Abstract
Background
Open globe injuries (OGIs) are a leading cause of monocular blindness worldwide and require prompt intervention to prevent proliferative vitreoretinopathy (PVR) and endophthalmitis when serious intraocular damage occurs. The management of OGIs involves initial wound closure within 24 hours, followed by vitrectomy as a secondary surgery. However, there is a lack of consensus regarding the optimal timing of vitrectomy for maximizing visual outcomes. This meta-analysis aimed to investigate whether early or delayed vitrectomy leads to better outcomes in patients with OGIs.
Methods
This review was conducted based on PRISMA guidelines. The Medline, Embase, Scopus, Cochrane Central Register of Controlled Trials, and ClinicalTrials.gov databases were searched (October 23, 2023). Clinical studies that used vitrectomy to manage OGIs as early (within 7 days) or delayed (8–14 days) interventions were included. Randomized controlled trials (RCTs) and non-RCTs were appraised using the Cochrane risk of bias and JBI tools, respectively.
Results
Eleven studies met the inclusion criteria and were included in the quantitative analyses. There were 235 patients with OGIs who received early intervention and 211 patients who received delayed intervention. The retina was reattached in 91% and 76% of the patients after early and delayed intervention, respectively. Traumatic PVR was present in 9% and 41% of the patients in the early and delayed groups, respectively. The odds of retinal reattachment after vitrectomy were greater in the early group (OR = 3.42, p = 0.010, 95% CI=1.34–8.72), and the odds of visual acuity ≥ 5/200 were 2.4 times greater in the early group. The incidence of PVR was significantly greater in the delayed surgery group (OR = 0.16, p < 0.0001; 95% CI=0.06–0.39), which also required more than one vitrectomy surgery.
Conclusion
Early vitrectomy results in better postoperative visual acuity, a greater proportion of retinal reattachment, and a decreased incidence of PVR.
Introduction
Ocular injuries are the leading cause of monocular blindness worldwide. Depending on the type of eye damage, mechanical injury to the globe is categorized as a closed (CGI) or open globe injury (OGI). An OGI is a full-thickness wound of the eye wall caused by a laceration or rupture. Lacerations are usually caused by sharp objects and are subdivided into penetrating injuries, perforating injuries, and intraocular foreign bodies (IOFBs). Penetrating injuries have an entry point but no clear exit point, whereas perforating injuries have both entry and exit points. On the other hand, rupture is caused by considerable blunt force on the globe, leading to rupture of the globe.Citation1 OGIs have a poorer prognosis than CGIs and can therefore lead to substantial ocular morbidity. Prompt intervention is usually necessary to repair the globe and reduce complications, such as endophthalmitis. The current management suggestion is initial wound closure within 24 hours, followed by secondary surgery, if clinically indicated.Citation2,Citation3
As a secondary surgery, vitrectomy is known to improve the efficacy and prognosis of visual outcomes; however, the optimal timing of vitrectomy remains controversial.Citation3–5 Ocular trauma may affect several structures within the eye to different extents, making it difficult to plan a unified surgical procedure for all patients. One of the major consequences of OGIs is retinal detachment (RD) complicated by traumatic proliferative vitreoretinopathy (PVR), the incidence of which can be significantly reduced if vitrectomy is performed at the right time, as observed in a retrospective study.Citation6
Early vitrectomy performed within a week has been shown to provide better anatomical and visual outcomes than delayed vitrectomy in some studies,Citation7–9 while other studies have shown better results with delayed vitrectomy performed at 8–14 days.Citation10 Therefore, there is a lack of consensus on the optimal timing of vitrectomy for severely injured eyes. This systematic review and meta-analysis aimed to systematically review the literature and assess whether early or delayed vitrectomy improves the anatomical and functional outcomes. The primary objective was to investigate the influence of the timing of vitrectomy on anatomical and functional success, which was determined by the rate of retinal reattachment, while functional success was determined by a postoperative visual acuity of 5/200 or better. The secondary objective was to determine the incidence of traumatic PVR and the number of needed pars plana vitrectomy (PPV) procedures.
Methods
The present systematic review was conducted in accordance with the Preferred Reporting Items for Systematic Review and Meta-analyses (PRISMA) guidelines.Citation11 A systematic review protocol was developed, and the patients strictly adhered to the study protocol. A search strategy [see Appendix 1] was used to identify all articles that reported the use of vitrectomy for OGI management.
Study Eligibility Criteria
Studies were selected for inclusion based on the prespecified population, intervention, comparator, and outcome (PICO) framework (). The aim was to include only randomized controlled trials (RCTs). However, considering the scarcity of RCTs on the topic identified through a preliminary literature search during the protocol writing stage, nonrandomized studies were also included. Conference abstracts, generic reviews, animal studies, and individual case reports were also excluded.
Table 1 PICO Criteria for the Inclusion of Studies
Search Strategy
The following electronic bibliographic databases were searched for clinical trials: MEDLINE, Embase, Scopus, the Cochrane Central Register of Controlled Trials, and Clinical Trials. gov for studies published between 1947 and October 23, 2023. The bibliographies of the included articles were also searched to identify further relevant studies [see Appendix 1].
Data Extraction and Management
Two reviewers (MAQR and EAQG) independently screened titles and abstracts identified in the bibliographic search. Full-text review and data extraction were performed independently, and discrepancies were resolved by mutually comparing the results against the inclusion criteria using Covidence software. The following data were extracted using a standardized platform (Microsoft Excel): first author, year of study publication, study design, mean age and age range of participants, number of eyes included in each group, type of ocular injury, and outcome measures included in the individual studies. The data extracted for the meta-analysis included the frequency of retinal reattachment postvitrectomy, the number of eyes that achieved a visual acuity of 5/200 or better, the number of vitrectomies required until the final follow-up visit, and the incidence of traumatic PVR.
Risk of Bias Assessment
The Cochrane Collaboration tool was used to assess the risk of bias (ROB)Citation12 in the RCTs and prospective cohort studies. These tools incorporate several domains that assess sampling Methods, randomization, reporting bias, and detection bias. The Joanna Briggs Institute (JBI) Critical Appraisal ToolCitation13 was used to assess ROB in the non-RCTs. The JBI tool has eight domains that assess study details regarding sampling, outcome measurement, analysis, and reporting [see Appendices 2 and Appendices 3]. Two reviewers (MAQR and MAQG) independently assessed the risk of bias in each RCT across the six domains. Disagreements were resolved through consensus.
Measures of Effect of Intervention
The primary outcome measures were the odds of retinal reattachment after vitrectomy (anatomical success) and postoperative visual acuity ≥ 5/200 (functional success). The secondary outcome measure was the incidence of traumatic PVR requiring more than one vitrectomy in either group.
Data Synthesis and Analysis
All outcome measures are expressed as odds ratios (ORs) with corresponding 95% confidence intervals (CIs). A random effects model with the restricted maximum likelihood estimation (REML) approach was used to analyze the data, and forest plots were generated. The existence of statistical heterogeneity between studies was evaluated using I2 statistics, where values greater than 50% were considered to represent moderate to considerable heterogeneity.Citation14 A p value < 0.05 was considered to indicate statistical significance. The meta-analysis was performed using R software (version 4.3.1) and the metafor package.Citation15
Results
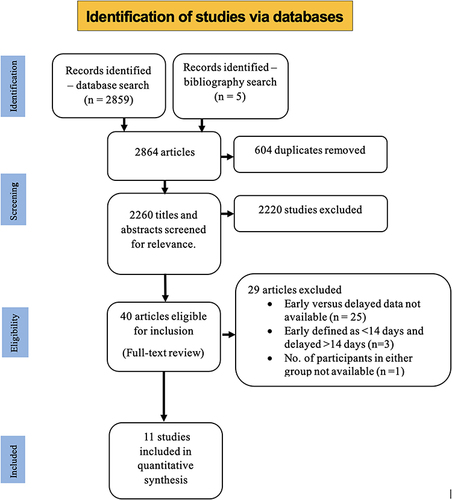
The literature search yielded 2864 articles—2859 through database searches and five through a bibliographic search of the included studies. After removing duplicates, 2260 articles were screened through titles and abstracts, and 40 articles were found to be eligible for a full-text review. Finally, 11 studies met the inclusion criteria and were included in the quantitative synthesis. The PRISMA flowchart for the selection of studies is shown in .
The review included 11 studies,Citation7–10,Citation16–22 one RCT, one prospective cohort study, and nine retrospective observational studies. Among the included studies, six were conducted in the US, three in China and one each in Portugal and Slovenia. This review included 446 patients with OGIs who underwent early vitrectomy within one week (n=235) and delayed vitrectomy between 8–14 days (n=211). The characteristics of the included studies are summarized in and .
Table 2 Characteristics of the Included Non Controlled Studies
Table 3 Characteristics of the Included Controlled Studies
Visual acuity ≥5/200 was achieved in nearly two-thirds of the patients (97/141) in the early group, while it was achieved in one-half of the patients (55/107) in the delayed group. The retina postvitrectomy was reattached in 91% of the patients (83/91) in the early vitrectomy group and 76% of patients (65/86) in the delayed vitrectomy group. Similarly, traumatic PVR was present in 8 of 90 patients (9%) in the early vitrectomy group, while it was present in 36 of 88 patients (41%) in the delayed vitrectomy group. The percentage of patients who underwent more than one vitrectomy was greater in the delayed group than in the early group (26% [15/57 patients in the early group] vs 40% [24/60 patients in the delayed group]). The Results are summarized in .
Table 4 Summary of the Results from the Included Studies
Meta-Analysis
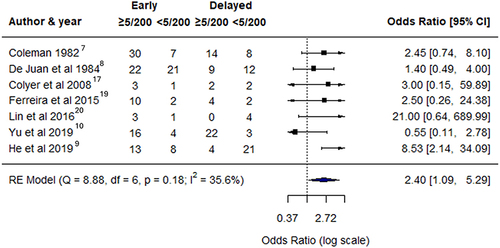
The meta-analysis showed that the odds of retinal reattachment postvitrectomy were significantly greater in the early group than in the delayed group (OR = 3.42, p = 0.010, 95% CI: 1.34–8.72). No heterogeneity was observed in the model fit (Q (df = 4) = 1.9948, I2=0.00%). A forest plot comparing the efficacy of early versus delayed intervention on retinal reattachment postvitrectomy is presented in . Similarly, visual acuity 5/200 or better postvitrectomy was significantly greater in the early group than in the delayed vitrectomy group, with no significant heterogeneity (Q = 8.88, df = 6, I2 = 35.6%). The odds of a visual acuity of 5/200 or better were 2.4 times greater in the early vitrectomy group than in the delayed vitrectomy group (forest plot; ).
Figure 2 The odds of retinal reattachment postvitrectomy were significantly greater in the early group than in the delayed group; ra+, retina reattached; ra-, retina not attached.
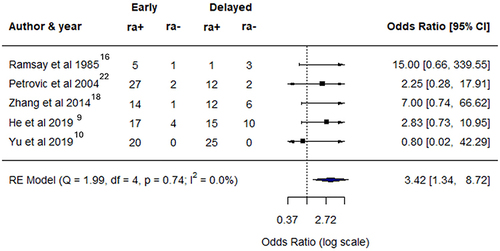
Figure 3 The odds of a visual acuity of 5/200 or better were 2.4x greater in the early group than in the delayed vitrectomy group.
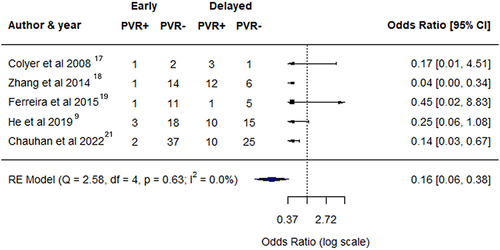
The incidence of PVR was significantly greater in the delayed group (OR = 0.16, p < 0.0001, 95% CI: 0.06–0.39). Early vitrectomy resulted in an 84% reduction in the odds of having PVR compared to delayed vitrectomy. Again, there was no heterogeneity associated with this model (Q = 2.58, df = 4, I2 = 0.00%). The forest plot for the incidence of PVR in early versus delayed vitrectomy patients is presented in . More than one vitrectomy had to be performed in more patients who underwent delayed vitrectomy than in those who underwent early vitrectomy.
Figure 4 Forest plots comparing the odds of proliferative vitreoretinopathy (PVR) in early and delayed intervention after ocular injury. The incidence of PVR was significantly greater in the delayed group.
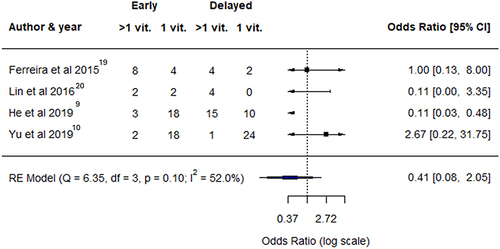
Although there was not very high heterogeneity (Q = 6.35, df =3, I2 = 52.0%) associated with this model, the results did not reach statistical significance (OR = 0.41, p = 0.280, 95% CI: 0.08–2.05) (forest plot; ).
Risk of Bias Assessment
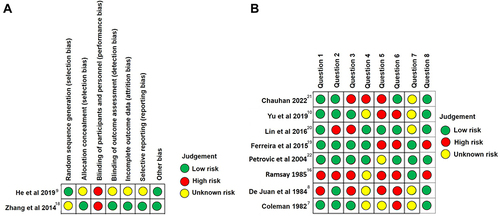
Of the two controlled studies, the one by Zhang et al (2014)Citation18 was assessed to have a low risk of bias in five out of seven domains, whereas the one by He et al (2020)Citation9 was assessed to have an unknown risk of bias across four domains (). Among the noncontrolled studies, six clearly defined their subjects and settings. However, these studies performed poorly when assessed in terms of exposure measurements, criteria used to measure outcomes and controlling for confounding variables ().
Figure 6 (A) Risk of bias assessment of randomized controlled trials. Green indicates a low risk of bias, red indicates a high risk of bias, and yellow indicates an unknown risk of bias. (B). Risk of bias assessment of nonrandomized controlled trials. Green indicates a low risk of bias, red indicates a high risk of bias, and yellow indicates an unknown risk of bias.
Discussion
This systematic review and meta-analysis aimed to determine the influence of vitrectomy timing on OGIs. Previous studies have not provided robust evidence regarding whether early vitrectomy provides effective anatomical and functional outcomes. There are studies that favor early intervention within 72 hours of injury,Citation7,Citation8 within 1 week,Citation9 or delayed vitrectomy within 8–14 days.Citation10 We systematically reviewed the literature, and the meta-analysis revealed significant findings. The results of our study suggest that early vitrectomy within one week provides significant anatomical outcomes (as evidenced by the odds of occurrence of postoperative retinal reattachment) and functional outcomes (as evidenced by significant postoperative visual acuity ≥ 5/200). In particular, we used this cutoff for visual acuity because outcomes better than 5/200 have been described as functional success in the OGI literature.Citation8,Citation16 Similarly, the frequency of PVR was significantly greater in the delayed vitrectomy group than in the early vitrectomy group. These findings suggest that early vitrectomy within one week results in better anatomical and functional outcomes in the management of OGIs.
The results of our review are consistent with those of earlier studies, namely, Coleman et al (1982)Citation7 and De Juan et al (1984)Citation8, who recommended early vitrectomy, preferably within 72 hours of injury, for better visual recovery. These arguments were made more than four decades ago, and interestingly, there has been a scarcity of well-conducted RCTs in this area, which prompted us to include non-RCTs in the present review. Importantly, our findings also support the findings of only one RCT,Citation9 in which better anatomical and visual outcomes were observed in patients who underwent vitrectomy within a week. Similarly, there are also reports of vitrectomy performed later than 28 days, where the risk of PVR occurrence was nearly 240-fold greater than that of early vitrectomy.Citation23 Although we did not investigate the effect of late vitrectomy on PVR development or visual prognosis, our results indicate that the later the vitrectomy is, the worse the prognosis.
However, our findings do not support the use of conventional surgical management for OGIs. In conventional management, also described by Kuhn and Morris as a “mainstream” two-stage approach, wound closure occurs within day 1 of injury, followed by vitrectomy in the second half of the second week.Citation5 Our results are also inconsistent with a more recent finding that delayed vitrectomy is better than early or late vitrectomy.Citation10
The timing of vitrectomy (“when to do it”) is an important factor in the management of OGIs.Citation5 There has been considerable controversy regarding the exact timing of vitrectomy. Early vitrectomy suggests that early intervention helps to prevent the development of fibroblastic tissue within the vitreous cavity, leading to decreased risks of retinal detachment and cyclitic membranes.Citation5 However, delayed vitrectomy has been preferred by some surgeons because of certain benefits. Mittra and MielerCitation4 recommended vitrectomy 7–10 days after injury as a treatment option. Delayed vitrectomy is believed to be less complicated because of the decreased risk of uncontrolled hemorrhage. A delay in vitrectomy also makes the removal of the posterior vitreous easier. However, Ryan and AllenCitation24 believe that the timing of vitrectomy also depends on other factors, such as the presence of endophthalmitis, retinal detachment, IOFB, severe scleral rupture, and long-standing vitreous hemorrhage.
Assessment of ROB
Controlled studies have demonstrated a high risk of bias for most domains. Surgical interventional studies are likely to be inherently variable because of the nature of the surgery involved. Masking of participants and personnel is difficult because both clinicians and patients are involved in the decision-making process. Noncontrolled studies have shown satisfactory results in terms of subject selection. However, these studies performed poorly in describing the treatment plan and criteria used for outcome assessment. Although noncontrolled studies provide lower levels of evidence owing to an increased risk of bias, they have provided valuable information on the treatment outcome and applicability of treatment strategies, as seen in the present study. Therefore, the value of including these studies in the present review is justified because information that can be assessed from RCTs is unavailable. Noncontrolled studies have provided information and informed potential clinical trials in this area.
This study had several limitations. First, there is a dearth of RCTs available. We found only one RCT, and most of the studies included in the review were uncontrolled. Uncontrolled studies are subject to bias, and unlike RCTsCitation25 they do not provide a high level of evidence. Second, we were not able to include a few studies in which enough data for meta-analysis were not available because of inadequate reporting.Citation24,Citation26–31 Third, we studied the effect of early (within 1 week) and delayed (8–14 days) interventions; however, the effects of interventions after 14 days were not present because the search did not provide results available for this review. A network meta-analysis may better explain the effects of interventions with more than two timeframes. Finally, we were unable to assess clinical heterogeneity, which may have affected the outcome. In addition, other factors, such as the preoperative visual acuity, presence of relative afferent papillary defects, zone, location and type of injury, may have affected the outcomes. A subgroup analysis or a meta-regression would have provided more information on the effect of these variables on the outcome measures. However, we did not conduct a subgroup analysis or a meta-regression analysis because of an inadequate number of studies. Despite these limitations, our meta-analysis provided significant results. This review also highlights the paucity of RCTs, and we recommend that additional RCTs in this area are warranted.
Conclusion
Early vitrectomy within 7 days after OGI was associated with better outcomes than delayed vitrectomy between 8–14 days, both of which are approaches after an initial 24-hour globe wound closure. Early vitrectomy leads to better outcomes and is associated with better postoperative visual acuity, greater odds of retinal reattachment, and a decreased incidence of PVR. More RCTs are required to overcome the limitations of this review.
Abbreviations
BCVA, best-corrected visual acuity; CIs, confidence intervals; CGIs, closed globe injuries; IOFBs, intraocular foreign bodies; JBI, Joanna Briggs Institute; NA, not applicable; OGIs, open globe injuries; OR, odds ratio; PICO, population, intervention, comparator, outcomes; PRISMA, preferred reporting items for systematic review and meta-analyses; PVR, proliferative vitreoretinopathy; RCTs, randomized controlled trials; RD, retinal detachment; REML, restricted maximum likelihood; ROB, risk of bias; SD, standard deviation; US, United States; VA, visual acuity.
Ethics and Consent Statements
This study was conducted at the Retina Department of the Oftalmología Integral ABC. Institution in Mexico City, Mexico. The Institutional Review Board approved the study according to institutional guidelines. No reference numbers have been provided for this systematic review and meta-analysis. This study adhered to the tenets of the Declaration of Helsinki and received full approval from the appropriate research ethics committee, institutional review committee, and institutional teaching department.
Author Contributions
All the authors made a significant contribution to the work reported, whether in the conception, study design, execution, acquisition of data, analysis, and interpretation, or in all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; agreed on the journal to which the article has been submitted; and agreed to be accountable for all aspects of the work.
Disclosure
The authors declare no conflicts of interest in this work.
Acknowledgments
We express our deep appreciation to the technical staff of the Retina Department of Oftalmologia Integral ABC (a Medical and Surgical Nonprofit Organization), Mexico City, Mexico, which is affiliated with The Postgraduate Division Studies at the National Autonomous University of Mexico.
Data Sharing Statement
The datasets used in this study have been included in the main text. Photographs and figures from this study may be released via a written application to the Photographic Laboratory and Clinical Archives Retina Department at the Oftalmologia Integral ABC Medical and Surgical Assistance Institution (Nonprofit Organization), Av. Paseo de las Palmas 735 suite 303, Lomas de Chapultepec, Mexico City 11000, Mexico and the corresponding author upon request.
Additional information
Funding
References
- Pieramici DJ, Sternberg PJ, Aaberg S. et al. A system for classifying mechanical injuries of the eye (globe). the ocular trauma classification group. Am J Ophthalmol. 1997;123(6):820–831. doi:10.1016/S0002-9394(14)71132-8
- Blanch RJ, Bishop J, Javidi H, Murray PI. Effect of time to primary repair on final visual outcome after open globe injury. Br J Ophthalmol. 2019;103(10):1491–1494. doi:10.1136/BJOPHTHALMOL-2017-311559
- Aylward GW. Vitreous management in penetrating trauma: primary repair and secondary intervention. Eye. 2008;22(10):1366–1369. doi:10.1038/eye.2008.74
- Mittra RA, Mieler WF. Controversies in the management of open-globe injuries involving the posterior segment. Surv Ophthalmol. 1999;44(3):215–225. doi:10.1016/S0039-6257(99)00104-6
- Kuhn F, Morris R. Early vitrectomy for severe eye injuries. Eye. 2021;35(5):1288–1289. doi:10.1038/S41433-020-01308-W
- Han L, Jia J, Fan Y, et al. The Vitrectomy Timing Individualization System for Ocular Trauma (VTISOT). Sci Rep. 2019;9:1–9. doi:10.1038/s41598-019-48862-2
- Coleman DJ. Early vitrectomy in the management of the severely traumatized eye. Am J Ophthalmol. 1982;93(5):543–551. doi:10.1016/S0002-9394(14)77367-2
- De Juan E, Sternberg P, Michels RG. Timing of Vitrectomy after Penetrating Ocular Injuries. Ophthalmology. 1984;91(9):1072–1074. doi:10.1016/S0161-6420(84)34193-8
- He Y, Zhang L, Wang F, et al. Timing influence on outcomes of vitrectomy for open-globe injury: a prospective randomized comparative study. Retina. 2020;40(4):725–734. doi:10.1097/IAE.0000000000002447
- Yu H, Li J, Yu Y, et al. Optimal timing of vitrectomy for severe mechanical ocular trauma: a retrospective observational study. Sci Rep. 2019;9:1–6. doi:10.1038/s41598-019-54472-9
- Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021:372. 10.1136/BMJ.N71.
- Higgins JPT, Altman DG, Gøtzsche PC, et al. The Cochrane collaboration’s tool for assessing risk of bias in randomized trials. BMJ. 2011;1:343.
- Joanna Briggs Institute. Checklist for systematic reviews and research syntheses. 2017; Available From: https://joannabriggs.org/ebp/critical_appraisal_tools. Accessed june 18 2024.
- Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. Br Med J. 2003;327(7414):557–560. doi:10.1136/bmj.327.7414.557
- Viechtbauer W. Conducting Meta-Analyses in R with the metafor Package. J Stat Softw. 2010;36(3):1–48. doi:10.18637/jss.v036.i03
- Ramsay RC, Cantrill HL, Knobloch WH. Vitrectomy for double penetrating ocular injuries. Am J Ophthalmol. 1985;100(4):586–589. doi:10.1016/0002-9394(85)90686-5
- Colyer MH, Chun DW, Bower KS, et al. Perforating globe injuries during operation Iraqi Freedom. Ophthalmology. 2008:115. 10.1016/J.OPHTHA.2008.05.013.
- Zhang L, Liu Y, Chen S, Wang Y. Clinical observation of the vitreous surgery for open-globe injuries in different timing after the trauma. Chinese J Ophthalmol. 2014;50:121–125. doi:10.3760/CMA.J.ISSN.0412-4081.2014.02.008
- Ferreira N, Monteiro S, Meireles A, Kuhn F. Outcome of vitrectomy and chorioretinectomy in perforating eye injuries. Ophthalmic Res. 2015;53(4):200–206. doi:10.1159/000371494
- Lin H, Lema GMC, Yoganathan P. Prognostic indicators of visual acuity after open globe injury and retinal detachment repair. Retina. 2016;36(4):750–757. doi:10.1097/IAE.0000000000000798
- Chauhan MZ, Georgiou M, Al-Hindi H, Uwaydat SH. Outcomes of pars plana vitrectomy following ocular trauma at varying surgical time points. Int J Retin Vitr. 2022;8(1):1–6. doi:10.1186/S40942-022-00399-9/TABLES/3
- Petrovic MG, Lumi X, Olup BD. Prognostic factors in open eye injury managed with vitrectomy: retrospective study. Croat Med J. 2004;45(3):299–303.
- Feng K, Hu Y, Wang C, et al. Risk factors, anatomical, and visual outcomes of injured eyes with proliferative vitreoretinopathy: eye injury vitrectomy study. Retina. 2013;33(8):1512–1518. doi:10.1097/IAE.0B013E3182852469
- Ryan SJ, Allen AW. Pars plana vitrectomy in ocular trauma. Am J Ophthalmol. 1979;88(3):483–491. doi:10.1016/0002-9394(79)90651-2
- Pannucci CJ, Wilkins EG. Identifying and avoiding bias in research. Plast Reconstr Surg. 2010;126(2):619. doi:10.1097/PRS.0B013E3181DE24BC
- Akincioglu D, Kucukevcilioglu M, Durukan AH. Pars plana vitrectomy timing in deadly weapon-related open-globe injuries. Eye. 2021;35(7):2008–2015. doi:10.1038/s41433-020-01204-3
- Liggett PE, Gauderman WJ, Moreira CM, et al. Pars plana vitrectomy for acute retinal detachment in penetrating ocular injuries. Arch Ophthalmol. 1990;108(12):1724–1728. doi:10.1001/ARCHOPHT.1990.01070140078033
- Phillips HH, Blegen Iv HJ, Anthony C, et al. Pars plana vitrectomy following traumatic ocular injury and initial globe repair: a retrospective analysis of clinical outcomes. Mil Med. 2021;186(Supplement_1):491–495. doi:10.1093/MILMED/USAA286
- Meredith TA, Gordon PA. Pars plana vitrectomy for severe penetrating injury with posterior segment involvement. Am J Ophthalmol. 1987;103(4):549–554. doi:10.1016/S0002-9394(14)74279-5
- Mansouri MR, Tabatabaei SA, Soleimani M, et al. Ocular trauma treated with pars plana vitrectomy: early outcome report. Int J Ophthalmol. 2016;9(5):738–742. doi:10.18240/IJO.2016.05.18
- Salehi-Had H, Andreoli CM, Andreoli MT, et al. Visual outcomes of vitreoretinal surgery in eyes with severe open-globe injury presenting with no-light-perception vision. Graefes Arch Clin Exp Ophthalmol. 2009;247(4):477–483. doi:10.1007/S00417-009-1035-4