Abstract
Purpose
Flat anterior chamber (FAC) in association with overfiltration is a complication after trabeculectomy. The aim of the current study was to investigate the efficacy of injection of an ophthalmic viscoelastic device (OVD) to treat FAC after trabeculectomy in a retrospective consecutive case series study.
Materials and methods
Twenty-five consecutive patients who underwent injection of OVD for the treatment of FAC after trabeculectomy were analyzed. The primary outcome variable was the qualified success of trabeculectomy, which was defined at three different levels by the achievement of one of three IOP-related criteria with or without glaucoma medication. Kaplan–Meier plots were generated to estimate survival functions for trabeculectomy with OVD injection.
Results
Twenty-one patients (21/25 = 84.0%) recovered from FAC by one OVD injection. The postoperative intraocular pressure (IOP) measured at 12 months, 24 months, 36 months, 48 months, and 60 months was 14.7 ± 3.6 mmHg, 15.6 ± 7.0 mmHg, 14.2 ± 2.8 mmHg, 14.2 ± 3.8 mmHg, and 14.6 ± 2.7 mmHg, respectively. All postoperative IOP measurements were significantly lower than the preoperative IOP (P < 0.001). The probabilities of qualified success for 5 years after trabeculectomy with OVD injection were as follows: 24.4% (IOP ≦ 21 mmHg and ≧20% reduction of preoperative IOP), 16.5% (IOP ≦ 16 mmHg and ≧20% reduction) and 6.3% (IOP ≦ 12 mmHg and ≧30% reduction). One patient, who had undergone deep lamellar keratoplasty, experienced a complication associated with the injection of the viscoelastic material, Descemet’s membrane detachment.
Conclusion
Injection of OVD may be effective for the treatment of FAC; however, the long-term success rate was relatively low.
Introduction
The incidence of flat anterior chamber (FAC), a complication associated with overfiltration after a trabeculectomy with mitomycin C, is reported to be 13%–24%.Citation1,Citation2 Persistent FAC causes peripheral anterior synechiae, cataracts, and endothelial dysfunction.Citation3–Citation6 FAC has been successfully treated with atropine eye drops, a firmly applied eye patch, balanced salt solution injections, sodium hyaluronate, air bubbles, and injection of perfluoropropane or sulfur hexafluoride gas into the anterior chamber.Citation7–Citation11 Fisher et alCitation8 described using sodium hyaluronate to treat FAC in 1982, and Hoffman et alCitation7 reported using Healon 5® (Abbott Medical Optics, Inc, Santa Ana, CA, USA) to treat FAC after trabeculectomy in 2002.
This retrospective, consecutive case series study investigated the efficacy of injecting an ophthalmic viscoelastic device (OVD) to treat FAC after trabeculectomy.
Materials and methods
This study followed the tenets of the Declaration of Helsinki and was approved by the Ethics Committee of the Keio University School of Medicine (authorization number 2010214). This study included 25 consecutive patients who received OVD injections to treat FAC occurring after a trabeculectomy with mitomycin C between April 1, 2004 and March 31, 2008. In this retrospective study, we included all the subjects who underwent viscoelastic injection for the treatment of grade 2 FAC (entire iridocorneal touch without contact between the lens and the cornea) without conjunctival leakage.Citation12 There were no exclusion criteria. These patients had no leakage from the conjunctiva in the early postoperative period. All trabeculectomy surgeries were performed by one of three glaucoma specialists educated at the same institute. The trabeculectomies were performed using a limbal-based conjunctival fap, sub-Tenon dissection, and hemostasis. A half-thickness 4.0 × 4.0 mm rectangular scleral flap was fashioned in the superior area. A 4.0 × 4.0 mm sponge soaked in a 0.4 mg/mL solution of mitomycin C was applied for 3–5 minutes, and the area was irrigated thoroughly with 500 cc of physiological saline. The trabeculectomy was followed by a peripheral iridectomy. The scleral flap was sutured with 10-0 nylon sutures (Mani, Inc, Tochigi, Japan). All patients were given a postoperative regimen of topical 0.5% levofloxacin (Cravit® ophthalmic solution; Santen Pharmaceutical Co, Ltd, Osaka, Japan) three times per day, and betamethasone eye drops (Sanbetasone®; Santen Pharmaceutical Co, Ltd) four times per day.
OVD injections were performed after applying oxybuprocaine hydrochloride (Benoxil ophthalmic solution; Santen Pharmaceutical Co, Ltd) topically as an anesthetic, and disinfected with 5% povidone–iodine (Isodine; Meiji Seika Co, Ltd, Tokyo, Japan). An Opegan Hi® (Santen Pharmaceutical Co, Ltd), Healon®, or Healon 5® (AMO Japan, Inc, Tokyo, Japan) OVD was injected into the anterior chamber through a paracentesis made during the trabeculectomy. Using a 23 gauge blunt cannula, the OVD was injected until the anterior chamber was deepened sufficiently. After the injection, the intraocular pressure (IOP) was checked using a Tono-Pen® XL (Reichert™ Technologies, Inc, Buffalo, NY, USA). If the IOP was less than 5 mmHg, additional OVDs were injected into the anterior chamber until the IOP was greater than 10 mmHg.
We considered the patients’ age, sex, type of glaucoma, pre-operative lens status, surgical procedure (with or without cataract surgery), the type of OVD, pre- and post-trabeculectomy IOP, the IOP 24 hours after OVD injection, the number of laser suture lysis procedures, the prevalence of choroidal detachment, treatment prior to the OVD injection, the number of OVD injections required, the time from injection to FAC recovery, and any complications associated with the OVD injection. Goldmann applanation tonometry was used to measure the IOP each day during the admission period, 1 month after surgery, 3 months after surgery, and every 3 months thereafter up to 60 months after surgery.
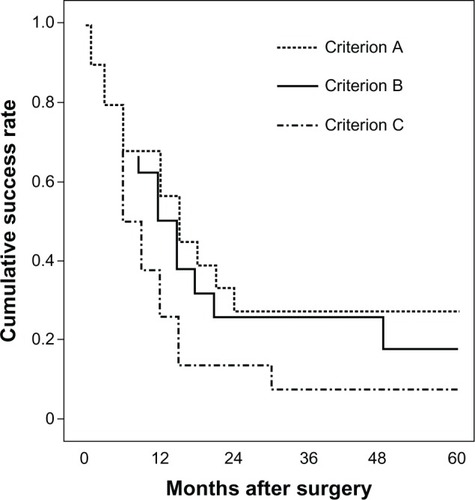
The primary outcome variable was the qualified success of the trabeculectomy, defined by three levels of IOP-related criteria with or without glaucoma medication, as follows: (1) IOP ≤21 mmHg, reduced ≥20% from the preoperative level (ie, the last IOP value before surgery); (2) IOP ≤16mmHg, reduced ≥20% from the preoperative level; or (3) IOP ≤12 mmHg, reduced ≥30% from the pre-operative level.Citation13,Citation17 The surgery was deemed to have failed if these criteria were not satisfied at two consecutive visits, or if a secondary surgery to lower the IOP was required. Kaplan–Meier plots were generated to estimate the survival functions for trabeculectomy with OVD injection. A one-way analysis of variance followed by Bonferroni’s multiple comparison test was used for statistical analysis of the IOP before and after trabeculectomy. Significance was defined as P < 0.05. Statistical analysis was performed using SPSS software, version 21.0 (IBM Software, Las Vegas, NV, USA).
Results
Demographic characteristics are listed in . After OVD injection treatment, all subjects had sufficient anterior chamber depth to achieve maintained anterior chamber. None of the subjects had total apposition between the iris and cornea with lens–cornea contact.
Table 1 Demographic characteristics of 25 patients given OVD injections
The number of OVD injections, the IOP 24 hours after injection, time from the injection until the FAC improved, and the type of injected OVD are shown in . Of the 25 patients, 21 (84.0%) recovered from FAC with one OVD injection; three patients required two injections, and one patient required four injections. All subjects recovered from FAC after OVD treatment without any other surgical procedures.
Table 2 Properties of OVD injection procedures
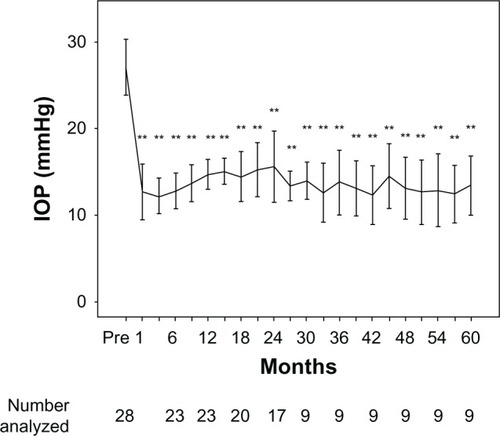
The mean preoperative IOP was 28.8 ± 9.2 mmHg. The postoperative IOP measured at 12 months, 24 months, 36 months, 48 months, and 60 months was 14.7 ± 3.6 mmHg, 15.6 ± 7.0 mmHg, 14.2 ± 2.8 mmHg, 14.2 ± 3.8 mmHg, and 14.6 ± 2.7 mmHg, respectively. All postoperative IOP measurements were significantly lower than the preoperative IOP (P < 0.001; ).
Figure 1 IOP measured prior to trabeculectomy, 1 month after surgery, and at 3-month intervals from the time of surgery until 60 months after surgery.
Abbreviation: IOP, intraocular pressure; pre, preopearative IOP.
The trabeculectomy postoperative success rate is shown in . The probability of 5-year success after trabeculectomy with OVD-treated FAC was 24.4% (criterion A), 16.5% (criterion B), and 6.3% (criterion C) ().
Figure 2 Survival curves of surgical failure of trabeculectomy with OVD-treated FAC.
Abbreviations: OVD, ophthalmic viscoelastic device; FAC, flat anterior chamber; IOP, intraocular pressure.
One patient, who had undergone deep lamellar keratoplasty, experienced a complication associated with the injection of the OVD – Descemet’s membrane detachment. Healon 5® was injected through the paracentesis, and was accidentally injected between Descemet’s membrane and the stroma where lamellar keratoplasty had been performed. The OVD could not be removed from the area between Descemet’s membrane and the stroma by aspiration with the cannula or by air tamponade from the anterior chamber. Therefore, the donor cornea was removed, irrigated with balanced salt solution to wash out the OVD, and resutured on the recipient cornea.
In one patient, the IOP rose to 38 mmHg the day after a Healon® OVD injection, but fell to 12 mmHg after two laser suture lysis procedures. This was the only subject to experience an IOP higher than 20 mmHg after an OVD injection.
Discussion
To our knowledge, this is the largest case series study analyzing the results of OVD injection to treat FAC after trabeculectomy. In our study, a single OVD injection resolved FAC and achieved deep anterior chamber in 84% of the subjects. Case reports by Hoffman et al,Citation7 as well as Gutierrez-Ortiz and Moreno-LópezCitation13 on the use of OVD injection to treat postoperative FAC suggested that OVD injection is a simple and effective procedure for managing this complication. Our case series study showed that OVD injection is an effective treatment for FAC after trabeculectomy.
In our study, the long-term, post-trabeculectomy IOP in patients with FAC treated by OVD was significantly lower than the preoperative IOP. We observed an IOP of 14.6 ± 2.7 mmHg 5 years after the trabeculectomy. This result suggests that OVD injection is an effective treatment for FAC. However, previous studies have measured post-trabeculectomy IOPs of 10.0 mmHg, 10.3 mmHg, and 11.1 mmHg; our results were relatively high in comparison.Citation14–Citation17
Our study found success rates of trabeculectomy after OVD injection of 24.4% (criterion A), 16.5% (criterion B), and 6.3% (criterion C). The qualified success rates of trabeculectomy reported previously are 71%Citation18 (criterion A), 61%,Citation15 57%,Citation17 60%Citation19 (criterion B), and 40%,Citation19 44%,Citation17 and 52%Citation15 (criterion C). Thus, our study, which included only patients who were treated with OVD for FAC after trabeculectomy, found a lower success rate for trabeculectomy along with the higher postoperative IOP.
In a randomized, controlled trial, de Barros et alCitation12 compared three groups treated for FAC: one with the anterior chamber reformed with OVD; one with the anterior chamber reformed with a balanced salt solution and concurrent drainage of choroidal effusion; and one treated with pharmacologic therapy. The authors concluded that the final IOP tended to be lower with reformation with OVD. The success rate of trabeculectomy in our study, which included only patients with FAC treated with OVD, was lower than that found in previous studies. However, in de Barros et al’sCitation12 study, trabeculectomy complicated by FAC had a higher success rate when the FAC was treated by OVD injection than by other procedures. Thus, OVD injection may be the best procedure for treating FAC after trabeculectomy.
One subject who had undergone deep lamellar keratoplasty showed Descemet’s membrane detachment. A blunt cannula can be inserted in the gap between the stroma and Descemet’s membrane, especially in lamellar surgery patients.Citation20 Therefore, extra care is required when injecting an OVD into patients who have undergone lamellar surgery, such as Descemet’s stripping endothelial keratoplasty or deep lamellar keratoplasty.
The limitations of this study include its retrospective case series design and a lack of analysis according to OVD type; we did not evaluate the efficacy of the different types of OVD separately. Another limitation is that we did not evaluate the effect of peripheral anterior synechiae formation after OVD injection because of a lack of accurate information about peripheral anterior synechiae in the medical record. The third limitation is that, after the 30-month follow up, eleven subjects were lost to follow up, four subjects underwent additional glaucoma surgery, and one subjects had retinal detachment. The success rate or the postoperative IOP may be affected by the relatively large number of participants lost to follow up.
In conclusion, our findings indicate that OVD injection is effective for treating FAC after trabeculectomy.
Disclosure
The authors report no conflicts of interest in this work.
References
- JampelHDMuschDCGillespieBWLichterPRWrightMMGuireKECollaborative Initial Glaucoma Treatment Study GroupPerioperative complications of trabeculectomy in the collaborative initial glaucoma treatment study (CIGTS)Am J Ophthalmol20051401162215939389
- EdmundsBThompsonJRSalmonJRWormaldRPThe National Survey of Trabeculectomy. III. Early and late complicationsEye (Lond)200216329730312032721
- PhillipsCIClarkCVLevyAMPosterior synechiae after glaucoma operations: aggravation by shallow anterior chamber and pilocarpineBr J Ophthalmol19877164284323620422
- KimYYJungHRThe effect of flat anterior chamber on the success of trabeculectomyActa Ophthalmol Scand19957332682727493243
- StewartWCShieldsMBManagement of anterior chamber depth after trabeculectomyAm J Ophthalmol1988106141443394767
- FiorePMRichterCUArzenoGThe effect of anterior chamber depth on endothelial cell count after filtration surgeryArch Ophthalmol198910711160916112818280
- HoffmanRSFineIHPackerMStabilization of flat anterior chamber after trabeculectomy with Healon5J Cataract Refract Surg200228471271411955917
- FisherYLTurtzAIGoldMCohenBZUramMUse of sodium hyaluronate in reformation and reconstruction of the persistent flat anterior chamber in the presence of severe hypotonyOphthalmic Surg198213108198217177558
- OsherRHCionniRJCohenJSRe-forming the flat anterior chamber with HealonJ Cataract Refract Surg19962244114158733842
- StewartRHKimbroughRLA method of managing flat anterior chamber following trabeculectomyOphthalmic Surg19801163823837402579
- FranksWAHitchingsRAIntraocular gas injection in the treatment of cornea-lens touch and choroidal effusion following fistulizing surgeryOphthalmic Surg199021128318342096342
- de BarrosDSNavarroJBMantravadiAVThe early flat anterior chamber after trabeculectomy: a randomized, prospective study of 3 methods of managementJ Glaucoma2009181132019142129
- Gutiérrez-OrtizCMoreno-LópezMHealon5 as a treatment option for recurrent flat anterior chamber after trabeculectomyJ Cataract Refract Surg200329463512686219
- FontanaHNouri-MahdaviKCaprioliJTrabeculectomy with mitomycin C in pseudophakic patients with open-angle glaucoma: outcomes and risk factors for failureAm J Ophthalmol2006141465265916564799
- LawSKShihKTranDHColemanALCaprioliJLong-term outcomes of repeat vs initial trabeculectomy in open-angle glaucomaAm J Ophthalmol20091485685695. e119596220
- Palanca-CapistranoAMHallJCantorLBMorganLHoopJWuDunnDLong-term outcomes of intraoperative 5-fuorouracil versus intraoperative mitomycin C in primary trabeculectomy surgeryOphthalmology2009116218519018930550
- FontanaHNouri-MahdaviKLumbaJRalliMCaprioliJTrabeculectomy with mitomycin C: outcomes and risk factors for failure in phakic open-angle glaucomaOphthalmology2006113693093616647135
- GeddeSJSchiffmanJCFeuerWJHerndonLWBrandtJDBudenzDLTube versus Trabeculectomy Study GroupTreatment outcomes in the Tube Versus Trabeculectomy (TVT) study after five years of follow-upAm J Ophthalmol20121535789803. e222245458
- SolusJFJampelHDTraceyPAComparison of limbus-based and fornix-based trabeculectomy: success, bleb-related complications, and bleb morphologyOphthalmology2012119470371122226886
- RasouliMMatherRTingeyDDescemet membrane detachment following viscoelastic injection for posttrabeculectomy hypotonyCan J Ophthalmol200843225425518347645