Abstract
A 68-year-old woman with bilateral idiopathic optic neuropathy was examined using blue-on-yellow perimetry. Best-corrected visual acuity was 0.5 and 0.6 in her right and left eyes, respectively. Visual field testing with a Goldmann perimeter showed constriction of the I/2 e isopter in both eyes. With regard to mean deviation, the results (−13.18 dB right, −10.01 dB left) of blue-on-yellow perimetry were worse than those obtained using white-on-white perimetry (−1.26 dB right, −1.83 dB left). Optical coherence tomography revealed decreased retinal nerve fiber layer thickness in both eyes. Blue-on-yellow perimetry is useful for the detection of visual field disturbances in patients with optic neuropathy.
Introduction
There are three types of cones in the human retina, with differing sensitivity to long, medium, and short wavelengths. Blue-on-yellow perimetry, or short-wavelength automated perimetry, has gained popularity because of utility in the early detection of glaucomatous visual field loss. This approach to perimetry is designed to evaluate the function of the cones most sensitive to short-wavelength light. A bright yellow background hyperpolarizes the rods as well as cones sensitive to middle- and long-wavelength light, so that only the cones that respond to short-wavelength light are able to detect the target.Citation1 Numerous studies on patients with ocular hypertension or early-stage glaucoma have suggested that defects detectable by blue-on-yellow perimetry can be recognized earlier than the defects that are detectable with white-on-white perimetry.Citation1–Citation6 Furthermore, longitudinal studies of patients with glaucoma have shown that blue-on-yellow visual field defects may progress faster than white-on-white defects.Citation1–Citation6
Short-wavelength stimuli have been used for many years to detect abnormalities in the retina and optic nerve.Citation1 The utility of blue-on-yellow perimetry has been discussed in connection with other retinal diseases such as age-related macular disease, night blindness, and idiopathic blind spot enlargement syndrome.Citation1,Citation7–Citation9 To my knowledge, few reports have investigated the utility of blue-on-yellow perimetry in the treatment of neuro-ophthalmological disorders.Citation1,Citation10–Citation14 Herein, I report the value of blue-on-yellow perimetry in a patient with idiopathic optic neuropathy.
Case report
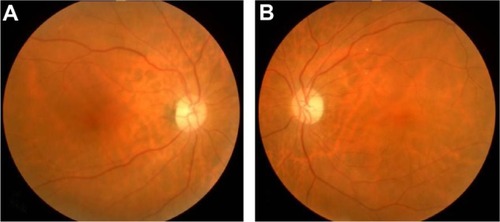
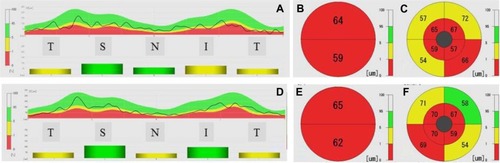
A 68-year-old woman was referred to the Jichi Medical University Hospital due to visual disturbances that began several years ago. Her personal and family history and systemic evaluation were unremarkable. On ophthalmic examination, the best-corrected visual acuity (BCVA) in the right eye was 0.5 with −0.50D−2.50D × 90°; BCVA in the left eye was 0.6 with +0.50D−1.75D × 105°. The patient was orthophoric and showed normal ocular movements. On slit-lamp examination, mild cortical opacities were detected in both lenses. Ocular pressures were normal. The fundus examination showed diffuse optic disc pallor in both eyes ( and ). Visual field testing with a Goldmann perimeter showed constriction of the I/2 e isopter in both eyes ( and ). White-on-white perimetry and blue-on-yellow perimetry were performed using program 24-2 (FASTPAC) of a Humphrey Field Analyzer (model 750; Humphrey Instruments, Inc, Dublin, CA, USA). All testing was performed with an appropriate near add and in adherence with the instructions provided in the Humphrey perimetry manual. All white-on-white perimetry was performed with a 10 cd/m2 white background and a size III white stimulus. Blue-on-yellow perimetry was performed with a 100 cd/m2 yellow background and a size V blue (440 nm) stimulus. All the visual fields included in the data analysis had acceptable visual field reliability indices (fixation loss <20%, false-positive or false-negative responses <33%). The results of blue-on-yellow perimetry were less precise than those obtained using white-on-white perimetry (−13.18 dB right, −10.01 dB left versus −1.26 dB right, −1.83 dB left) (). The pattern standard deviation was also worse with blue-on-yellow perimetry versus white-on-white perimetry (3.89 dB right, 4.03 dB left versus 1.78 dB right, 1.76 dB left) (). Color vision was normal when tested using Ishihara color plates. The patient also passed the Farnsworth dichotomous test. Optical coherence tomography (OCT) (RS-3000; NIDEK, Gamagori, Japan) was used to measure retinal nerve fiber layer (RNFL) thickness in a circular area centered on the optic disc. RNFL thickness measurements were averaged for each quadrant of this circle and for the circular area overall. OCT was also used to map the RNFL, ganglion cell layer (GCL), and inner plexiform layer (IPL). The latter two maps were overlapped to measure retinal thickness at the macula. Measurements were obtained at an inner ring (1.5–4.5 mm from the central fovea) and at an outer ring (4.5–9.0 mm from the central fovea). No measurement was obtained at the central fovea. The results showed decreased retinal thickness at each measurement point (). The decrease was much more marked in the combined NFL, GCL, and IPL map as compared with the RNFL map. In the right eye, mean RNFL thickness at the temporal, superior, nasal, and inferior quadrants was 47, 93, 60, and 75 μm, respectively. In the left eye, these values were 47,110,41, and 96 μm, respectively ( and ). The combined NFL, GCL, and IPL map showed that thickness at the superior and inferior segments was 64 and 59 μm, respectively, in the right eye. In the left eye, these values were 65 and 62 μm, respectively. In addition, combined NFL, GCL, and IPL map revealed that the thickness at the superotemporal, inferotemporal, superonasal, and inferonasal quadrants were 65, 59, 67, and 57 μm, respectively at the inner ring in the right eye. In the left eye, these values were 67, 59, 70, and 70 μm, respectively. Measurements at the outer ring, in the right eye, were as follows: 57, 54, 72, and 66 μm, respectively. In the left eye, these values were 58, 54, 71, and 69 μm, respectively (, , , and ). Comparison with the normative database showed that the combined thickness of the NFL, GCL, and IPL as measured at the inner ring was decreased in comparison with .99% of the population in both eyes.
Figure 2 Right (A) and left (B) Goldmann perimetry showed constriction of the I/2 e isopter in both eyes.
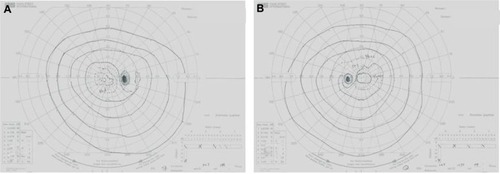
Figure 3 Results of right (A–F) and left (G–L) white-on-white perimetry (A–C and G–I) and blue-on-yellow perimetry (D–F and J–L). Gray-tone scale (A, D, G, and J), total deviation map (B, E, H, and K) and pattern standard deviation map (C, F, I, and L) for white-on-white and blue-on-yellow perimetry. Note that blue-on-yellow perimetry captured the visual field abnormalities more effectively than white-on-white perimetry.
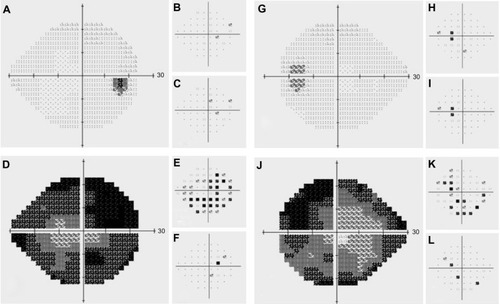
Figure 4 Right (A–C) and left (D–F) optical coherence tomography scans showing decreased retinal thickness.
Abbreviations: RNFL, retinal nerve fiber layer; GCL, ganglion cell layer; IPL, inner plexiform layer; T, temporal; S, superior; N, nasal; I, inferior.
Discussion
Few reports in the literature have used blue-on-yellow perimetry to investigate the functional manifestations of neuro-ophthalmological disorders.Citation10–Citation14 In a report by Keltner and Johnson,Citation10 one patient exhibited hemianopsia on blue-on-yellow perimetry despite a normal performance on standard automated perimetry. The authors evaluated patients with optic neuritis, multiple sclerosis, and other neuro-ophthalmologic disorders using blue-on-yellow perimetry. This approach often revealed more extensive visual field loss than was observed using standard automated perimetry. Wakai et alCitation11 highlighted the utility of blue-on-yellow perimetry in monitoring recovery from optic neuropathy. Their study showed differences between blue-on-yellow and white-on-white perimetry with respect to both the level of visual function as well as the time courses of these changes. They confirmed that blue-on-yellow perimetry evaluated visual field deficits distinct from those evaluated by white-on-white perimetry. The discrepancy stems from the former’s use of a mechanism sensitive to short wavelengths. Walters et alCitation12 evaluated short wavelength-automated perimetry in autosomal dominant optic neuropathy. The results suggested that short wavelength-automated perimetry might be a robust indicator in both early and late stages of this disease. Fujimoto et alCitation13,Citation14 reported on their study of multiple sclerosis patients with quadrantanopia and/or sectoranopia. Blue-on-yellow perimetry is useful in uncovering visual field defects that go undetected by conventional white-on-white perimetry.
Machida et alCitation9 reported on their evaluation of a patient with acute idiopathic blind-spot enlargement syndrome who was evaluated using both white-on-white and blue-on-yellow perimetry. The difference in the mean deviation was significantly greater for blue-on-yellow perimetry as compared with white-on-white perimetry. The authors recommend blue-on-yellow perimetry as a sensitive measure with which to detect retinal dysfunction that is not detected by white-on-white perimetry.
Two possible explanations can be considered for why blue-cone sensitivity is more vulnerable to pathological processes in comparison with other cone systems. First, blue cones may be more delicate physiologically and more susceptible to photoreceptor diseases.Citation9 Second, the response range over which the blue cone functions is significantly limited compared with those of the other cones. Because of this difference, an equivalent loss of response in each cone produces a larger elevation of the threshold in the blue cone system.Citation9
Two factors should be considered for evaluating the results of blue-on-yellow perimetry. The first is the influence of cataract. Kim et alCitation15 demonstrated improvements in mean deviation after cataract surgery in blue-on-yellow as well as white-on-white perimetry. However, the mean deviation change in blue-on-yellow perimetry was far greater than the mean deviation change in white-on-white perimetry. These findings show that cataracts affect visual function as measured by both blue-on-yellow and white-on-white perimetry, but the reduction in blue-on-yellow sensitivity is far greater than that of white-on-white sensitivity.
Although the mean deviation index should be used with great caution when evaluating a patient using blue-on-yellow perimetry, the lens opacities observed in this case did not have a significant effect on the patient’s vision. The second factor to consider is result reproducibility over time. Short- and long-term fluctuations in the visual fields of normal subjects were greater when measured by blue-on-yellow perimetry versus white-on-white perimetry.Citation16
With respect to the OCT findings, Ito et alCitation17 found that RNFL thickness in the macular area was significantly reduced in patients with autosomal dominant optic neuropathy as compared with normal subjects. This trend was true at all measured data-points, especially at 1 mm from the fovea. Combined thickness of the GCL, IPL, inner nuclear layer, and outer plexiform layer as measured in the macular area were significantly reduced compared with the values measured in normal patients. Takasugi et alCitation18 also demonstrated atrophy of the peripapillary RNFL in autosomal dominant optic neuropathy.
In conclusion, the above results showed that blue cone sensitivity is diffusely depressed in eyes with optic neuropathy. Furthermore, blue-on-yellow perimetry represents a sensitive method with which to detect retinal dysfunction that is not detected by white-on-white perimetry. Finally, the conclusions that can be drawn from these findings are limited due to the nature of the study. The reader must consider that these findings were based on a single case of idiopathic optic neuropathy. Additional studies with additional cases will be necessary.
Disclosure
There are no conflicts of interest in relation to this paper.
References
- SamplePAShort-wavelength automated perimetry: it’s role in the clinic and for understanding ganglion cell functionProgr Retin Eye Res200019369383
- TeesaluPAiraksinenPJTuulonenABlue-on-yellow visual field and retinal nerve fiber layer in ocular hypertension and glaucomaOphthalmology1998105207720819818609
- MokKHLeeVWNerve fiber analyzer and short-wavelength automated perimetry in glaucoma suspects. A pilot studyOphthalmology20001072101210411054341
- YamazakiYMizukiKHayamizuFTanakaCCorrelation of blue chromatic macular sensitivity with optic disc change in early glaucoma patientsJpn J Ophthalmol200246899411853721
- ArvindHGrahamSLeaneyJIdentifying preperimetric functional loss in glaucoma. A blue-on-yellow multifocal visual evoked potentials studyOphthalmology20091161134114119395037
- ZhongYZhouXChengYXieLRelation between blue-on-yellow perimetry and optical coherence tomography in normal tension glaucomaCan J Ophthalmol20104549450020648075
- RemkyAElsnerAEBlue on yellow perimetry with scanning laser ophthalmoscopy in patients with age related macular diseaseBr J Ophthalmol20058946446915774925
- TerasakiHMiyakeYNomuraRHoriguchiMSuzukiSKondoMBlue-on-yellow perimetry in the complete type of congenital stationary night blindnessInvest Ophthalmol Vis Sci1999402761276410509678
- MachidaSHaga-SanoTKizawaJTazawaYDecrease of blue cone sensitivity in acute idiopathic blind spot enlargement syndromeAm J Ophthalmol200413829629915289145
- KeltnerJLJohnsonCAShort-wavelength automated perimetry in neuro-ophthalmologic disordersArch Ophthalmol19951134754817710398
- WakaiMTakadaRSuzukiKTrakagiMHasegawaSAbeHComparison of Humphrey white-in-white and blue-on-yellow perimetry in monitoring recovery from optic neuropathyFolia Ophthalmol Jpn19974813191323
- WaltersJWGaumeAPateLShort wavelength-automated perimetry compared with standard achromatic perimetry in autosomal dominant optic atrophyBr J Ophthalmol2006901267127016837542
- FujimotoNAdachi-UsamiEUse of blue-on-yellow perimetry to demonstrate quadrantanopsia in multiple sclerosisArch Ophthalmol19981168288299639464
- FujimotoNKubotaMSaekiNAdachi-UsamiEUse of blue-on-yellow perimetry for detection of sectoranopiaEye20041833834115004597
- KimYYKimJSShinDHKimCJungHREffect of cataract extraction on blue-on-yellow visual fieldAm J Ophthalmol200113221722011476682
- KwonYHParkHJJapAUgurluSCaprioliJTest-retest variability of blue-on-yellow perimetry is greater than white-on-white perimetry in normal subjectsAm J Ophthalmol199812629369683146
- ItoYNakamuraMYamakoshiTLinJYatsuyaHTerasakiHReduction of inner retinal thickness in patients with autosomal dominant optic atrophy associated with OPA1 mutationsInvest Ophthalmol Vis Sci2007484079408617724190
- TakasugiMHayashiTOkudeSAssessment of macular function in dominant optic atrophy associated with mutation in the OPA1 geneJpn Orthopt J201039117122