Abstract
Purpose
To evaluate management strategies and outcomes for patients with giant retinal tear (GRT)-associated retinal detachment (RD) that had undergone previous pars plana vitrectomy (PPV).
Methods
A noncomparative consecutive case series between January 2005 and July 2010. Patients with a preceding history of PPV undergoing retinal reattachment surgery for GRTs were identified.
Results
Using International Classification of Diseases 9 codes for GRTs, 227 cases were identified. A total of eight eyes in eight patients were identified as having had preceding PPV for non-RD-related pathology. The mean age was 45.5 (range of 10–79) years. The mean time between PPV and diagnosis of GRT was 2.4 months. The mean follow-up after RD surgery was 24.3 months. Presenting visual acuity was 20/400 or better in four of eight patients (50%). All patients underwent repeat PPV with either gas or oil tamponade. A scleral buckling procedure was performed in seven patients (88%). Perfluorocarbon liquid was used during reattachment surgery in four patients (50%). Although anatomic success was achieved in all patients, visual acuity at last follow-up was 20/400 or better in 6 patients (75%).
Conclusion
GRTs are an uncommon complication of PPV. The majority of patients underwent repeat PPV, scleral buckling procedure, perfluorocarbon liquid use and silicone-oil tamponade. Patients presenting with GRT-associated RD after PPV undergoing additional surgery achieved high rates of anatomic success, but visual outcomes were variable.
Introduction
A giant retinal tear (GRT) is classically defined as a full-thickness break in the neurosensory retina that extends ≥3 hours circumferentially.Citation1 The true incidence of GRTs is difficult to assess given their rarity, but one recent study estimates 0.094 per 100,000 of the general population per year.Citation2 The majority of GRTs are thought to be idiopathic, but identifiable associations include hereditary vitreoretinopathies, trauma, complications of cataract surgery, cryotherapy, and photocoagulation.Citation1,Citation3–Citation5
Intraocular surgery is a known risk factor for retinal tears and retinal detachment (RD).Citation6–Citation8 The rate of RD after pars plana vitrectomy (PPV) varies widely in the literature, ranging from 1.1% to 17.4%, and may depend on the size of sclerotomy, indications for initial PPV, and patient comorbidities.Citation9–Citation13 The current study represents a noncomparative case series of patients with a history of previous PPV for non-RD-related indications that developed a GRT-associated RD at a university referral center. The etiologies, surgical techniques, and outcomes are reported in these selected GRTs.
Methods
The institutional review board at the University of Miami approved the study protocol. The study population consisted of patients who had undergone primary RD repair with PPV at the Bascom Palmer Eye Institute between January 2005 and July 2010. Patients were included if they had undergone prior PPV and had more than 1 month of follow-up. A GRT was defined as a retinal tear of 90° or greater confirmed by clinical examination or intraoperatively.
Patients were initially identified through the use of the International Classification of Diseases (ICD)-9 code for GRT (361.03). A total of 227 patients were listed through the use of ICD-9 codes. Subsequent chart review yielded eight eyes that met the study inclusion criteria, including a history of prior PPV. Data were collected regarding demographic information, recorded etiologies, and surgical techniques.
Outcome variables included visual acuity (VA), rates of retinal reattachment, rates of reoperation, and rates of complications. Outcome variable data were collected at postoperative week 1, month 1, month 3, month 6, 1 year, and last follow-up date. Best-corrected visual acuity and intraocular pressure were recorded during all follow-up examinations. The operating surgeon selected the surgical approach for the individual patient, and there was no defined protocol in this study.
Results
Demographic and baseline characteristics are summarized in . The study included eight eyes of eight patients followed for a mean of 24.3 months (see ). Preceding PPV was undertaken for a pars plana lensectomy in three cases, nonclearing vitreous hemorrhage in three cases, intraocular lens repositioning in one case, and endophthalmitis in one case. All preceding PPVs that were undertaken were 20-gauge, and only two cases had had a previous anterior vitrectomy. The mean time between PPV and diagnosis of GRT was 2.4 months. Prior to initial RD repair, proliferative vitreoretinopathy was described in two cases (25%). None of the study eyes had a history of high myopia, and only one eye had preceding blunt trauma recorded in the medical record. None of the patients had a history of RD in the fellow eye.
Figure 1 Fundus photo of a 52-year-old man with a history of proliferative diabetic retinopathy status-postpan-retinal photocoagulation who had initially undergone pars plana vitrectomy for nonclearing vitreous hemorrhage and subsequently developed a superior giant retinal tear macula-sparing retinal detachment (A). He underwent pars plana vitrectomy/endolaser/fluid–air exchange/silicone-oil infusion. His retina remains attached 4 years postremoval of silicone oil with a best-corrected visual acuity of 20/200 (B).
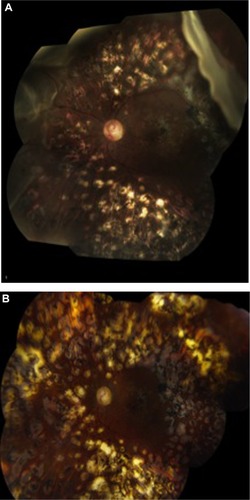
Table 1 Baseline characteristics of patients with previous pars plana vitrectomy undergoing surgery for giant retinal tear-related retinal detachment
On initial presentation with GRT, two eyes (25%) were phakic, and six eyes were pseudophakic (75%). Four eyes (50%) had macular involvement at the time of GRT diagnosis. Initial visual acuity was ≥20/400 in four eyes (50%) and <20/400 in four eyes (50%). Intraoperative data are summarized in and . The GRT was 90° in five eyes (63%), greater than 90° but less than 180° in two eyes (25%), and greater than or equal to 180° in one eye (13%). GRT location was superotemporal in three cases, temporal in two cases, inferonasal in one case, and superonasal in one case.
Figure 2 Initial management for patients with previous pars plana vitrectomy (PPV) undergoing surgery for giant retinal tear-associated retinal detachments.
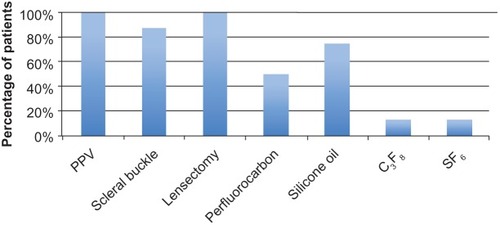
Table 2 Intraoperative data for patients with previous pars plana vitrectomy undergoing surgery for giant retinal tear-related retinal detachments
All eight eyes underwent repeat PPV as part of the retinal reattachment surgery. An encircling scleral buckle was utilized in seven eyes (88%), and perfluorocarbon liquid was used in four eyes (50%). A lensectomy was performed in all phakic eyes. Internal tamponade was achieved with silicone oil in six eyes (75%), SF6 in one eye (13%) and C3F8 in one eye (13%). None of the eyes required additional surgery for recurrent RD. Four of the six eyes (67%) that underwent silicone-oil tamponade on initial surgery underwent a second operation for silicone-oil removal by last follow-up visit. All eyes were reattached at last follow-up visit.
Postoperative visual outcomes are summarized in . VA at last follow-up visit was ≥20/40 in two eyes (25%), ≥20/400 in six eyes (75%), and <20/400 in two eyes (25%). All eyes demonstrated improvement or stability in VA at the last follow-up examination when compared to initial presentation.
Table 3 Anatomic and visual acuity outcomes of patients undergoing surgery for giant retinal tear-related retinal detachments
Discussion
The reported development of new-onset RD after intraocular surgery varies according to the surgical procedure. The rate of RD is higher in procedures in which there is significant manipulation of the vitreous cavity compared to those in which the posterior segment is not manipulated. Complicated cataract surgery with vitreous loss may have an incidence of RD as high as 6.2%–8.2% compared to uncomplicated cataract surgery, in which the estimated incidence of RD may be as low as 0.7%.Citation14 Few studies have reported on rates of new-onset RD after PPV, but recent published data seem to report the incidence to be less than 2% in sutureless PPV.Citation10 During PPV, proposed mechanisms for iatrogenic breaks are sudden mechanical traction of the vitreous base during surgical manipulation, postoperative peripheral vitreous contracture, and incarceration of vitreous into sclerotomy sites.Citation9,Citation12,Citation13,Citation15
The development of a GRT following PPV appears to be less common. Iatrogenic GRTs have been reported in small case studies after cataract surgery, phakic intraocular lens insertion, and PPV for retained lens fragments.Citation16–Citation18 In the current study, the rate of GRTs after PPV appears to be low, with only eight total cases identified over a 5-year period.
Prior studies have established risk factors for the development of GRTs, including high myopia, hereditary vitreoretinopathy, and prior trauma.Citation1,Citation4,Citation5 In the current study, none of the eyes had a history of high myopia, and only one eye had a history of prior trauma. The superiorly skewed distribution for the majority of the GRTs (87% of cases) also supports the presumed iatrogenic etiology for the development of these GRTs. As initially postulated by McLeod, the development of GRT after PPV could be related to vitreous incarceration and secondary traction on the retina in the area of the vitreous base.Citation19 Another possible cause is aggressive vitreous base dissection with or without the use of scleral indentation. When shaving the vitreous base, iatrogenic retinal breaks may occur and could coalesce into a GRT.
GRT-related RDs are unique with respect to the surgical techniques required, postoperative management, and ultimate visual outcomes.Citation20 They present a unique challenge to the vitreoretinal surgeon, and may have higher rates of proliferative vitreoretinopathy and subsequent development of redetachment.Citation5,Citation21 In the current study, none of the cases required surgery for recurrent RD. The majority of cases underwent silicone-oil tamponade, and it is possible that the persistent presence of oil skewed the long-term anatomic results.
In addition to PPV, the use of encircling scleral buckle has been a point of controversy among vitreoretinal surgeons.Citation20,Citation22 Some studies have identified a lack of encircling scleral buckle to be associated with a higher rate of recurrent RD.Citation22,Citation23 Other studies have reported comparable success rates in the absence of encircling scleral buckle.Citation24 None of these studies reported on cases that had preceding PPV. Primary GRT-associated RDs may initially be managed with PPV and gas tamponade. In the current study, GRT-associated RDs in the setting of a previous vitrectomy were more commonly managed with the addition of an encircling scleral buckle (87%) and long-term internal tamponade with silicone oil.
The use of perfluorocarbon liquids has become increasingly popular as a means to unfold and manipulate a GRT. In the current study, only four of the eight cases had perfluorocarbon-liquid use. Factors involved in the decision to use perfluorocarbon liquid include the extent of the GRT and the ease of manipulation of the retinal flap. In general, longer circumferential extent and more peripheral flaps were associated with the use of perfluorocarbon liquid. By contrast, quadrantic GRTs and more posterior flaps were associated with nonuse of perfluorocarbon liquid.
Lensectomy is often performed to enable better visualization of the peripheral retina and to accomplish more effective shaving of the anterior peripheral vitreous. Some authors have advocated lensectomy in patients with larger GRTs and with the presence of proliferative vitreoretinopathy. In the current study, all phakic patients underwent pars plana lensectomy with initial reattachment surgery. This is most likely a selection bias, as most patients would have likely had previously induced cataractous changes secondary to their initial PPV.
In conclusion, GRT-related RD is an uncommon complication after PPV. In the current study, the majority of cases underwent repeat PPV, an encircling scleral buckle procedure, and silicone-oil tamponade. Perfluorocarbon-liquid use varied according to circumferential extent of the GRT and surgeon preference. Most patients achieved a VA of ≥20/400 (75%) and anatomic success (100%) after initial surgery.
Acknowledgments
This study was supported in part by an NIH Center Core Grant P30EY014801 and a Research to Prevent Blindness Unrestricted Grant, Department of Defense (DOD-Grant#W81XWH-09-1-0675).
Disclosure
Harry W Flynn Jr, Vindico (Speaker), Santeen (Consultant); Thomas A Albini, Allergan (Consultant), Bausch and Lomb (Consultant), Eleven Biotherapeutics (Consultant), ThromboGenics (Consultant), Genentech (Grant); Audina M Berrocal, ThromboGenics (Consultant), Genentech (Consultant). MA Gonzalez, WE Smiddy and P Tenzel report no conflicts of interest in this work.
References
- SchepensCLDobbleJGMcMeelJWRetinal detachments with giant breaks: preliminary reportTrans Am Acad Ophthalmol Otolaryngol19626647147914498242
- AngGSTownendJLoisNEpidemiology of giant retinal tears in the United Kingdom: the British Giant Retinal Tear Epidemiology Eye Study (BGEES)Invest Ophthalmol Vis Sci20105194781478720393105
- AabergTMJrRubsamenPEFlynnHWJrChangSMielerWFSmiddyWEGiant retinal tear as a complication of attempted removal of intravitreal lens fragments during cataract surgeryAm J Ophthalmol199712422222269262547
- KarelIDolezalováJOudováPStickler’s syndrome (dystrophia vitreoretinalis hereditaria). Results of surgery for retinal detachmentCesk Slov Oftalmol2001573147154 Czech11433587
- AylwardGWCoolingRJLeaverPKTrauma-induced retinal detachment associated with giant retinal tearsRetina19931321361418337495
- LoisNWongDPseudophakic retinal detachmentSurv Ophthalmol200348546748714499816
- ErieJCRaeckerMABaratzKHSchleckCDBurkeJPRobertsonDMRisk of retinal detachment after cataract extraction, 1980–2004: a population-based studyOphthalmology2006113112026203216935341
- KraffMCSandersDRIncidence of retinal detachment following posterior chamber intraocular lens surgeryJ Cataract Refract Surg19901644774802380929
- RizzoSBeltingCGenovesi-EbertFRetinal detachment after small-incision, sutureless pars plana vitrectomy: possible causative agentsGraefes Arch Clin Exp Ophthalmol2010248101401140620473765
- ChaDMWooSJParkKHChungHIntraoperative iatrogenic peripheral retinal break in 23-gauge transconjunctival sutureless vitrectomy versus 20-gauge conventional vitrectomyGraefes Arch Clin Exp Ophthalmol201325161469147423504087
- ParkSSMarcusDMDukerJSPosterior segment complications after vitrectomy for macular holeOphthalmology199510257757817777277
- GuillaubeyAMalvitteLLafontainePOIncidence of retinal detachment after macular surgery: a retrospective study of 634 casesBr J Ophthalmol200791101327133017522152
- TabandehHChaudhryNASmiddyWERetinal detachment associated with macular hole surgery: characteristics, mechanism, and outcomesRetina199919428128610458291
- HaugSJBhisitkulRBRisk factors for retinal detachment following cataract surgeryCurr Opin Ophthalmol201223171122081033
- SjaardaRNGlaserBMThompsonJTMurphyRPHanhamADistribution of iatrogenic retinal breaks in macular hole surgeryOphthalmology19951029138713929097778
- AtulKSubijaySJaideepTVarunGEarly onset giant retinal tear after posterior chamber phakic IOLActa Ophthalmologica2011896e537e53820698829
- GeorgalasIPetrouPPapaconstantinouDKoutsandreaCLadasIBilateral giant tear-associated retinal detachment following Artisan phakic intraocular lens implantation for correction of moderate myopiaActa Ophthalmologica2009884e143e14419549101
- MooreJKScottIUFlynnHWRetinal detachment in eyes undergoing pars plana vitrectomy for removal of retained lens fragmentsOphthalmology20031104709713 discussion 713–71412689890
- McLeodDGiant retinal tears after central vitrectomyBr J Ophthalmol198569296983967003
- GonzalezMAFlynnHWJrSmiddyWEAlbiniTATenzelPSurgery for retinal detachment in patients with giant retinal tear: etiologies, management strategies, and outcomesOphthalmic Surg Lasers Imaging Retina201344323223723676223
- Al-KhairiAMAl-KahtaniEKangaveDAbu El-AsrarAMPrognostic factors associated with outcomes after giant retinal tear management using perfluorocarbon liquidsEur J Ophthalmol200818227027718320521
- LeaverPKBillingtonBMVitrectomy and fluid/silicone-oil exchange for giant retinal tears: 5 years follow-upGraefes Arch Clin Exp Ophthalmol198922743233272777101
- GoezinneFLA HeijECBerendschotTTLow redetachment rate due to encircling scleral buckle in giant retinal tears treated with vitrectomy and silicone oilRetina200828348549218327143
- KreigerAELewisHManagement of giant retinal tears without scleral buckling. Use of radical dissection of the vitreous base and perfluoro-octane and intraocular tamponadeOphthalmology19929944914971584565