Abstract
Of all the treatments currently used to lower intraocular pressure in glaucoma patients, filtration surgery is known to be the most effective. However, in a significant percentage of cases, the constructed channel closes due to excessive scar formation, resulting in surgical failure. The process of postoperative wound healing is characterized by the coagulative and inflammatory phase, followed by the proliferative and repair phase, and finally the remodeling phase. Perioperative antimitotic agents, such as mitomycin C and 5-fluorouracil, are known to modulate the process of wound healing and to improve surgical outcome, but they carry a risk of vision-threatening complications. New alternative strategies to prevent filtration failure, such as inhibition of transforming growth factor-β, vascular endothelial growth factor, and placental growth factor, have shown promising results in the improvement of surgical success. However, it remains necessary to broaden the therapeutic approach by focusing on combined therapies and on extended drug delivery.
Introduction
The most effective treatment to lower intraocular pressure (IOP) in glaucoma patients is glaucoma filtration surgery. Trabeculectomy, the reference procedure, is a surgical technique by which a tunnel is created between the anterior chamber and the subconjunctival space, with removal of a part of the trabecular meshwork. A controlled leaking area for aqueous humor is formed, called a filtration bleb. Although this procedure may be crucial in the management of glaucoma,Citation1,Citation2 it carries a risk of complications. Excessive postoperative wound healing of the conjunctiva and Tenon’s capsule, with subsequent scarring, is known to frequently lead to surgical failure,Citation3 associated with poor postoperative IOP control and consequent progression of glaucomatous disc cupping and visual field loss.
Pharmacological enhancement of trabeculectomy using different antiscarring agents was found to significantly improve surgical success rates. Indeed, the use of 5-fluorouracil and mitomycin C, known as the gold standards in clinical practice, has improved the success rate significantly by enhancing bleb survival. However, long-term success rates for blebs supplemented with these antimitotics were not as promising as desired. Moreover, the nonspecific mechanism of action of these agents may result in severe vision-threatening side effects, such as corneal toxicity, thin-walled avascular blebs, blebitis, endophthalmitis, and hypotony. Therefore, there is still a need for alternative strategies to prevent filtration failure. In this review, an overview of the current wound healing modulation agents is provided, and new approaches to wound modulation that may improve glaucoma filtration surgery are discussed.
Process of wound healing
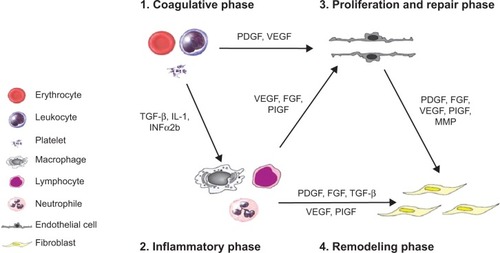
Wound healing comprises a cascade of different processes that are closely linked, and includes a coagulative and inflammatory phase, followed by a proliferation and repair phase, and finally a remodeling phase.Citation4 gives a schematic overview of the wound healing process and the various molecules (growth factors, cytokines, and proteinases) involved in the different phases. After injury, leakage of plasma proteins (fibrinogen, fibronectin, and plasminogen) and blood cells (red and white blood cells and platelets) from disrupted blood vessels takes place. Clotting factor activation leads to conversion of fibrinogen to fibrin, to reduce blood loss. Clots as well as hormones (histamine, serotonin, prostaglandins and leukotrienes), cytokines (eg, interleukin-1 and interferon-α2b) and growth factors (eg, vascular endothelial growth factor [VEGF], placental growth factor, platelet-derived growth factor, fibroblast growth factor, and transforming growth factor [TGF]-β), released during vascular injury, lead to cellular migration and attraction of neutrophils, macrophages, and lymphocytes to the damaged tissue during the inflammatory phase. This results in a proliferative and repair phase during which endothelial cells and fibroblasts migrate into the site of injury. In this phase, angiogenesis and formation of granulation tissue occurs. Finally, remodeling of tissue takes place and involves the formation of scar tissue. Blood vessels regress over time, and fibroblasts induce crosslinking of collagen type I and elastin, which leads to collagen supercoil formation and dense scar tissue.Citation4,Citation5 After trabeculectomy, wound healing under the scleral flap may play a role in some cases, but Tenon fibroblasts are regarded as the key players in the initiation of wound healing and fibrotic scar formation.Citation6 Although it is known that bleb failure in humans normally happens at around 2–3 months,Citation7,Citation8 proliferation of subconjunctival fibroblasts already occurs on postoperative days 3–5.Citation9 The further development of conjunctival fibrosis, regulated by the release of a number of cytokines and growth factors, appears as a result of inflammation, angiogenesis, progressive fibroblast proliferation and migration, and collagen deposition at the site of filtration.Citation4
Figure 1 Schematic overview of the process of wound healing and the most important molecules (growth factors, cytokines, and proteinases) involved.
Modulators of wound healing in clinical practice
Gentle handling of tissue and control of intraoperative bleeding lead to reduced fibroblast activity, but such preventive maneuvers are usually insufficient to prevent scarring in the long term.Citation4 Therefore, various anti-inflammatory and antiproliferative agents are used in clinical practice to inhibit wound healing and to improve bleb survival.
Anti-inflammatory agents
Inhibition of inflammation and wound healing by corticosteroids is largely mediated by suppression of leukocyte concentration and function, as well as by their effects on vascular permeability. This leads to less local tissue disruption, reduced mitogen and growth factor release, and less clot and fibrin production, resulting in diminished fibroblast activity and wound healing.Citation4 Corticosteroids are therefore frequently used as anti-inflammatory agents after glaucoma filtration surgery. Theoretically, they carry a risk of inducing a steroid response, resulting in elevated IOP. It is known that approximately 18%–36% of the general population is steroid-responsive, but this prevalence can increase to 46%–92% in patients with primary-open angle glaucoma.Citation10 It is clear that steroid-induced ocular hypertension is associated with specific morphological changes in the trabecular meshwork, such as an increased deposition of extracellular matrix and altered trabecular meshwork cell function, which in turn will cause disturbed aqueous humor outflow and an increase in IOP.Citation11 Although these morphological changes in the trabecular meshwork still exist after glaucoma filtration surgery, it is known that steroid response is less common after surgery, presumably because the aqueous humor bypasses the trabecular meshwork via the created channel. Indeed, it has been shown that aqueous flow after surgery is reduced through the trabecular pathway, and that after a successful trabeculectomy, the diameter of Schlemm’s canal decreases, most likely due to underperfusion of the trabecular meshwork.Citation12,Citation13 This may explain why only 17%–36% of operated glaucoma patients develop a steroid-induced rise in IOP after trabeculectomy,Citation14 whereas the risk in nonoperated glaucoma patients is much higher (46%–92%).Citation10 Moreover, a ten-year follow-up of a prospective randomized trial of postoperative corticosteroids after trabeculectomy showed that IOP was stabilized in 82.8% (38 of 46 eyes) of steroidtreated eyes after successful glaucoma surgery.Citation15 Finally, it has been suggested that the risk of a steroid response might increase after filtration failure, since the aqueous humor must again flow through the altered trabecular meshwork.Citation16 Also, nonsteroidal anti-inflammatory drugs suppress the inflammatory response in the process of wound healing, but are known to be less potent as compared with corticosteroids.Citation17
Antimitotics
In the early 1980s, antimitotic agents, such as 5-fluorouracil and mitomycin C, were found to be effective in inhibiting activation of fibroblasts. Although these agents have impacted the success rate of glaucoma filtration surgery, they carry a risk of vision-threatening complications. With lower levels of exposure, bleb-related complications are less frequent, but filtration failure is more common, representing a trade-off between efficacy and safety.
5-Fluorouracil
The antiproliferative effect of 5-fluorouracil (Hoffman-La Roche Ltd., Basel, Switzerland), a chemotherapeutic agent, is mediated by antagonizing pyrimidine metabolism. It interferes with the synthesis of thymidine nucleotides, resulting in inhibition of DNA synthesis and ultimately in cell death.Citation18 Khaw et al showed that 5- fluorouracil is an effective inhibitor of fibroblast growth. A five-minute exposure resulted in arrest of growth and had a long-lasting effect on human Tenon fibroblasts.Citation19 Animal studies demonstrated that adjunctive 5-fluorouracil following trabeculectomy resulted in prolonged bleb survival with decreased scarring and fibroblast proliferation compared with no 5-fluorouracil.Citation20 Use of 5-fluorouracil at high levels, however, frequently leads to corneal toxicity and apoptosis, since 5-fluorouracil is toxic to all actively replicating tissues, such as corneal epithelium.Citation21
Mitomycin C
Mitomycin C (Kyowa Hakko Kirin Co., Ltd., Princeton, NJ, USA), is another chemotherapeutic agent with antiproliferative properties. It undergoes metabolic activation via reduction into an alkylating agent that cross-links DNA. Mitomycin C not only inhibits DNA replication, but also mitosis and synthesis of proteins, since it can interfere with any phase in the cell cycle.Citation4 Inhibition of the proliferative phase of the wound healing pathway by mitomycin C increases the success rate of glaucoma surgery, mainly through inhibition of proliferation of fibroblasts and endothelial cells.Citation22 Importantly, different aspects of mitomycin C administration, including dose and exposure time, can determine the outcome of success and affect the wound healing process. It is indeed known that brief intraoperative application of mitomycin C (2–2.5 minutes) is as effective for improvement of surgical outcome as a long exposure (5 minutes),Citation23,Citation24 whereas a low dose of mitomycin C (0.002%) shows reduced effectiveness as compared with a higher dose (0.02%).Citation25 In addition to dose and duration of application, the size of the surface area can also affect the surgical outcome. Indeed, a large area treated with mitomycin C is more effective in achieving and maintaining target IOP, and the incidence of bleb scarring is lower compared with eyes with small areas of application.Citation26–Citation28 Moreover, Cordeiro et al reported that diffuse noncystic blebs were observed more often in rabbits treated with large sponges (8×10 mm) than in those treated with small sponges (4×2 mm).Citation29 Khaw et al showed that mitomycin C is more potent than 5-fluorouracil.Citation30,Citation31 They found that fibroblasts cultured from rabbit samples treated with mitomycin C still induced inhibition of growth at one month, while fibroblasts from 5-fluorouracil-treated rabbits demonstrated full recovery from growth arrest after 7 days. This can be explained by their different mode of action, since it is known that mitomycin C induces permanent apoptosis through activation of caspase-3 and caspase-9, Fas, Bad, and phosphorylated p53 in human Tenon fibroblasts, while this is not the case after administration of 5-fluorouracil.Citation32 Mitomycin C-related cytological toxicity and apoptosis has been associated with the development of thin-walled avascular blebs, which carry a risk of hypotony and endophthalmitis.Citation33 Comparative clinical trials demonstrated that 5-fluorouracil was associated with fewer side effects than mitomycin C, but seemed to be less efficient in improving the surgical outcome.Citation34–Citation36
Altogether, although these anti-inflammatory and antimitotic agents were found to be effective in inhibiting the process of wound healing in clinical practice, they are not sufficiently effective to satisfactorily inhibit scarring after filtering surgery, and some carry a risk of severe side effects. Therefore, there is still a need for new approaches in modulation of wound healing to prevent filtration failure.
State of the art in modulation of wound healing
The aqueous humor flowing through the constructed channel into the bleb after glaucoma surgery contains a large number of growth factors. It is known that the presence of growth factors in the aqueous humor of patients with glaucoma can increase the proliferation of Tenon fibroblasts by 60% compared with the aqueous humor of normal persons.Citation37 As such, pre-existing elevated aqueous levels of these growth factors may put patients with glaucoma at a higher risk of scarring after filtration surgery. Therefore, the upregulated growth factors in the aqueous humor of patients with glaucoma can be considered as potential targets in the development of new wound modulation agents. Indeed, a number of growth factor inhibitors have been investigated to improve the surgical outcome after glaucoma filtration surgery. represents an overview of the new wound modulation agents.
Table 1 New wound modulation agents
Inhibition of TGF-β
TGF-β is a key cytokine in the process of wound healing and has been found to be present at significantly higher levels in the aqueous humor of patients with glaucoma than in that of normal individuals.Citation38 Moreover, TGF-β2 is known to stimulate proliferation of human Tenon fibroblasts in vitro and to enhance fibroblast-mediated collagen contraction.Citation39 Therefore, the strategy of inhibiting this growth factor has been extensively investigated by a group led by Professor PT Khaw (Moorfields Eye Hospital and UCL Institute of Ophthalmology, London, UK). Blocking TGF-β2 with a recombinant human monoclonal antibody (CAT-152, Cambridge Antibody Technology, Cambridge, UK) seemed promising with regard to proliferation of Tenon fibroblasts and in an animal model. Khaw’s group investigated CAT-152 as an adjunct to glaucoma filtration surgery in a rabbit model and showed that repeated subconjunctival injections (1 mg/mL on postoperative days 0, 1, 2, 3, and 7) significantly improved the surgical outcome and bleb survival compared with controls. Histologically, CAT-152-treated eyes showed less collagen deposition and clear evidence of bleb formation, without side effects.Citation40 A clinical study was initiated but was terminated prematurely due to lack of efficacy at the dose used (1 mg/mL).Citation41 Decorin, a naturally occurring TGF-β inhibitor, also significantly altered conjunctival scarring and the surgical outcome of glaucoma filtration surgery in rabbits, but no clinical data are available as yet.Citation42 Inhibition of TGF-β2 by other agents, such as suramin (Bayer AG, Leverkusen, Germany),Citation43,Citation44 tranilast (Kissei Pharmaceutical Co., Ltd., Matsumoto City, Japan),Citation45–Citation47 lovastatin (Merck & Co., Inc., Whitehouse Station, NJ, USA),Citation48 and ALK5 inhibitors,Citation49,Citation50 has also been attempted in in vitro and animal studies, with promising results. A novel approach for targeting the TGF-β signaling pathway, currently under investigation, is the use of microRNA;Citation51 however, confirmation in animal studies is required.
Inhibition of VEGF
VEGF is known to play an important role in scar formation.Citation52 Increased concentrations of VEGF have been demonstrated in the aqueous humor from eyes of patients with glaucoma when compared with nonglaucomatous controls.Citation53–Citation55 In addition to being a potent inducer of angiogenesis, VEGF promotes the migration of inflammatory cells (such as neutrophils and macrophages) and fibroblasts. This growth factor indirectly stimulates fibrosis via angiogenesis, and also has a direct effect on the activity of fibroblasts.Citation56–Citation58 Therefore, VEGF inhibitors were investigated by several groups as a potential antiscarring adjunct to filtration surgery.
Our group showed for the first time in a rabbit model of glaucoma filtration surgery that a single subconjunctival (2.5 mg) and intracameral (5 mg) injection of bevacizumab (Genentech, Inc., San Francisco, CA, USA) was effective in improving the outcome of glaucoma surgery by increasing bleb area and survival. This was associated with a reduction in angiogenesis during the initial phase of healing and with diminished fibrosis in the later stages.Citation53 When compared with blebs treated with 5-fluorouracil (5 mg), those treated with the VEGF inhibitor (1.25 mg) survived longer,Citation59 and combining bevacizumab (2.5 mg) and 5-fluorouracil (5 mg) resulted in 100% bleb survival and a greater antifibrotic effect compared with monotherapy using each inhibitor.Citation60 Importantly, the various VEGF inhibitors available differ in their isoform selectivity, with implications for both efficacy and safety. Based on their VEGF isoform targets, two types of VEGF inhibitors have been identified, ie, selective and nonselective. The effect of pegaptanib (Pfizer Inc., New York, NY, USA), a selective VEGF165 inhibitor, on surgical outcome in a rabbit model of glaucoma surgery was less pronounced than that of nonselective VEGF inhibition, due to a retained action of the VEGF121 and VEGF189 isoforms. It is indeed known that Tenon fibroblasts proliferation is mainly induced by these isoforms, while VEGF165 has less pronounced effects on Tenon fibroblasts.Citation61
Meanwhile, a number of clinical case reports and case series have also shown a beneficial effect of subconjunctival (1, 1.25, and 2.5 mg) and topical (5 mg/mL) bevacizumab, a nonselective VEGF inhibitor, in reducing IOP and improving the surgical outcome.Citation62–Citation67 These studies also demonstrated that the antibody against VEGF is safe for ocular use. An early pilot study to evaluate a single subconjunctival bevacizumab injection (1.25 mg) demonstrated that this VEGF inhibitor is a potential adjunctive treatment for reducing the incidence of bleb failure after trabeculectomy. Six-month outcomes showed that trabeculectomy was successful in terms of IOP control in eleven of 12 eyes (92%), with an average IOP reduction of 52%.Citation68 This beneficial effect was confirmed in more recent studies indicating no significant differences between subconjunctival bevacizumab (1.25 and 2.5 mg) and mitomycin C (0.03% for 3 minutes) in terms of morphological bleb features and IOP-lowering.Citation69,Citation70
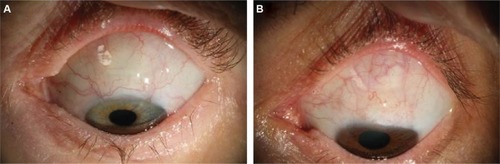
On the other hand, four further pilot studies showed that administration of bevacizumab (0.2 and 1.25 mg) during trabeculectomy did not affect IOP differently from placeboCitation71 or 5-fluorouracil (5 and 7.5 mg).Citation72–Citation74 Notably, all these studies included small numbers of patients or had a short follow-up duration, meaning that they lacked the necessary power to draw firm conclusions. Therefore, our group at the University Hospitals of Leuven performed a prospective, randomized, double-blind, placebo-controlled trial in which a 12-month follow-up was undertaken in 138 patients, 69 of whom were treated with bevacizumab (1.25 mg by intracameral injection). The absolute success rate was higher in the bevacizumab group than in the placebo group (71% versus 51%, respectively), with the need for IOP-lowering interventions (needlings) being lower after bevacizumab treatment (12% versus 33%).Citation75 shows blebs from the bevacizumab and placebo groups at 6 months of follow-up. Bevacizumab-treated eyes showed less vascularity than those treated with placebo. These recent insights open up promising perspectives for the use of anti-VEGF therapy to prevent filtration failure after glaucoma surgery.
Figure 2 Representative blebs from (A) bevacizumab group and (B) placebo group showing less vascularity in the bevacizumab-treated eye at 6 months postoperatively.
Inhibition of placental growth factor
Importantly, although bevacizumab could improve the surgical outcome by inhibiting angiogenesis and deposition of collagen, and VEGF is known to have proinflammatory properties, neither selective nor nonselective VEGF inhibition could reduce inflammation, another important process in postoperative healing.Citation53,Citation61 Our group showed that the upregulated levels of aqueous placental growth factor after administration of bevacizumab might explain why anti-VEGF therapy was not sufficient to reduce the inflammatory response after glaucoma surgery. Indeed, aqueous placental growth factor levels were significantly upregulated in patients with glaucoma compared with control subjects. Moreover, intracameral injection of anti-placental growth factor antibody (5.2 μg, ThromboGenics NV, Leuven, Belgium) effectively improved the surgical outcome in a mouse model of trabeculectomy, by increasing the bleb area and survival after surgery compared with an irrelevant antibody control and with the VEGF-R2 antibody. The effect on surgical outcome was associated with a decreased angiogenesis, fibrosis, and importantly, inflammation. Therefore, inhibition of placental growth factor might theoretically be even more effective than inhibition of VEGF, due to the additional effect on inflammation.Citation76
Other growth factors, cytokines, and proteinases
Several other molecules, including growth factors (eg, platelet-derived growth factor) cytokines (eg, interleukin-6, interleukin-8, and tumor necrosis factor-α), and matrix metalloproteinases (eg, MMP-2 and MMP-3) have been reported to be upregulated after glaucoma filtration surgery.Citation77–Citation80 Different studies have shown that these factors can stimulate proliferation of Tenon fibroblasts in vitro.Citation81,Citation82 Moreover, inhibition of some of these factors reduced growth of Tenon fibroblastsCitation83 and improved surgical outcome in a rabbit model of glaucoma.Citation84,Citation85 However, none of these inhibitors have reached clinical trials. This can probably be explained by the fact that upregulation of TGF-(β2 and VEGF in patients with glaucoma correlates strongly with surgical failure, whereas other factors (eg, MMP-1, interleukin-6, and interleukin-8) are associated with surgical success.Citation86
Inhibition of ROCK
Rho kinases (ROCK 1 and 2) are major downstream effectors of Rho-GTPase proteins and mediate a number of important cellular functions associated with cytoskeletal rearrangement, such as cell morphology, motility, adhesion, contraction, and cytokinesis.Citation87 It is known that ROCK plays an important role in a number of wound healing processes, ie, inflammation, angiogenesis, and fibrosis. Administration of ROCK inhibitors on lipopolysaccharide-stimulated inflammatory cells decreased the activation of NF-κβ and subsequently blocked the generation of proinflammatory cytokines, such as interleukin-1β/6 and tumor necrosis factor-α.Citation88–Citation90 Increased expression of RhoA in endothelial cells also significantly enhanced migration and angiogenic capacity in vitro, which suggests an important role for the Rho/ROCK pathway in these processes.Citation91 Furthermore, van Niew-Amerongen et al showed demonstrated that inhibition of the Rho/ROCK pathway attenuated VEGF-mediated migration and angiogenesis in vitro.Citation92 Importantly, in vitro studies also showed that contractility of Tenon fibroblasts is essential in the transdifferentation into myofibroblasts. Inhibition of the Rho/ROCK pathway by specific kinase inhibitors (Y-27632 [Novartis AG, Basel, Switzerland], HA-1077 [Santen Pharmaceutical Co., Ltd., Osaka, Japan], H-1152 [Calbiochem®; Merck KGaA, Darmstadt, Germany], and ML-7 [Merck KGaA]) is known to counteract this contraction by blocking TGF-β or lysophospholipid acid-induced activation of Tenon fibroblasts.Citation93,Citation94 Secondly, Honjo et al showed that topical treatment with the ROCK inhibitor Y-27632 had profound effects on surgical outcome in a rabbit model of glaucoma surgery. Histological examination revealed that blebs treated with Y-27632 lacked significant collagen deposition compared with vehicle treatment.Citation93 As such, ROCK inhibitors could strengthen our armamentarium to improve the effectiveness of filtration surgery, because these inhibitors have the potency to interfere at different levels of the wound healing process.
Future perspectives
Although bevacizumab has been proven to be effective in reducing wound healing after filtering glaucoma surgery in a prospective clinical trial, mitomycin C is still the most common antifibrotic agent used during trabeculectomy in routine clinical practice. This study may represent a breakthrough in the quest for novel antifibrotic strategies in filtering surgery; however, some additional questions remain to be answered. The most optimal route of administration of anti-VEGF drugs is still unknown. Nomoto et al showed that, despite lower maximal concentrations of bevacizumab after subconjunctival injection in the rabbit eye, the intraocular half-life was higher after subconjunctival injection as compared with intravitreal injection.Citation95 Ambati et al showed that immunoglobulin G antibodies have a relatively high scleral permeability.Citation96 Since bevacizumab is an immunoglobulin G1 antibody, it should penetrate intraocular tissues via the sclera, which might then work as a sustained-release mechanism. Recent studies in a rabbit model of glaucoma surgery showed that postoperative subconjunctival injection of bevacizumab was more effective than intravitreal administration.Citation97 It also remains unknown whether bevacizumab could replace antimitotics in clinical practice, or if it should be considered as an adjunctive to antimitotics. Although some small comparativeCitation69,Citation70,Citation98 and complementary studiesCitation99,Citation100 have been performed, large randomized clinical trials are still lacking.
A variety of alternative antiscarring strategies (), such as photodynamic therapy,Citation101–Citation104 saratin (Merck KGaA),Citation105,Citation106 sonepcizumab (Lpath, Inc., San Diego, CA, USA),Citation107 doxycycline (Pfizer Inc.),Citation108 pirfenidone (InterMune, Brisbane, CA, USA),Citation109,Citation110 tacrolimus (Astellas Pharma Inc., Tokyo, Japan),Citation111 and octreotide (Novartis),Citation111 have also shown promising results by improving the outcome of surgery in a standard rabbit model. Although many agents have been evaluated in preclinical models for glaucoma filtration surgery, few have been found to be beneficial in large prospective comparative clinical trials and none have replaced mitomycin C or 5-fluorouracil in clinical practice so far. Therefore, it is necessary to broaden the therapeutic approach, given that treatment with a single agent may lead to drug resistance. Indeed, because of the complexity of the wound healing process,Citation4,Citation5 it is possible that targeting one molecule may be insufficient to impede the wound healing process due to the upregulation of other growth factors. It has been suggested that mitomycin C can upregulate proinflammatory, proangiogenic, and/or profibrotic factors. Therefore, combining mitomycin C with drugs that block these upregulated profibrotic growth factors may offer promising complementary efficacy and allow a lower dose of mitomycin C to be used, with fewer side effects.
Finally, wound healing is a relatively slow process involving interaction between the antiscarring agent and the target tissue (Tenon’s capsule) for several weeks to months. Therefore, future research should focus on the development of targeted drug delivery systems that improve and/or prolong contact between the target tissues and the antiscarring molecules. A few studies have already been published in which a slow-release formulation of 5-fluorouracil is described. Collagen plugs,Citation112 polyesters,Citation113 and amniotic membranesCitation114 containing the antimitotic agent were shown to induce a prolonged effect on bleb survival in the standard rabbit model. The effect of a sustained-release dexamethasone implant (Ozurdex®, Allergan, Irvine, CA, USA) on postoperative wound healing was also investigated in this animal model, and was found to be effective in prolonging bleb survival. However, mitomycin C-treated blebs showed significantly longer survival compared with Ozurdex-treated blebs.Citation115
Khalili et al developed a new solid tissue tablet that provides prolonged release of bevacizumab in vitro, and an in vivo study showed substantially prolonged bleb survival compared with mitomycin C in the rabbit model.Citation116 Thus, this antibody tablet has the potential to prolong local antibody release and exert a significant biological effect. These data are very promising, but further studies are required. If successful, such improved drug delivery systems might significantly improve the efficacy of known antiscarring molecules and possibly decrease their side effects.
Conclusion
Failing filtering surgery due to an excessive healing reaction is still a considerable problem in ophthalmology, and contributes to progressive vision loss in patients with glaucoma. Although a number of studies have demonstrated that many antifibrotic agents can reduce postoperative wound healing in the preclinical setting, bevacizumab is the only agent that has been proven to be effective in a prospective randomized clinical trial. Further research should focus on targeting multiple steps of the wound healing process by use of combination therapy and also on new methods of extended drug delivery to improve the efficacy of the known antiscarring agents. Finally, we should be cautious when extrapolating preclinical findings to the management of human disease. Animal models are not precise replicas of human pathology, and the pharmacokinetics and half-lives of the therapeutic agents might differ between animals and human eyes. Therefore, further clinical trials in humans with long-term follow-up and inclusion of comparative controls are required.
Disclosure
The authors report no conflicts of interest in this work.
References
- BurrJAzuara-BlancoAAvenellAMedical versus surgical interventions for open angle glaucomaCochrane Database Syst Rev20052CD00439915846712
- HitchingsRInitial treatment for open-angle glaucoma – medical, laser, or surgical? Surgery is the treatment of choice for open-angle glaucomaArch Ophthalmol199811622412429488281
- AddicksEMQuigleyHAGreenWRRobinALHistologic characteristics of filtering blebs in glaucomatous eyesArch Ophthalmol198310157957986847472
- LamaPJFechtnerRDAntifibrotics and wound healing in glaucoma surgerySurv Ophthalmol200348331434612745005
- GeorgoulasSDahlmann-NoorABrocchiniSKhawPTModulation of wound healing during and after glaucoma surgeryProg Brain Res200817323725418929113
- SkutaGLParrishRK2ndWound healing in glaucoma filtering surgerySurv Ophthalmol19873231491703328315
- MillerMHJosephNHEnnisKWGriersonIHitchingsRAAn animal model of filtration surgeryTrans Ophthalmol Soc U K1985104Pt 88938973868883
- SchultzGCheginiNGrantMKhawPMacKaySEffects of growth factors on corneal wound healingActa Ophthalmol Suppl199220260661322013
- WongJWangNMillerJWSchumanJSModulation of human fibroblast activity by selected angiogenesis inhibitorsExp Eye Res19945844394517523160
- TripathiRCParapuramSKTripathiBJZhongYChalamKVCorticosteroids and glaucoma riskDrugs Aging199915643945010641955
- ClarkAFWordingerRJThe role of steroids in outflow resistanceExp Eye Res200988475275918977348
- JohnsonDHMatsumotoYSchlemm’s canal becomes smaller after successful filtration surgeryArch Ophthalmol200011891251125610980771
- Lutjen-DrecollEBaranyEHFunctional and electron microscopic changes in the trabecular meshwork remaining after trabeculectomy in cynomolgus monkeysInvest Ophthalmol19741375115244209932
- ThomasRJayJLRaised intraocular pressure with topical steroids after trabeculectomyGraefes Arch Clin Exp Ophthalmol198822643373403169586
- AraujoSVSpaethGLRothSMStaritaRJA ten-year follow-up on a prospective, randomized trial of postoperative corticosteroids after trabeculectomyOphthalmology199510212175317599098274
- MueckeJBrianGSteroid-induced ocular hypertension in the presence of a functioning Molteno setonAust N Z J Ophthalmol199523167687619460
- ChangMRChengQLeeDABasic science and clinical aspects of wound healing in glaucoma filtering surgeryJ Ocul Pharmacol Ther199814175959493785
- SkutaGLBeesonCCHigginbothamEJIntraoperative mitomycin versus postoperative 5-fluorouracil in high-risk glaucoma filtering surgeryOphthalmology19929934384441565457
- KhawPTSherwoodMBMacKaySLRossiMJSchultzGFive- minute treatments with fluorouracil, floxuridine, and mitomycin have long-term effects on human Tenon’s capsule fibroblastsArch Ophthalmol19921108115011541386726
- GresselMGParrishRK2ndFolbergR5-fluorouracil and glaucoma filtering surgery: I. An animal modelOphthalmology19849143783836717922
- ShapiroMSThoftRAFriendJParrishRKGresselMG5- Fluorouracil toxicity to the ocular surface epitheliumInvest Ophthalmol Vis Sci19852645805833980172
- SmithSD’AmorePADreyerEBComparative toxicity of mitomycin C and 5-fluorouracil in vitroAm J Ophthalmol199411833323378085590
- MegevandGSSalmonJFScholtzRPMurrayADThe effect of reducing the exposure time of mitomycin C in glaucoma filtering surgeryOphthalmology1995102184907831047
- SchnyderCCBernasconiOMermoudAFaggioniR2,5 oder 5minütige Applikation von Mitomycin C bei fistulisierenden Operationen? Eine Vergleichstudie [Comparative study of administration time of mitomycin C in trabeculectomy: 2.5 or 5 minutes?]Klin Monbl Augenheilkd19952065307311 German7609372
- ThorntonIXuMKruegerRRComparison of standard (0.02%) and low dose (0.002%) mitomycin C in the prevention of corneal haze following surface ablation for myopiaJ Refract Surg2008241S68S7618269154
- MatlachJPanidouEGrehnFKlinkTLarge-area versus small-area application of mitomycin C during trabeculectomyEur J Ophthalmol201323567067723640510
- OnolMAktasZHasanreisogluBEnhancement of the success rate in trabeculectomy: large-area mitomycin-C applicationClin Experiment Ophthalmol200836431632218700917
- KhawPTChangLWongTTMeadADanielsJTCordeiroMFModulation of wound healing after glaucoma surgeryCurr Opin Ophthalmol200112214314811224722
- CordeiroMFConstablePHAlexanderRABhattacharyaSSKhawPTEffect of varying the mitomycin-C treatment area in glaucoma filtration surgery in the rabbitInvest Ophthalmol Vis Sci1997388163916469224294
- KhawPTDoyleJWSherwoodMBGriersonISchultzGMcGorraySProlonged localized tissue effects from 5-minute exposures to fluorouracil and mitomycin CArch Ophthalmol199311122632678431167
- KhawPTSherwoodMBDoyleJWIntraoperative and post-operative treatment with 5-fluorouracil and mitomycin-C: long term effects in vivo on subconjunctival and scleral fibroblastsInt Ophthalmol1992164–53813851428576
- SeongGJParkCKimCYMitomycin-C induces the apoptosis of human Tenon’s capsule fibroblast by activation of c-Jun N-terminal kinase 1 and caspase-3 proteaseInvest Ophthalmol Vis Sci200546103545355216186332
- SoltauJBRothmanRFBudenzDLRisk factors for glaucoma filtering bleb infectionsArch Ophthalmol2000118333834210721955
- SistoDVetrugnoMTrabuccoTCantatoreFRuggeriGSborgiaCThe role of antimetabolites in filtration surgery for neovascular glaucoma: intermediate-term follow-upActa Ophthalmol Scand200785326727117488455
- GreenfieldDSLiebmannJMJeeJRitchRLate-onset bleb leaks after glaucoma filtering surgeryArch Ophthalmol199811644434479565040
- HigginbothamEJStevensRKMuschDCBleb-related endophthalmitis after trabeculectomy with mitomycin COphthalmology199610346506568618766
- KaralekasDHARosenbergLRudermanJKrupinTEffects of human glaucomatous and non-glaucomatous aqueous humor on fibroblast proliferation in vitroInvest Ophthalmol Vis Sci19943541898
- TripathiRCLiJChanWFTripathiBJAqueous humor in glaucomatous eyes contains an increased level of TGF-beta 2Exp Eye Res19945967237277698265
- CordeiroMFBhattacharyaSSSchultzGSKhawPTTGF-beta1, -beta2, and -beta3 in vitro: biphasic effects on Tenon’s fibroblast contraction, proliferation, and migrationInvest Ophthalmol Vis Sci200041375676310711691
- CordeiroMFGayJAKhawPTHuman anti-transforming growth factor-beta2 antibody: a new glaucoma anti-scarring agentInvest Ophthalmol Vis Sci199940102225223410476787
- KhawPGrehnFHolloGA phase III study of subconjunctival human anti-transforming growth factor beta(2) monoclonal antibody (CAT-152) to prevent scarring after first-time trabeculectomyOphthalmology2007114101822183017908591
- GrisantiSSzurmanPWargaMDecorin modulates wound healing in experimental glaucoma filtration surgery: a pilot studyInvest Ophthalmol Vis Sci200546119119615623773
- MietzHKrieglsteinGKSuramin to enhance glaucoma filtering procedures: a clinical comparison with mitomycinOphthalmic Surg Lasers200132535836911563779
- MietzHChevez-BarriosPFeldmanRMLiebermanMWSuramin inhibits wound healing following filtering procedures for glaucomaBr J Ophthalmol19988278168209924379
- SpitzerMSSatMSchrammCBiocompatibility and antifibrotic effect of UV-cross-linked hyaluronate as a release-system for tranilast after trabeculectomy in a rabbit model – a pilot studyCurr Eye Res201237646347022577763
- OshimaTKurosakaDKatoKTranilast inhibits cell proliferation and collagen synthesis by rabbit corneal and Tenon’s capsule fibroblastsCurr Eye Res200020428328610806442
- ChiharaEDongJOchiaiHHamadaSEffects of tranilast on filtering blebs: a pilot studyJ Glaucoma200211212713311912360
- Meyer-Ter-VehnTKatzenbergerBHanHGrehnFSchlunckGLovastatin inhibits TGF-beta-induced myofibroblast transdifferentiation in human Tenon fibroblastsInvest Ophthalmol Vis Sci20084993955396018421080
- XiaoYQLiuKShenJFXuGTYeWSB-431542 inhibition of scar formation after filtration surgery and its potential mechanismInvest Ophthalmol Vis Sci20095041698170619098325
- SapitroJDunmireJJScottSESuppression of transforming growth factor-beta effects in rabbit subconjunctival fibroblasts by activin receptor-like kinase 5 inhibitorMol Vis2010161880189221031133
- LiNCuiJDuanXChenHFanFSuppression of type I collagen expression by miR-29b via PI3K, Akt, and Sp1 pathway in human Tenon’s fibroblastsInvest Ophthalmol Vis Sci20125331670167822297492
- BaoPKodraATomic-CanicMGolinkoMSEhrlichHPBremHThe role of vascular endothelial growth factor in wound healingJ Surg Res2009153234735819027922
- LiZVan BergenTVan de VeireSInhibition of vascular endothelial growth factor reduces scar formation after glaucoma filtration surgeryInvest Ophthalmol Vis Sci200950115217522519474408
- HuDNRitchRLiebmannJLiuYChengBHuMSVascular endothelial growth factor is increased in aqueous humor of glaucomatous eyesJ Glaucoma200211540641012362079
- TripathiRCLiJTripathiBJChalamKVAdamisAPIncreased level of vascular endothelial growth factor in aqueous humor of patients with neovascular glaucomaOphthalmology199810522322379479280
- BeddyDWatsonRWFitzpatrickJMO’ConnellPRIncreased vascular endothelial growth factor production in fibroblasts isolated from strictures in patients with Crohn’s diseaseBr J Surg2004911727714716797
- NissenNNPolveriniPJKochAEVolinMVGamelliRLDiPietroLAVascular endothelial growth factor mediates angiogenic activity during the proliferative phase of wound healingAm J Pathol19981526144514529626049
- WilgusTAFerreiraAMOberyszynTMBergdallVKDipietroLARegulation of scar formation by vascular endothelial growth factorLab Invest200888657959018427552
- MemarzadehFVarmaRLinLTPostoperative use of bevacizumab as an antifibrotic agent in glaucoma filtration surgery in the rabbitInvest Ophthalmol Vis Sci20095073233323719182254
- HowAChuaJLCharltonACombined treatment with bevacizumab and 5-fluorouracil attenuates the postoperative scarring response after experimental glaucoma filtration surgeryInvest Ophthalmol Vis Sci201051292893219797222
- Van BergenTVandewalleEVan de VeireSThe role of different VEGF isoforms in scar formation after glaucoma filtration surgeryExp Eye Res201193568969921907194
- KahookMYSchumanJSNoeckerRJNeedle bleb revision of encapsulated filtering bleb with bevacizumabOphthalmic Surg Lasers Imaging200637214815016583638
- CooteMARuddleJBQinQCrowstonJGVascular changes after intra-bleb injection of bevacizumabJ Glaucoma200817751751818854726
- ZarnowskiTTulidowicz-BielakMTopical bevacizumab is efficacious in the early bleb failure after trabeculectomyActa Ophthalmol2011897e605e60619925517
- BiteliLGPrataTSSubconjunctival bevacizumab as an adjuvant in first-time filtration surgery for patients with primary glaucomasInt Ophthalmol201333674174623389840
- Klos-RolaJTulidowicz-BielakMZarnowskiTEffects of topical bevacizumab application on early bleb failure after trabeculectomy: observational case seriesClin Ophthalmol201371929193524109173
- AkkanJUCilsimSRole of subconjunctival bevacizumab as an adjuvant to primary trabeculectomy: a prospective randomized comparative 1-year follow-up studyJ Glaucoma582013 Epub ahead of print
- GrewalDSJainRKumarHGrewalSPEvaluation of subconjunctival bevacizumab as an adjunct to trabeculectomy a pilot studyOphthalmology20081151221412145.e214218692246
- NilforushanNYadgariMKishSKNassiriNSubconjunctival bevacizumab versus mitomycin C adjunctive to trabeculectomyAm J Ophthalmol20121532352357.e35121982106
- SenguptaSVenkateshRRavindranRDSafety and efficacy of using off-label bevacizumab versus mitomycin C to prevent bleb failure in a single-site phacotrabeculectomy by a randomized controlled clinical trialJ Glaucoma201221745045921543993
- SedghipourMRMostafaeiATaghaviYLow-dose subconjunctival bevacizumab to augment trabeculectomy for glaucomaClin Ophthalmol2011579780021750613
- ChuaBENguyenDQQinQBleb vascularity following post-trabeculectomy subconjunctival bevacizumab: a pilot studyClin Experiment Ophthalmol201240877377922429268
- Jurkowska-DudzinskaJKosior-JareckaEZarnowskiTComparison of the use of 5-fluorouracil and bevacizumab in primary trabeculectomy: results at 1 yearClin Experiment Ophthalmol2012404e135e14221668792
- SuhWKeeCThe effect of bevacizumab on the outcome of trabeculectomy with 5-fluorouracilJ Ocul Pharmacol Ther201329764665123621628
- VandewalleEAbegao PintoLVan BergenTIntracameral bevacizumab as an adjunct to trabeculectomy: a 1-year prospective, randomised studyBr J Ophthalmol2014981737824158846
- Van BergenTJonckxBHollandersKInhibition of placental growth factor improves surgical outcome of glaucoma surgeryJ Cell Mol Med201317121632164324118824
- InoueTKawajiTInataniMKamedaTYoshimuraNTaniharaHSimultaneous increases in multiple proinflammatory cytokines in the aqueous humor in pseudophakic glaucomatous eyesJ Cataract Refract Surg20123881389139722814044
- TakaiYTanitoMOhiraAMultiplex cytokine analysis of aqueous humor in eyes with primary open-angle glaucoma, exfoliation glaucoma, and cataractInvest Ophthalmol Vis Sci201253124124722159018
- KuchteyJRezaeiKAJaru-AmpornpanPSternbergPJrKuchteyRWMultiplex cytokine analysis reveals elevated concentration of interleukin-8 in glaucomatous aqueous humorInvest Ophthalmol Vis Sci201051126441644720592224
- Schlotzer-SchrehardtULommatzschJKuchleMKonstasAGNaumannGOMatrix metalloproteinases and their inhibitors in aqueous humor of patients with pseudoexfoliation syndrome/glaucoma and primary open-angle glaucomaInvest Ophthalmol Vis Sci20034431117112512601038
- KnorrMVolkerMDenkPOWunderlichKThielHJProliferative response of cultured human Tenon’s capsule fibroblasts to platelet-derived growth factor isoformsGraefes Arch Clin Exp Ophthalmol1997235106676719349953
- CunliffeIARichardsonPSReesRCRennieIGEffect of TNF, IL-1, and IL-6 on the proliferation of human Tenon’s capsule fibroblasts in tissue cultureBr J Ophthalmol19957965905957626577
- Salas-PratoMAssalianAMehdiAZDuperreJThompsonPBrazeauPInhibition by rapamycin of PDGF- and bFGF-induced human tenon fibroblast proliferation in vitroJ Glaucoma19965154598795734
- WongTTMeadALKhawPTMatrix metalloproteinase inhibition modulates postoperative scarring after experimental glaucoma filtration surgeryInvest Ophthalmol Vis Sci20034431097110312601035
- Martin-MartinBTovellVDahlmann-NoorAHKhawPTBaillyMThe effect of MMP inhibitor GM6001 on early fibroblast-mediated collagen matrix contraction is correlated to a decrease in cell protrusive activityEur J Cell Biol2011901263621040999
- Rodriguez-AgirretxeIGarciaISoriaJAceraASuarez-CortesTMPrognosis of glaucoma surgery failure by customized gene expression PCR-arrayInvest Ophthalmol Vis Sci201253 ARVO E-Abstract 2514
- LiaoJKSetoMNomaKRho kinase (ROCK) inhibitorsJ Cardiovasc Pharmacol2007501172417666911
- DoeCBentleyRBehmDJNovel Rho kinase inhibitors with anti-inflammatory and vasodilatory activitiesJ Pharmacol Exp Ther20073201899817018693
- HeYXuHLiangLAntiinflammatory effect of Rho kinase blockade via inhibition of NF-kappaB activation in rheumatoid arthritisArthritis Rheum200858113366337618975348
- OkamotoHYoshioTKanekoHYamanakaHInhibition of NF-kappaB signaling by fasudil as a potential therapeutic strategy for rheumatoid arthritisArthritis Rheum2010621829220039418
- ZhaoLXuGZhouJThe effect of RhoA on human umbilical vein endothelial cell migration and angiogenesis in vitroOncol Rep20061551147115216596177
- van Nieuw AmerongenGPKoolwijkPVersteilenAvan HinsberghVWInvolvement of RhoA/Rho kinase signaling in VEGF-induced endothelial cell migration and angiogenesis in vitroArterioscler Thromb Vasc Biol200323221121712588761
- HonjoMTaniharaHKamedaTKawajiTYoshimuraNAraieMPotential role of Rho-associated protein kinase inhibitor Y-27632 in glaucoma filtration surgeryInvest Ophthalmol Vis Sci200748125549555718055804
- Meyer-ter-VehnTSieprathSKatzenbergerBGebhardtSGrehnFSchlunckGContractility as a prerequisite for TGF-beta-induced myofibroblast transdifferentiation in human Tenon fibroblastsInvest Ophthalmol Vis Sci200647114895490417065504
- NomotoHShiragaFKunoNPharmacokinetics of bevacizumab after topical, subconjunctival, and intravitreal administration in rabbitsInvest Ophthalmol Vis Sci200950104807481319324856
- AmbatiJGragoudasESMillerJWTransscleral delivery of bioactive protein to the choroid and retinaInvest Ophthalmol Vis Sci20004151186119110752959
- OzgonulCMumcuogluTGunalAThe effect of bevacizumab on wound healing modulation in an experimental trabeculectomy modelCurr Eye Res11112013 Epub ahead of print
- AnandNBongCDeep sclerectomy with bevacizumab and mitomycin C: a comparative studyJ Glaucoma2192013 Epub ahead of print
- KahookMYBleb morphology and vascularity after trabeculectomy with intravitreal ranibizumab: a pilot studyAm J Ophthalmol20101503399403.e39120570237
- FreibergFJMatlachJGrehnFKarlSKlinkTPostoperative subconjunctival bevacizumab injection as an adjunct to 5-fluorouracil in the management of scarring after trabeculectomyClin Ophthalmol201371211121723814458
- ChenHYGeJGuoYJinCJLanYQLinMK[The inhibition effect of photodynamic on human Tenon capsule fibroblast cells]Zhonghua Yan Ke Za Zhi2003393160162 Chinese12880573
- JordanJFDiestelhorstMGrisantiSKrieglsteinGKPhotodynamic modulation of wound healing in glaucoma filtration surgeryBr J Ophthalmol200387787087512812889
- DiestelhorstMGrisantiSPhotodynamic therapy to control fibrosis in human glaucomatous eyes after trabeculectomy: a clinical pilot studyArch Ophthalmol2002120213013411831913
- SaeedAMComparative study between trabeculectomy with photodynamic therapy (BCECF-AM) and trabeculectomy with antimetabolite (MMC) in the treatment of primary open angle glaucomaClin Ophthalmol201261651166423109802
- MinJLukowskiZLLevineMAPrevention of ocular scarring post glaucoma filtration surgery using the inflammatory cell and platelet binding modulator saratin in a rabbit modelPLoS One201274e3562722558182
- MinJLukowskiZLLevineMAComparison of single versus multiple injections of the protein saratin for prolonging bleb survival in a rabbit modelInvest Ophthalmol Vis Sci201253127625763023033390
- LukowskiZLMinJBeattieARPrevention of ocular scarring after glaucoma filtering surgery using the monoclonal antibody LT1009 (sonepcizumab) in a rabbit modelJ Glaucoma201322214515121946553
- SenEBalikoglu-YilmazMBozdag-PehlivanSEffect of doxycycline on postoperative scarring after trabeculectomy in an experimental rabbit modelJ Ocul Pharmacol Ther201026539940620874665
- LinXYuMWuKYuanHZhongHEffects of pirfenidone on proliferation, migration, and collagen contraction of human Tenon’s fibroblasts in vitroInvest Ophthalmol Vis Sci20095083763377019264889
- ZhongHSunGLinXWuKYuMEvaluation of pirfenidone as a new postoperative antiscarring agent in experimental glaucoma surgeryInvest Ophthalmol Vis Sci20115263136314221330661
- ArslanSAydemirOGulerMDagliAFModulation of postoperative scarring with tacrolimus and octreotide in experimental glaucoma filtration surgeryCurr Eye Res201237322823322335810
- JacobJTLacourOJBurgoyneCFSlow release of the antimetabolite 5-fluorouracil (5-FU) from modified Baerveldt glaucoma drains to prolong drain functionBiomaterials200122243329333511700805
- PolakMBValamaneshFFeltOControlled delivery of 5-chlorouracil using poly (ortho esters) in filtering surgery for glaucomaInvest Ophthalmol Vis Sci20084972993300318579761
- LiWChenWJLiuWLiangLZhangMCHomemade lyophilized cross linking amniotic sustained-release drug membrane with anti-scarring role after filtering surgery in rabbit eyesInt J Ophthalmol20125555556123166864
- SooHooJRSeiboldLKLaingAEKahookMYBleb morphology and histology in a rabbit model of glaucoma filtration surgery using Ozurdex®) or mitomycin-CMol Vis20121871471922509101
- KhaliliARayapureddiSPaulDJA novel slow release solid bevacizumab tissue tablet prevents scarring following experimental glaucoma filtration surgery (GFS)Abstract 1645 presented at the Research in Vision and Ophthalmology Annual MeetingMay 1–5, 2011Fort Lauderdale, FL, USA
