Abstract
Summary
We report a case of previously unsuspected myeloma, presenting with cornea verticillata due to intracorneal paraprotein deposition.
History
An 85-year-old female presented via her optician with a 4-month history of cloudy vision. She had undergone an uneventful bilateral phacoemulsification surgery 7 years earlier. Extensive spiraling corneal epithelial opacification was noted on slit-lamp examination. On further investigation, she was found to have a previously unsuspected low-grade multiple myeloma. We established the nature of the corneal deposits with corneal epithelial biopsy histopathology and electron microscopy. It is very rare for multiple myeloma to present in this fashion. Ophthalmologists should be aware that such a presentation may rarely be due to systemic multiple myeloma.
Introduction
Corneal deposits of various types have been described in multiple myeloma, monoclonal gammopathy, and essential cryoglobulinemia.Citation1,Citation2 There are only a very few case reports of corneal immunoglobulin (Ig) deposition. We present one such case in which there was intraepithelial deposition of corneal IgG-kappa. In addition, it is noteworthy that the presentation to the ophthalmologist was the presenting complaint leading to the diagnosis of myeloma.
Case report
An 85-year-old lady with bilateral cloudy corneas was referred to ophthalmology as an outpatient from her optometrist. She gave a 3–4 month history of cloudy vision, mainly in her right eye. She had undergone an uneventful bilateral phacoemulsification surgery 7 years earlier.
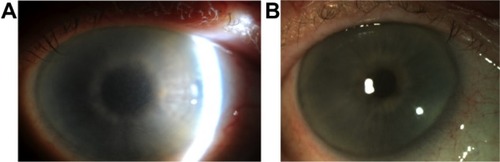
Her visual acuity at presentation was 6/7.5 OU. On examination, she had marked grayish intraepithelial corneal opacities in a pattern of hazy spiraling lines in both eyes (). The corneal stroma and endothelium had normal appearance; there was no evidence of corneal edema. Specular microscopy was not possible. The anterior chamber depth and contents, intraocular lenses, posterior capsule, and fundus examination were normal.
Figure 1 Clinical photographs of the right cornea.
She had a past medical history of ischemic heart disease and osteopenia. Her current medications were aspirin, simvastatin, lisinopril, codeine, and paracetamol.
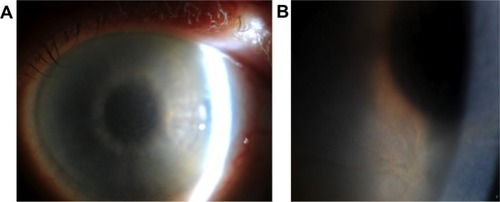
Systemic investigation revealed a raised serum IgG with a kappa paraprotein band (12.4 g/L) on serum protein electrophoresis (). The erythrocyte sedimentation rate was raised (49 mm/hour), and there was a mild kidney impairment with raised urea (8.1 mmol/L) and raised creatinine (118 μmol/L). The random blood glucose, electrolytes, liver function, lipid profile, and calcium profile were normal. Urinary Bence Jones proteins were elevated. There was no evidence of Fabry disease as the lysosomal enzymes were all found to be normal.
Figure 2 Serum immunofixation electrophoresis and its graphical representation.
Abbreviations: ELP, serum protein electrophoresis; G, immunoglobulin G; A, immunoglobulin A; M, immunoglobulin M; K, kappa light chain; L, lambda light chain.
She was referred to the Department of Haematology, Sunderland Royal Hospital, Sunderland, UK, and a bone marrow biopsy was carried out that showed increased plasma cells (11%) with pink staining crystals in the cytoplasm. Free crystals were also seen. These findings were consistent with multiple myeloma.
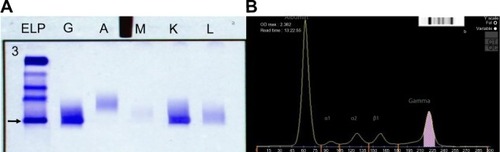
A corneal epithelial biopsy was undertaken and subjected to further laboratory analysis. Immunohistochemistry of the corneal biopsy showed excessive amounts of kappa light chain staining, relative to lambda light chain staining. On transmission electron microscopy, there was evidence of intraepithelial intracellular and extracellular geometrically irregular hexagonal electron dense particles (). These are typically found in crystalline keratopathy due to gammopathy. There was an absence of immunotactoid, a paraprotein also commonly present in these cases, but not detected in our case.
Figure 3 Electron microscopy of the corneal biopsy specimen.
The patient was commenced on systemic chemotherapy with cyclophosphamide and dexamethasone. Six months later, there was significant improvement in corneal clarity ().
Discussion
Corneal epithelial disturbance in a spiraling pattern is variously known as cornea verticillata, vortex keratopathy, and hurricane keratopathy. Well-recognized causes include: Fabry disease;Citation3 drugsCitation4 (amiodarone,Citation5 chloroquine, hydroxychloroquine, indomethacin, chlorpromazine, tamoxifen, meperidine); toxicity of topical medications; and ocular surface failure secondary to chemical and thermal burns, conjunctival malignancy, and cicatrizing conjunctivitis.
In myeloma, an intracorneal accumulation of Ig is well-described. Patients may be asymptomatic or complain of decreased vision,Citation6 irritation,Citation7 photophobia,Citation8 and erosions.Citation9,Citation10 The corneal deposition can be crystalline,Citation10–Citation12 amorphous,Citation6 or a combination.
Other ocular surface manifestations of multiple myeloma include repeated subconjunctival hemorrhages,Citation13 peripheral ulcerative keratitis,Citation14 prominent corneal nerves,Citation9 and band keratopathy.Citation15
Our patient turned out to have intracorneal crystal deposition, although the crystals were too small to be seen on slit-lamp examination. Other causes of intracorneal crystal deposition include cystinosis,Citation16 Schnyder crystalline corneal dystrophy,Citation17 Bietti crystalline corneoretinal dystrophy, tyrosinemia,Citation18 gout, and topical medications (fluoroquinolone).Citation19
The pathophysiology of intracorneal crystal formation in multiple myeloma remains enigmatic. One theory is that the deposits result from elevated Ig levels in the tears and aqueous humor;Citation20 another is that they enter the cornea from the limbal blood vessels; and a third is that the keratocytes themselves synthesize the precipitated Ig. Henderson et alCitation21 discuss that some of the reasons for Ig deposition are: 1) an inherent propensity of some Ig or kappa light chains to crystallize; and 2) local factors in the cornea that may promote deposition, such as temperature, pH, water content, and extracellular matrix deposition. The immunoglobulin substances have been found in serum, tears, urine, aqueous humor, corneaCitation8,Citation22 (subepithelialCitation2,Citation22,Citation23/intraepithelialCitation10 tissues), and bone marrow.
This case is unusual because it is rare to have corneal deposition in multiple myeloma. It is even rarer for it to be the presenting complaint to an ophthalmologist. On searching the literature, we have found a total of 27 case reports of corneal Ig deposition in multiple myeloma. Of these, 17 were crystalline,Citation7 four were amorphous,Citation25 two were hyaline,Citation26 one was granular,Citation27 and no tissue was obtained in three. This suggests that the corneal Ig distribution in multiple myeloma is frequently crystalline. Ig deposits can be both intracellular and extracellular.Citation28 Another distinct pattern of involvement is an immunotactoid pattern. Stirling et alCitation28 showed ultrastructural images of tubular paracrystalline structure of corneal immunoglobulin deposition which were later termed as “immunotactoid keratopathy” by Garibaldi. GaribaldiCitation7 proposed the use of term “immunotactoid keratopathy” to describe corneal Ig deposits in tubular, electron-dense, crystalloid deposits with central lucent core on electron microscopy (they reported two such cases with Ig kapa deposits).
Ig-kappa deposition in the cornea was seen in eleven cases of multiple myeloma,Citation7 although IgG gamma globulin was deposited in three corneas, and IgG lambda was deposited in three cases – with IgG-kappa and lambda in one case, IgD in one case, and IgA in one case. The type of Ig deposited in the cornea was not clarified in seven cases. This suggests that Ig deposition in the cornea is most frequent in the kappa variety of multiple myeloma.
Ig-kappa distribution can affect different corneal layers. It was reported to be deposited in: all layers of the cornea in four cases;Citation20,Citation29–Citation31 only stromal involvement in three cases;Citation8,Citation12 only epithelial involvement in two cases;Citation11,Citation32 epithelium and stromalCitation6 involvement in one case; and endothelium and Descemet’s membraneCitation33 involvement in one case.
Corneal deposition of immunoglobulins in multiple myeloma is rarely in a vortex pattern. Two cases of vortex keratopathy in multiple myeloma have been previously reported. Auran et alCitation32 described a case of crystalline keratopathy in a vortex pattern in a patient with multiple myeloma. However, they did not obtain any pathological material. Their patient had already undergone bilateral phacoemulsification 7 years previously and later developed an endocapsular hematoma that resolved without treatment. There were some similarities between Auran’s case and ours. Both cases had a clinical picture of vortex keratopathy and an Ig-kappa spike on serum electrophoresis. Auran’s case differed in that the patient had decreased vision and glare, while our patient only had decreased vision without glare or photophobia. Their patient had crystalline deposits in the epithelium and stroma, while our patient had deposition only in the epithelium.
Chong et alCitation34 described the second case of vortex keratopathy in multiple myeloma. Their case was diagnosed with multiple myeloma 18 months after first presentation to the ophthalmologist. Again, they did not obtain a corneal biopsy. They did, however, take conjunctival specimens which stained monoclonally for IgG-kappa light chains. Conjunctival electron microscopy showed intracellular hexagonal crystalline structures – similar to our corneal biopsy picture. Their conjunctival specimen also showed some extracellular material in the form of microfibrils, which stained for kappa light chains. This was not evident in our case. Chong et al therefore assumed that the corneal crystalline vortex keratopathy was due to Ig deposition.
Buerk and TuCitation35 reported a patient with multiple myeloma crystalline keratopathy where confocal microscopy showed in vivo crystals in the corneal epithelium and the anterior stroma. They repeated confocal microscopy after 6 months of chemotherapy and demonstrated a decrease in the size and the number of the corneal crystals. Use of in vivo confocal microscopy was also used by Paladini et alCitation36 in a case with bilateral crystalline corneal deposits, due to monoclonal gammopathy. Confocal microscopy has the advantage of being able to image corneal crystalline deposits in vivo and help monitor a decrease in these changes with chemotherapy more quantitatively. However, confocal microscopy is not a histological tissue test and, therefore, cannot confirm the type of material/Ig deposited. We did not have access to confocal microscopy at our center.
Our case is, therefore, the first published case of vortex keratopathy in multiple myeloma with corneal deposition of Ig confirmed by corneal epithelial biopsy.
It is very rare for multiple myeloma to present in this fashion. There are several causes of intracorneal crystalline deposits, and the differentiation is impossible clinically, but laboratory studies – specifically a serum protein electrophoresis – will help detect any unsuspected multiple myeloma.Citation37 Ophthalmologists should be aware that such a presentation may rarely be due to systemic multiple myeloma.
Disclosure
The authors report no conflicts of interest in this work.
References
- OglesbyRBCorneal opacities in a patient with cryoglobulinemia and reticulohistiocytosisArch Ophthalmol196165636613730450
- KremerIWrightPMerinSWeissJPickAlKaufmanHCorneal subepithelial monoclonal kappa IgG deposits in essential cryoglobulinemiaBr J Ophthalmol19897386696732504274
- MassonCCisséISimonVInsalacoPAudranMFabry disease: a reviewJoint Bone Spine200471538138315474388
- HollanderDAAldaveAJDrug-induced corneal complicationsCurr Opin Ophthalmol200415654154815523201
- ChewEGhoshMMcCullochCAmiodarone-induced cornea verticillataCan J Ophthalmol198217396997116220
- BeebeWEWebsterRGJrSpencerWBAtypical corneal manifestations of multiple myeloma. A clinical, histopathologic, and immunohistochemical reportCornea1989842742802509136
- GaribaldiDCGottschJde la CruzZHaasMGreenWRImmunotactoid keratopathy: a clinicopathologic case report and a review of reports of corneal involvement in systemic paraproteinemiasSurv Ophthalmol2005501618015621078
- BarrCCGelenderHFontRLCornea crystalline deposits associated with dysproteinemia. Report of two cases and review of the literatureArch Ophthalmol19809858848896246862
- ParghiCMcknightGTPflugfelderSCProminent corneal nerves in a patient with multiple myelomaCornea200726222022217251817
- PerryHDDonnenfeldEDFontRLIntraepithelial corneal immunoglobulin crystals in IgG-kappa multiple myelomaCornea19931254484508306667
- KlintworthGKBredehoeftSJReedJWAnalysis of corneal crystalline deposits in multiple myelomaAm J Ophthalmol1978863303313102200
- WakitaMKanaiANakajimaAShiraiTSaionjiKCorneal crystalline deposits in multiple myelomaNippon Ganka Gakkai Zasshi1989936665675 Japanese [with English abstract]2510479
- FelipeAFNottageJMRapuanoCJRecurrent bilateral subconjunctival hemorrhage as an initial presentation of multiple myelomaOman J Ophthalmol20125213313422993476
- LimLTRamamurthiSCollinsCEMantrySPeripheral ulcerative keratitis associated with multiple myelomaAnn Acad Med Singapore2011401255055122294068
- WilsonKSAlexanderSChisholmIABand keratopathy in hypercalcemia of myelomaCan Med Assoc J19821261113147074461
- GahlWAKuehlEMIwataFLindbladAKaiser-KupferMICorneal crystals in nephropathic cystinosis: natural history and treatment with cysteamine eyedropsMol Genet Metab2000711–210012011001803
- WeissJSKhemichianAJDifferential diagnosis of Schnyder corneal dystrophyDev Ophthalmol201148679621540632
- ScottCRThe genetic tyrosinemiasAm J Med Genet C Semin Med Genet2006142C212112616602095
- Crystalline keratopathy: spectrum of disease, diagnosis and treatment [webpage on the Internet]San Francisco, CA, USAAmerican Academy of Ophthalmology EyeNet Magazine2008 [cited January 1, 2018]. Available from: http://www.aao.org/aao/publications/eyenet/200801/pearls.cfmAccessed April 28, 2013
- SteuhlKPKnorrMRohrbachJMLischWKaiserlingEThielHJParaproteinemic corneal deposits in plasma cell myelomaAm J Ophthalmol199111133123181900387
- HendersonDWStirlingJWLipsettJRozenbildsMARoberts-ThomsonPJCosterDJParaproteinemic crystalloidal keratopathy: an ultrastructural study of two cases, including immunoelectron microscopyUltrastruct Pathol19931766436688122330
- KnappAJGartnerSHenkindPMultiple myeloma and its ocular manifestationsSurv Ophthalmol19873153433513603371
- HillJCMulliganGPSubepithelial corneal deposits in IgG lambda myelomaBr J Ophthalmol19897375525542503029
- GarnerAKirknessCMCorneal gammopathyCornea19887144493127116
- SekundoWSeifertPMonoclonal corneal gammopathy: topographic considerationsGer J Ophthalmol1996552622678911947
- FrancoisJRabaeyMCorneal dystrophy and paraproteinemiaAm J Ophthalmol19615289590113894566
- GreenEDMorrisonLKLovePEA structurally aberrant immunoglobulin paraprotein in a patient with multiple myeloma and corneal crystals depositsAm J Med19908833043112309746
- StirlingJWHendersonDWRozenbildsMASkinnerJMFilipicMCrystalloidal paraprotein deposits in the cornea: an ultrastructural study of two new cases with tubular crystalloids that contain IgG kappa light chains and IgG gamma heavy chainsUltrastruct Pathol19972143373449205998
- LaibsonPDamianoVX-ray and electron diffraction of ocular and bone marrow crystals in paraproteinemiaScience196916338675815835762191
- KawamuraHSeoTWatanabeIItoIShirasawaHMuranakaYA case of corneal crystalline deposits associated with multiple myelomaNihon Ganka Gakkai Zasshi198892914731478 Japanese3063100
- YamamotoTHishidaAHondaNItoIShirasawaHNagaseMCrystal-storing histiocytosis and crystalline tissue deposition in multiple myelomaArch Pathol Lab Med199111543513542012495
- AuranJDDonnAHymanGAMultiple myeloma presenting as vortex crystalline keratopathy and complicated by endocapsular hematomaCornea19921165845851468223
- HøisenHRingvoldAKildahl-AndersenOCorneal crystalline deposits in multiple myeloma. A case reportActa Ophthalmol (Copenh)19836134935006414237
- ChongEMCampbellRJBourneWMVortex keratopathy in a patient with multiple myelomaCornea19971655925949294696
- BuerkBMTuEConfocal microscopy in multiple myeloma crystalline keratopathyCornea200221661962012131045
- PaladiniIPierettiGGiuntoliMAbbruzzeseGMenchiniUMencucciRCrystalline corneal deposits in monoclonal gammopathy: in-vivo confocal microscopySemin Ophthalmol2013281374023305440
- RobertsonDMNon-cancerous ophthalmic clues to non-ocular cancerSurv Ophthalmol200247539743012431692