Abstract
Background
Idiopathic polypoidal choroidal vasculopathy is an abnormal choroidal vascular pathology similar to age-related macular degeneration. It may present with sudden visual loss from hemorrhagic retinal pigment epithelial detachment and breakthrough vitreous hemorrhage or with chronic recurrent episodes. The condition is not uncommon in the retina clinic at the University College Hospital, Ibadan, Sub-Saharan Africa. This study presents the pattern of presentation in Ibadan.
Methods
We review all cases of idiopathic polypoidal choroidal vasculopathy seen from 2007 to 2012 in the retina clinic at the University College Hospital, Ibadan, to determine the major pattern of presentations, available treatment modalities, and visual outcomes.
Results
Ten cases were seen during the study period. Their mean age was 58 years, with a male to female ratio of 1:4. The most common presenting complaint was sudden visual loss. Major examination findings were retinal pigment epithelial detachment, orange subretinal lesions, and breakthrough vitreous hemorrhage. The modalities of treatment available included vitrectomy to clear vitreous hemorrhage. Intravitreal bevacizumab reduced the height of the pigment epithelial detachment and cleared vitreous hemorrhage. Thermal laser was applied for extrafoveal lesions. Two patients with subfoveal lesions were referred abroad for photodynamic therapy. Visual outcome showed significant improvement in vitrectomized patients who presented with vitreous hemorrhage. Presenting vision of hand motion and light perception improved to vision ranging from counting fingers to 6/12 after vitrectomy.
Conclusion
Idiopathic polypoidal choroidal vasculopathy may not be uncommon in Sub-Saharan Africa. A high index of suspicion is warranted in the diagnosis so as to provide timely intervention.
Introduction
Idiopathic polypoidal choroidal vasculopathy (IPCV) is a choroidal vascular abnormality characterized by sudden visual loss from macular hemorrhage or breakthrough vitreous hemorrhage. Exudation is also common. The condition was often confused with wet age-related macular degeneration until Yannuzzi et alCitation1,Citation2 described it as a separate entity. Early reports described in Asians and patients of dark skin race showed a female preponderance, a younger age, an association with systemic hypertension, and presentation of orange retinal lesions and subretinal hemorrhagic detachment,Citation3,Citation4 but to the best of the authors’ knowledge, not in Sub-Saharan Africans. This study describes the patterns of presentation in ten patients diagnosed with IPCV in Ibadan, Sub-Saharan Africa.
Materials and methods
A retrospective review was done of 10 patients seen in the retina clinic at the Department of Ophthalmology, University College Hospital, Ibadan between 2007 and 2012. The retina register was opened in 2007 after subspecialization in the Department of Ophthalmology at this hospital. Case files of patients with a diagnosis of IPCV vasculopathy were retrieved and studied. The diagnosis was based on clinical findings of subretinal orange lesions, retinal pigment epithelial detachments, subretinal hemorrhagic detachments, and exudates in the absence of drusen, as described in previous reports.Citation1–Citation4 Information extracted from the case file included patient demographics, presenting complaints, and visual acuity. Others included fundus findings, treatment modalities, and visual outcome at 3 months. The data were analyzed as proportions and percentages.
Results
The results are summarized in .
Table 1 Pattern of presentation of idiopathic polypoidal choroidal vasculopathy in Ibadan
Discussion
Idiopathic polypoidal choroidal vasculopathy was described by Yannuzzi et al in hypertensive African Americans with hemorrhagic retinal pigment epithelial detachment in the absence of drusen.Citation1 The present study showed a female preponderance (male to female ratio, 1:4) in the fifth and sixth decades, in keeping with previous reports of younger age than in patients with age-related macular degeneration.Citation4
In a previous report from our center, a total of 768 retinal cases were seen in the hospital over a 3-year period, of which 101 were diagnosed to have age-related macular degeneration, representing 14% of all retinal cases seen. The peak age was at least 60 years, and the male to female ratio was about 2:3. Wet age-related macular degeneration was seen in 40 (40%) of cases. More females presented with wet age-related macular degeneration (26% versus 14%) and the intermediate form, while more males appeared to present with advanced dry age-related macular degeneration (12% versus 5%).Citation5
Sudden visual loss was the commonest presentation in the present study. Bilateral disease occurs in about 70% of the cases. The main findings included breakthrough vitreous hemorrhage, subretinal orange lesions, and hemorrhagic retinal pigment epithelial detachment with subretinal exudates and blood.
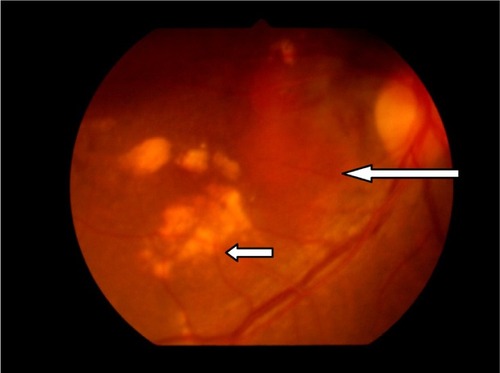
The natural course (, , and ) of the disease includes chronic serosanguinous detachment with preservation of vision. Other patients had hemorrhagic foveal detachment or chronic macular degeneration resulting in profound visual loss. The presentation usually is that of sudden visual loss, some () with a chronic course, some with recurrences, and 50% with favorable visual outcomes.Citation4,Citation6
Figure 1 Idiopathic polypoidal choroidal vasculopathy with chronic subretinal exudate in a 68-year-old woman (patient 1).
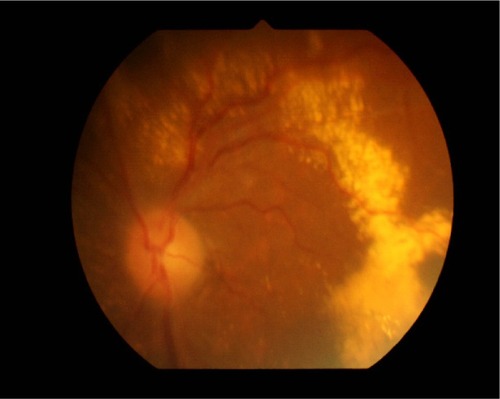
Figure 2 Fundus findings in patient 8 with idiopathic polypoidal choroidal vasculopathy. Right eye (A) with resolved subretinal blood and macular degeneration. (A) subretinal orange lesions (medium arrow); The left eye (B) shows fresh subretinal hemorrhage (long arrow); and (C) retinal pigment epithelial detachment (short arrow). Note the absence of drusen seen in age-related macular degeneration.
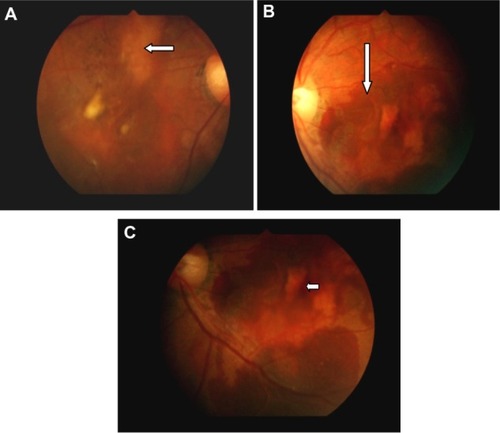
Figure 3 Patient 10 with idiopathic polypoidal choroidal vasculopathy. Orange subretinal lesion (long arrow) and subretinal exudates (short arrow).
Idiopathic polypoidal choroidal vasculopathy is characterized by vascular aneurysmal lesions with interconnecting branches of vessels terminating in polyps. These polyps are prone to developing multiple, recurrent, serosanguinous retinal pigment epithelial detachment and neurosensory retinal detachment due to leakage and/or hemorrhage from the abnormal choroidal vascular lesions.Citation1,Citation2,Citation4
Reported retinal findings include hemorrhagic detachment in about 75% and exudative findings in 25%.Citation6 The present study showed hemorrhagic detachment in about 90% of cases, with breakthrough vitreous hemorrhage in 50% of cases.
The diagnosis of IPCV should be suspected in the presence of hemorrhagic or exudative retinal pigment epithelial detachments in the absence of drusen. However, the definitive diagnosis is established using indocyanine green angiography. This demonstrates the branching vascular network originating from choroidal circulation terminating in aneurysmal dilatation. Indocyanine green angiography uses infrared rays, hence its ability to detect the lesion under blood as opposed to fundus fluorescein angiography.Citation7 Indocyanine green angiography studies showed two types of aneurysmal dilatation, ie, the solitary lesion and clusters resembling grapes. The latter is associated with recurrent bleeding and a poor visual prognosis.Citation3 Indocyanine green angiography and optical coherence tomography are not available in our center, so the diagnosis was based on clinical findings.
Treatment modalities for IPCV include observation for extrafoveal lesions. Thermal laser is suggested for extrafoveal lesions threatening the fovea. Photodynamic therapy has been reported to be effective for subfoveal lesions by causing occlusion of the abnormal choroidal vasculature with improvement in vision.Citation8–Citation14 In the present study, vitrectomy was performed to clear breakthrough vitreous hemorrhage with improvement in vision. Intravitreal bevacizumab helped in clearing vitreous hemorrhage and reducing the height of pigment epithelial detachment. Intravitreal bevacizumab has been demonstrated to be beneficial in IPCV.Citation15 Two of our patients were referred abroad for photodynamic therapy.
Visual outcome in the present study showed significant improvement in vitrectomized patients with vitreous hemorrhage. Presenting vision of hand motion and light perception improved to vision ranging from counting fingers at one meter to 6/12 after vitrectomy. Intravitreal bevacizumab was administered to five patients and found to stabilize vision.
Conclusion
IPCV is not uncommon in Ibadan, Sub-Saharan Africa. Patients presenting with sudden visual loss, vitreous hemorrhage, retinal pigment epithelial detachment, and subretinal exudation in the absence of drusen, should raise an index of suspicion in ophthalmologists in Sub-Saharan Africa.
Acknowledgment
The authors thank the Juvenile Open Angle Glaucoma Study Group for the use of their retinal camera.
Disclosure
The authors declare that no conflict of interest is associated with this study.
References
- YannuzziLAIdiopathic polypoidal choroidal vasculopathyPaper presented at the Macula Society MeetingFebruary 5, 1982Miami, FL
- YannuzziLASorensonJSpaideRFLipsonBIdiopathic choroidal vasculopathyRetina199010181693009
- UyamaMMatsubaraTFukushimaIIdiopathic polypoidal choroidal vasculopathy in Japanese patientsArch Ophthalmol19991171035104210448746
- YannuzziLACiardellaASpaideRRabbMFreundKBOrlockDThe expanding clinical spectrum of idiopathic polypoidal choroidal vasculopathyArch Ophthalmol19971154784859109756
- OluleyeTSIs age related macular degeneration a problem in Ibadan, Sub Sahara AfricaClin Ophthalmol2012656156422536053
- AhujaRMStangaPEVingerlingJRReckACBirdACPolypoidal choroidal vasculopathy in exudative and hemorrhagic pigment epithelial detachmentsBr J Ophthalmol20008447948410781511
- SpaideRFYannuzziLASlakterJSSorensonJOrlachDAIndocyanine green video angiography of idiopathic choroidal vasculopathyRetina1995151001107542796
- SpaideRFDonsoffILamDLTreatment of polypoidal choroidal vasculopathy with photodynamic therapyRetina20022252953512441716
- ChanWMLamDSLaiTYPhotodynamic therapy with verteporfin for symptomatic polypoidal choroidal vasculopathy: one-year result of a prospective case seriesOphthalmology20041111576158415288991
- QuarantaMMauget-FayseeMCoscasGExudative idiopathic polypoidal choroidal vasculopathy and photodynamic therapy with verteporfinAm J Ophthalmol200213427728012140043
- RogersAHGreenbergPBMartidisAPuliafitoCAPhotodynamic therapy of polypoidal choroidal vasculopathyOphthalmic Surg Lasers Imaging200334606312570008
- LeeSCSeongYSKimSSKohHJKwonOWPhotodynamic therapy with verteporfin for polypoidal choroidal vasculopathy of the maculaOphthalmologica200421819320115103216
- Mauget-FaÿsseMQuaranta-El MaftouhiMDe La MarnièrreELeysAPhotodynamic therapy with vertoporfin in the treatment of exudative polypoidal choroidal vasculopathyEur J Ophthalmol200616569570417061220
- HussainNHussainANatarajanSRole of photodynamic therapy in idiopathic polypoidal choroidal vasculopathyIndian J Ophthalmol20055310110415976464
- LaiTYChanWMLiuDTIntravitreal bevacizumab (Avastin) with or without photodynamic therapy for the treatment of polypoidal choroidal vasculopathyBr J Ophthalmol20089266166618356265