Abstract
Purpose
We report the successful treatment of a case of cystoid macular edema (CME) associated with topical tafluprost, which was accompanied by serous retinal detachment (SRD).
Case
A 78-year-old woman underwent intraocular lens suture surgery, including anterior vitreous cutting, for crystalline lens dislocation in the right eye. Tafluprost was initiated 12 weeks after surgery. Intraocular pressure (IOP) was controlled at 10–14 mmHg. Visual acuity remained at 20/40–30/40. However, the patient complained of blurred vision (20/200) 9 months after surgery. CME accompanied by SRD was identified by optical coherence tomography (OCT) and treated with subtenon triamcinolone injection. Visual acuity rapidly increased to 20/50, and the volume of SRD decreased in a few days. Discontinuation of tafluprost and initiation of diclofenac eye drops improved visual acuity to 20/40 and resulted in improved OCT findings within a few weeks. Three months after injection, tafluprost was resumed along with diclofenac. No recurrence of CME occurred over the following 3 months, and IOP was controlled at 10–15 mmHg.
Conclusion
SRD is considered to be a symptom of treatment-resistant CME, which may lead to poor visual acuity after recovery. In such cases, subtenon triamcinolone injection should be strongly considered at an early stage.
Introduction
Cystoid macular edema (CME) has been reported in association with the use of latanoprost, travoprost, and bimatoprost.Citation1,Citation2 These drugs are ocular hypotensive lipids, and their side effects can be expected to be somewhat similar. In this report, we describe a case of CME associated with tafluprost. Optical coherence tomography (OCT) revealed typical CME appearance with serous retinal detachment (SRD). The patient was successfully treated with subtenon triamcinolone injection. To our knowledge, this is the first report of CME associated with tafluprost.
Case report
A 78-year-old woman, who had a history of chronic bronchitis, was under observation for glaucoma with use of tafluprost. Intraocular pressure (IOP) was controlled at 13–16 mmHg without any tafluprost side effects.
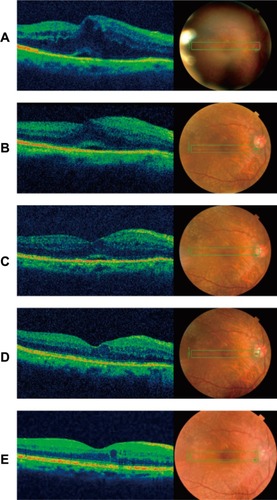
The patient underwent intraocular lens (IOL) suture surgery, including anterior vitreous cutting, for crystalline lens dislocation in the right eye. Tafluprost was resumed 12 weeks after surgery. Intraocular pressure (IOP) was controlled at 10–14 mmHg. Visual acuity remained at 20/40–30/40. However, 9 months after the surgery, the patient complained of blurred vision (20/200), and CME accompanied by SRD was identified with OCT (). After injection of subtenon triamcinolone, visual acuity rapidly recovered to 20/50, and the SRD lost its volume in a few days (). Discontinuation of tafluprost and initiation of diclofenac eye drops improved visual acuity to 20/40 and OCT showed improvements within a few weeks ( and ). An IOP spike after injection of subtenon triamcinolone was observed. Because IOP was above 20 mmHg, we resumed treatment with diclofenac eye drops and tafluprost 3 months after injection, as we considered that the damage to the blood–aqueous barrier would be protracted. No recurrence of CME occurred during the following 3 months, and IOP was controlled at 10–15 mmHg ().
Figure 1 Vertical sections of optical coherence tomography
Abbreviations: CME, cystoid macular edema; SRD, serous retinal detachment.
Discussion
Tafluprost, like other prostaglandin analogs, exerts its effects on prostaglandin F receptors to reduce IOP. Several clinical studies have assessed the efficacy of tafluprost and reported that it was equivalent to the efficacy of latanoprost.Citation3 Furthermore, some recent studies have suggested that tafluprost has direct neuroprotective effects. Mayama et al found that topical tafluprost enhanced optic nerve head blood flow in naïve eyes without significant IOP reduction.Citation4 Side effects of tafluprost, such as deepening of the eyelid sulcus and increased eyelid pigmentation, have been reported to be similar to those of other prostaglandin eye drops.Citation5 The incidence of deepening of the eyelid sulcus has been shown to be lower with tafluprost than with latanoprost, travoprost, or bimatoprost.Citation5 Liang et al indicated that the benzalkonium chloride (BAK) preservative is the primary cause of cytotoxicity due to prostaglandin analogs, given that BAK-free products had minimal impact on the corneoconjunctival surface.Citation6 Uusitalo et al evaluated the pharmacokinetics and safety profiles of preservative-free and preservative-containing tafluprost; although the incidence of ocular hyperemia was similar for both forms of tafluprost, it was less severe with preservative-free tafluprost.Citation7 Prostaglandin analogs have been shown to cause CME after cataract surgery. Miyake et al reported that the preservatives in prostaglandin eye drops have a greater influence on the development of CME than the base compound.Citation8 There are many reports of CME associated with latanoprost,Citation9–Citation19 which contains a relatively high BAK concentration (0.02%), but there are few reports of CME associated with BAK-free travoprost. BAK-free tafluprost became available in Western countries in 2012; the Japanese product contains a very low concentration of BAK (0.001%). To our knowledge, this is the first report of CME associated with tafluprost.
Risk factors for CME due to prostaglandin eye drops include a history of glaucoma surgeries, aphakia, complicated cataract surgery, scleral buckling, and vitrectomy, as well as a history of uveitis and other retinal diseases. It is rare for patients without risk factors to develop CME.Citation9–Citation15 Wand et alCitation12 reported that two of 38 high-risk cases (5.3%) developed clinical CME. Fukuichi et alCitation16 found no cases of clinical CME among 68 patients without any of the reported risk factors. In cases without known risk factors, CME can appear within 2–3 months after surgery,Citation17,Citation18 while in high-risk cases, CME can develop several years after surgery.Citation9,Citation11–Citation13,Citation15,Citation20 In the former, CME may develop immediately after surgery because of temporary damage to the blood–aqueous barrier, while in cases with known risk factors, the damage to the blood– aqueous barrier is protracted, resulting in a continuation of conditions that can lead to CME in the long term. In the case reported here, anterior vitreous cutting and the IOL suture surgery were performed for crystalline lens dislocation; thus, CME accompanied with SRD occurred 9 months after surgery.
As leakage from retinal capillaries increases, traction on the inner and outer segments of the fovea produces a small, pointed retinal detachment with a small base. When the barrier function of external limiting membrane breaks down, the serous RD enlarges and changes into a dome-shaped retinal detachment with a large base.Citation21
Tsujikawa et al reported that the outer retinal discontinuity on the external surface of the retina does not necessarily lead to poor vision.Citation21 However, even after complete resolution of the macular edema and SRD, diffuse disorganization of the outer photoreceptor layer beneath the fovea often results in poor visual acuity. In addition, a dome-shaped retinal detachment sometimes accompanies a focal defect of the outer segment of the photoreceptors above SRD.Citation21
Several treatment options are available for prostaglandin-induced CME, including non-steroidal anti-inflammatory drugs (NSAIDs), steroids, dorzolamide hydrochloride eye drops, and oral acetazolamide; however, in many cases, recovery can take a month or more.Citation11–Citation13,Citation17,Citation19,Citation22 We previously reported two cases in which travoprost- and latanoprost-induced CME was successfully treated in a few days with subtenon injection of triamcinolone.Citation23 Subtenon triamcinolone injection is considered to be effective and is the standard treatment for CME due to diabetic retinopathy, retinal vein occlusion, uveitis, and other conditions. Therefore, in this case, we employed subtenon triamcinolone injection immediately after diagnosis, anticipating a quick recovery from CME and a subsequently minimized irreversible disruption in the sensory retina.
We reported two cases in which CME did not recur for more than 3 years after resumption of prostaglandin eye drops.Citation23 The first case was CME associated with travoprost following uneventful cataract surgery. The second case was CME associated with latanoprost after anterior vitreous cutting and IOL suture. Diclofenac was used after resumption of latanoprost in the second case. Wand and GaudioCitation20 reported two cases in which CME treated with NSAIDs did not recur after unoprostone and bimatoprost treatments were resumed. Furthermore, Wand et al reported one case in which CME did not recur after latanoprost treatment was resumed.Citation12 Callanan et alCitation11 reported one case in which CME that was not treated with NSAIDs recurred after resuming treatment with latanoprost. Prostaglandin has no systemic side effects and is currently the most effective drug in the form of eye drops.
Beta-blockers were not chosen as treatment in this case because of the patient’s history of bronchitis, nor brimonidine, which was not commercially available until May 2012 in Japan. Thus, tafluprost use was resumed postoperatively, considering that the patient had been well-controlled and without tafluprost side effects before surgery. Although we believe the risk of CME would be reduced by using tafluprost along with NSAIDs, the patient was informed of the necessity of careful observation.
When possible, the use of prostaglandin eye drops can be resumed after a certain period of time after recovery, under careful observation. In certain cases, the concomitant use of NSAIDs and prostaglandin eye drops can be greatly beneficial to patients.
Conclusion
We have reported a case of CME associated with tafluprost and accompanied by SRD. SRD was considered to be a symptom of treatment-resistant CME, which can lead to poor visual acuity after recovery. In such cases, subtenon triamcinolone injection should be considered at an early stage.
Disclosure
The authors report no conflicts of interest in this work.
References
- ArcieriESSantanaARochaFNGaupoGLCostaVPBlood-aqueous barrier changes after the use of prostaglandin analogues in patients with pseudophakia and aphakia: a 6-month randomized trialArch Ophthalmol2005123218619215710814
- AgangeNMosaedSProstaglandin-induced cystoid macular edema following routine cataract extractionJ Ophthalmol20102010
- LiuYMaoWTafluprost once daily for treatment of elevated intraocular pressure in patients with open-angle glaucomaClin Ophthalmol2013771423293509
- MayamaCIshiiKSaekiTOtaTTomidokoroAAraieMEffects of topical phenylephrine and tafluprost on optic nerve head circulation in monkeys with unilateral experimental glaucomaInvest Ophthalmol Vis Sci20105184117412420357196
- InoueKShiokawaMWakakuraMTomitaGDeepening of the upper eyelid sulcus caused by 5 types of prostaglandin analogsJ Glaucoma Epub8292012
- LiangHBaudouinCLabbeARianchoLBrignole-BaudouinFConjunctiva-associated lymphoid tissue (CALT) reactions to antiglaucoma prostaglandins with or without BAK-preservative in rabbit acute toxicity studyPLoS One20127e3391322442734
- UusitaloHKaarnirantaKRopoAPharmacokinetics, efficacy, and safety profiles of preserved and preserve-free tafluprost in healthy volunteersActa Ophthalmol Suppl (Oxf)200824271318752509
- MiyakeKOtaIIbarakiNEnhanced disruption of the blood-aqueous barrier and the incidence of angiographic cystoid macular edema by topical timolol and its preservative in early postoperative pseudophakiaArch Ophthalmol2001119338739411231772
- AyyalaRSCruzDAMargoCECystoid macular edema associated with latanoprost in aphakic and pseudophakic eyesAm J Ophthalmol199812646026049780112
- MoroiSEGottfredsdottirMSSchteingartMTCystoid macular edema associated with latanprost therapy in a case of patients with glaucoma and ocular hypertensionOphthalmology199910651024102910328408
- CallananDFellmanRLSavageJALatanoprost-associated cystoid macular edemaAm J Ophthalmol199812611341359683162
- WandMGaudioARShieldsMBLatanoprost and cystoid macular edema in high-risk aphakic or pseudophakic eyesJ Cataract Refract Surg20012791397140111566522
- TokunagaTKashiwagiKSaitoJA case of cystoid macular edema associated with latanoprost ophthalmic solutionJpn J Ophthalmol200246665665912543193
- JägerMJonasJBCytoid macular edema associated with latano-prost therapy in a pseudophakic vitrectomized patient after removal of silicone oil endotamponadeEur J Ophthalmol200313222122212696646
- WatanabeKHayasakaSHayasakaYNagakiYWatanabeKCystoid macular edema associated with latanoprost use in a pseudophakic eye with a history of surgical complicationsJpn J Ophthalmol200347111011212586189
- FukuichiMChibaTAbeKCystoid macular edema associated with topical latanoprost in glaucomatous eyes with a normally functioning blood-ocular barrierJ Glaucoma200110323323611442189
- AltintasOYükselNKarabasVLDermirciGCystoid macular edema associated with latanoprost after uncomplicated cataract surgeryEur J Ophthalmol200515115816115751259
- YehPCRamanathanSLatanoprost and clinically significant cystoid macular edema after uneventful phacoemulsification with intraocular lens implantationJ Cataract Refract Surg200228101814181812388034
- CarrilloMMNicolelaMTCystoid macular edema in a low-risk patient after switching from latanoprost to bimatoprostAm J Ophthalmol2004137596696815126179
- WandMGaudioARCystoid macular edema associated with ocular hypotensive lipidsAm J Ophthalmol2002133340340511860980
- TsujikawaASakamotoAOtaMSerous retinal detachment associated with retinal vein occlusionAm J Ophthalmol2010149229130120103055
- EsquenaziSCystoid macular edema in a pseudophakic patient after switching from latanoprost to BAK-free travoprostJ Ocul Pharmacol Ther200723656757018001244
- MatsuuraKSasakiSUotaniRSuccessful treatment of prostaglandin-induced cystoid macular edema with subtenon triamcinoloneClin Ophthalmol201262105210823269859