosure
The authors report no conflicts of interest in this work.
Acknowledgment
Dr. Antunes and Dr. Rosatelli Neto contributed equally to this work and share joint first authorship.
References
- Jacob S, Agarwal A, Agarwal A, et al. Trypan blue as an adjunct for safe phacoemulsification in eyes with white cataract. J Cataract Refract Surg. 2002;28:1819–1825. doi:10.1016/S0886-3350(01)01316-5
- Chakrabarti A, Singh S, Krishnadas R. Phacoemulsification in eyes with white cataract. J Cataract Refract Surg. 2000;26:1041–1047. doi:10.1016/S0886-3350(00)00525-3
- Figueiredo CG, Figueiredo J, Figueiredo GB. Brazilian technique for prevention of the Argentinean flag sign in white cataract. J Cataract Refract Surg. 2012;38:1531–1536. doi:10.1016/j.jcrs.2012.07.002
- Kara-Junior N, de Santhiago MR, Kawakami A, et al. Mini-rhexis for white intumescent cataracts. Clinics (Sao Paulo). 2009;64:309–312. doi:10.1590/S1807-59322009000400007
- Titiyal JS, Kaur M, Singh A, et al. Comparative evaluation of femtosecond laser-assisted cataract surgery and conventional phacoemulsification in white cataract. Clin Ophthalmol. 2016;10:1357–1364. doi:10.2147/OPTH.S108243
- Coelho RP, Neumann RZ, Vieira Messias AM. Comparison between FLACS and Nd: YAG laser in preventing the Argentinian flag sign in intumescent white cataracts. J Cataract Refract Surg. 2023;49:213–214. doi:10.1097/j.jcrs.0000000000001114
- Balyan M, Jain AK, Malhotra C, et al. Achieving successful capsulorhexis in intumescent white mature cataracts to prevent Argentinian flag sign - A new multifaceted approach to meet the challenge. Indian J Ophthalmol. 2021;69:1398–1403. doi:10.4103/ijo.IJO_1903_20
- Teng CC. Phaco capsulotomy: a technique to prevent the Argentinean Flag Sign. Clin Ophthalmol. 2017;11:1937–1940. doi:10.2147/OPTH.S138676
- Dhami A, Dhami AS, Singh H, et al. Role of anterior segment optical coherence tomography for safer management of mature white cataracts. J Cataract Refract Surg. 2019;45:480–484. doi:10.1016/j.jcrs.2018.11.009