Abstract
Purpose
To assess the relationship between tear osmolarity and dry eye symptoms in patients with diabetes.
Patients and methods
Fifty patients with diabetes were enrolled. Demographic information and past medical history were recorded. Symptoms were assessed using the ocular surface disease index (OSDI). Tear osmolarity of each eye was measured with the TearLab® Osmolarity System.
Results
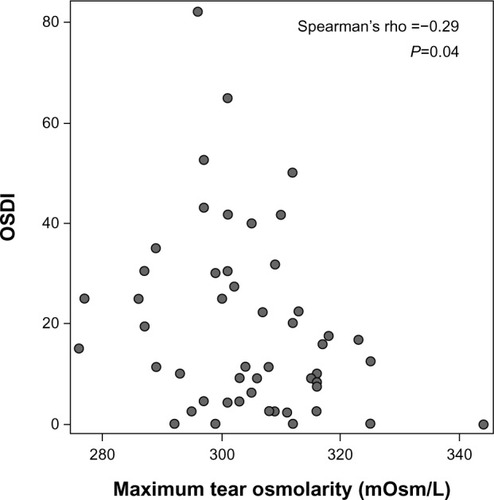
The majority of the subjects were female (76%), African American (56%), and/or had a diagnosis of type 2 diabetes (82%). The mean ± standard deviation (SD) for age was 54.6±13.4, and maximum tear osmolarity was 304.6±12.7 mOsm/L. Men had higher osmolarity than women (mean ± standard error (SE) 311.8±4.0 mOsm/L versus 302.3±1.9 mOsm/L, P=0.02). Age, race, use of artificial tears, years of diabetes, and hemoglobin A1c did not have a statistically significant association with tear osmolarity. Longer duration of diabetes was associated with lower (less severe) OSDI scores (r=−0.35, P=0.01). Higher tear osmolarity was associated with lower (less severe) OSDI scores (r=−0.29, P=0.04).
Conclusion
Approximately half of the diabetic subjects in our study had elevated tear osmolarity, and half of our population also reported symptoms consistent with dry eye disease. However, the two were slightly inversely related in that those with higher osmolarity reported fewer symptoms. Subjects with a longer duration of diabetes also reported fewer dry eye symptoms. Therefore, health care providers should be aware that patients who are most likely to have ocular surface disease, including those with long-standing diabetes, may not experience symptoms and seek care in a timely manner.
Keywords:
Introduction
In 2007, the Dry Eye Workshop (DEWS) defined dry eye as “a multifactorial disease of the tears and ocular surface that results in symptoms of discomfort, visual disturbance, and tear film instability. It is accompanied by increased osmolarity of the tear film and inflammation of the ocular surface.”Citation1 Dry eye disease (DED) is common and significantly affects quality of life. The estimated prevalence of DED for women and men over the age of 50 years in the United States is 3.2 million and 1.6 million, respectively.Citation2,Citation3 Compared with age-matched controls, patients with dry eye are two to four times more likely to experience difficulty with reading, carrying out professional work, using a computer, watching television, and driving.Citation4
The assessment of tear film osmolarity may be helpful in the study of DED, as tear osmolarity changes have been shown to reflect disturbances of the tear film.Citation5–Citation10 A recent study using electrical impedance to measure tear osmolarity found that dry eye disease could be diagnosed with a sensitivity of 87% and a specificity of 81% when 316 mOsm/L was used as a cutoff.Citation9 In another study, tear osmolarity had superior diagnostic performance over other dry eye tests, including tear break up time, corneal staining, conjunctival staining, Schirmer’s test, and meibomian gland grading. In that study, a tear osmolarity cutoff of 312 mOsm/L yielded a sensitivity of 73% and a specificity of 92% for diagnosing dry eye.Citation10
Many systemic diseases such as diabetes can lead to DED through a variety of mechanisms.Citation11–Citation14 Although the association between diabetes and dry eye is complex,Citation15 most studies support that diabetics experience high rates of DED.Citation15–Citation20 In one study, 53% of subjects with either diabetes or borderline diabetes had self-reported, clinically significant dry eyes.Citation15 When severe, dry eye can cause ocular surface abnormalities such as superficial punctate erosions, epithelial defects, and corneal ulcers, which can lead to permanent corneal scarring. It is important to diagnose and treat dry eye in patients with diabetes, because they are already at risk for developing corneal problems. One study reported that 47%–64% of diabetic patients have primary corneal lesions during their lifetime.Citation21
As tear osmolarity has been proposed as an objective test to diagnose and follow DED,Citation1 we sought to examine whether this would be a useful test in diabetic subjects, with the hope that an early diagnosis of DED could help prevent complications and improve quality of life. Despite numerous studies describing an association between diabetes and DED, to our knowledge, there are few publications describing tear osmolarity as a marker of dry eye severity in diabetes.Citation22–Citation24 Additionally, we sought to examine how self-reported dry eye severity related to tear osmolarity in this population. We hypothesized that diabetic subjects would have increased dry eye symptoms and signs, including increased tear osmolarity, and that these would correlate with various parameters of diabetic control and complications. To test this hypothesis, we analyzed the relationship between tear osmolarity and dry eye symptoms in patients with type 1, type 2, and steroid-induced diabetes.
Materials and methods
Subjects were recruited from ophthalmology and endocrinology practices at an academic medical center during the summers of 2010 and 2012. Inclusion criteria were age over 18 years and a diagnosis of diabetes. Exclusion criteria were similar to previous studies of dry eye and tear osmolarity and included history of any significant ocular surface disease or ocular inflammation (other than keratoconjunctivitis sicca), history of ocular surgery within the past year, contact lens wear during the previous month, and the use of eye medications or artificial tears within 2 hours of checking tear osmolarity.Citation25,Citation26 Past medical history, including medications, medical conditions, ocular history, years of diabetes, use of insulin, and a hemoglobin A1c (HbA1c) value within the last 3 months was obtained. Symptoms of DED were assessed with the ocular surface disease index (OSDI; Allergan, Inc, Irvine, CA, USA). The OSDI consists of 12 questions on symptoms within the past week and yields scores ranging from 0 (least severe) to 100 (most severe). A score of 12 is typically used as a cutoff for normal, 13–22 for mild dry eye, 23–32 for moderate dry eye, and ≥33 for severe dry eye.Citation27,Citation28
Tear osmolarity was measured in each eye with the TearLab® Osmolarity System (TearLab Corporation, San Diego, CA, USA). The system was stored in a temperature and humidity controlled environment, and these values were logged prior to each measurement of tear osmolarity. The system was calibrated at the beginning of each study day according to the manufacturer’s instructions; the test cards used for each tear osmolarity measurement were from the same lot numbers as the test cards used to calibrate the machine each day. Tear samples were collected atraumatically from the lateral tear meniscus of the right eye and then the left eye using Pen 1 only for all measurements. A tear osmolarity value of 305 mOsm/L was used as the cutoff for mild dry eye,Citation6 and 316 mOsm/L was used as the cut-off for more severe dry eye disease.Citation29
Statistical analysis
As recommended by the TearLab® manufacturer, statistical analysis was performed using the maximum osmolarity measurement value of the two eyes. Unless specifically stated, the osmolarity in this analysis will refer to the maximum osmolarity measurement of the two eyes. Statistical analysis using the average tear osmolarity of both eyes is presented in the supplementary materials (Table S1, Table S2 and Figure S1). Patient characteristics with continuous measurements were assessed using Spearman rank-order correlation coefficients to examine pairwise relationships with tear osmolarity or OSDI scores. The differences in tear osmolarity or OSDI between different levels of categorical characteristics were compared using one-way analysis of variance (ANOVA). All analysis was performed in Statistical Applications Software version 9.3 (SAS Inc, Cary, NC, USA).
Results
Subject characteristics
Fifty subjects (38 females and 12 males) with a mean (±standard deviation [SD]) age of 54.6±13.4 years, ranging from 19 to 73 years old were recruited (). The majority of subjects were female (76%), African American (56%), and/or had type 2 diabetes (82%). Sixty percent of subjects required insulin treatment, 24% of subjects had a diagnosis of diabetic nephropathy, 18% of subjects had a diagnosis of diabetic retinopathy, and 38% of subjects had a diagnosis of peripheral neuropathy. Thirty-six percent of subjects had an HbA1c value below 7.0% within the previous 3 months, and 20% of subjects had an HbA1c ≥9.0%. Fifteen (30%) subjects reported current use of artificial tears, with frequency ranging from once per week to three times per day. None of the patients reported recent use of topical cyclosporine or ophthalmic ointments. Twenty-seven subjects (54%) had a tear osmolarity ≤305 mOsm/L, and ten subjects (20%) had a tear osmolarity ≥316 mOsm/L (). The mean of the patients’ maximum tear osmolarity was 304.6±12.7 mOsm/L ().
Table 1 Baseline characteristics of subjects
Based on OSDI symptom scores, 24 subjects were classified as normal (48%), eight subjects had mild dry eye (16%), nine subjects had moderate dry eye (18%) and nine subjects had severe dry eye (18%; ).
Associations with tear osmolarity and dry eye symptoms (OSDI)
On average, men had higher osmolarity than women (mean, 311.8 mOsm/L [95% confidence interval {CI} 305.1, 318.5] versus [vs] 302.3 mOsm/L [298.5, 306.1], P=0.02) (). Among our study population, age, race, use of artificial tears, duration of diabetes, years of insulin use, and HbA1c were not significantly associated with tear osmolarity ( and ).
Table 2 Differences in categorical variables by either tear osmolarity or OSDI using maximum tear osmolarity for analysis
Table 3 Correlations between continuous variables and either tear osmolarity or OSDI using maximum tear osmolarity for analysis
There was no significant effect of age, race, sex, years of insulin use, or HbA1c value on OSDI symptom scores in our study population ( and ). Longer duration of diabetes was associated with lower OSDI scores (r=−0.35, P=0.01) ().
Subjects with higher tear osmolarity had significantly lower OSDI values (r=−0.29, P=0.04) ( and ) with 13 of 24 (54%) nonsymptomatic (OSDI <13) patients having high osmolarity (>305), compared with ten of 26 (38%) symptomatic patients (OSDI ≥13). Subjects using artificial tears had worse OSDI scores than those not using artificial tears; however, this finding was not statistically significant (25.6 [16.7, 34.4] vs 16.7 [10.9, 22.5], P=0.11) ().
Discussion
Tear osmolarity and diabetes
Our population of diabetic subjects had an average maximum tear osmolarity of 304.6±12.7 mOsm/L with 46% having a tear osmolarity >305 mOsm/L, which is consistent with mild dry eye using the cutoffs described by Versura et al.Citation6 Our findings are similar to the findings of Najafi et al,Citation24 who found that in 243 subjects with type 2 diabetes, the mean tear osmolarity using the TearLab® system was 302±14 mOsm/L. The slightly lower average tear osmolarity found in their study is not unexpected, as they reported the mean of the average tear osmolarity of both eyes instead of the average maximum tear osmolarity.
However, tear osmolarity in our diabetic population was lower than that found by Sağdik et al,Citation22 who found an average tear osmolarity of 320±22 mOsm/L in diabetic subjects and 308±18 mOsm/L in controls. Glycemic control was similar in our study and that of Sağdik et al, with a mean HbA1c of 7.9% in both studies. One possible explanation for the difference in tear osmolarity is that Sağdik et al required an eye drop washout period of 12 hours and ointment washout of 5 days, whereas our study required that subjects not use any eye drops for a period of 2 hours as recommended by TearLab and as employed by other tear osmolarity studies.Citation25,Citation26,Citation30 Because 30% of our subjects reported using artificial tears, future studies in our population with a longer washout period may find a maximum tear osmolarity closer to the value found by Sağdik et al.Citation22
We also studied whether or not markers of diabetic severity correlated with tear osmolarity. We did not find a significant relationship between tear osmolarity and the duration of diabetes, HbA1c level, or use of insulin. This is similar to the findings of Aragona et al,Citation23 who found that tear osmolarity in patients with type 1 diabetes was not correlated with HbA1c, diabetes duration, or retinopathy. Similarly, Sağdik et alCitation22 did not find a correlation between tear osmolarity and HbA1c; however, their study did find that tear osmolarity increased with duration of diabetes.Citation22
Relationship of dry eye symptoms with diabetic severity markers
Based on OSDI symptom scores, 52% of our diabetic population had at least mild dry eye, and subjects with a shorter duration of diabetes reported the greatest symptoms, whereas patients with longstanding diabetes reported fewer symptoms. The frequency of dry eye symptoms in our study is similar to that of Manaviat et al,Citation31 who found that 54% of 199 diabetic subjects had dry eye symptoms. In contrast to our study, Manaviat et al found a significant positive association between dry eye syndrome and the duration of diabetes. However, our finding that patients with longstanding diabetes had fewer DED symptoms is in agreement with previous evidence showing that, over time, poorly controlled diabetes can result in reduced corneal sensation,Citation32–Citation36 and therefore, reduced dry eye symptoms. Moreover, in vivo confocal microscopy has shown that diabetic patients have reduced corneal nerve fiber length, thickness, and branching compared with non-diabetic controls.Citation37–Citation39 Similarly, patients with severe diabetic neurotrophic keratopathy exhibit signs of severe dryness with very few symptoms.Citation11
We did not find a relationship between DED symptoms and HbA1c in our study. This is in contrast to the results of previous research,Citation17,Citation19,Citation24,Citation31 including the results of Kaiserman et al,Citation17 who found a greater use of artificial tears among diabetic subjects with a higher HbA1c. It is possible that HbA1c levels did not correlate with dry eye symptoms in our study because HbA1c reflects only the average blood glucose level over the previous 3 months. Therefore, HbA1c levels may not necessarily correlate with decreased corneal sensation, which can affect the perception of dry eye symptoms and likely takes years of poorly controlled diabetes to develop.
Tear osmolarity and dry eye symptoms in diabetic patients
In our diabetic population, subjects with higher tear osmolarity reported fewer dry eye symptoms. This association is the opposite of that found in a previous study showing a significant small positive correlation between tear osmolarity and OSDI score among the general population and an even stronger correlation among moderate dry eye subjects.Citation6 One possible explanation for the negative correlation seen in our study is that, as mentioned previously, diabetic subjects may have reduced corneal sensitivity,Citation34,Citation35 which could lead to decreased awareness of dry eye symptoms. Reduced corneal sensation can also lead to a reduced blink rate and increased tear evaporation.Citation14 In addition, diabetic patients also show reduced tear production, with some studies showing a reduction in basal tear productionCitation32,Citation35 and others showing a reduction in reflex tearing only.Citation33 Both increased tear evaporation and reduced tear production can result in increased tear osmolarity.Citation40 Therefore, it is possible that diabetic patients with a higher tear osmolarity resulting from increased tear evaporation and reduced tear production may also report a lower OSDI score because of their decreased corneal sensation.
Limitations
Our study did not have sufficient power to determine whether there is a relationship between type of diabetes (type 1, type 2, steroid-induced), diabetic microvascular complications (retinopathy, neuropathy, or nephropathy) and tear osmolarity or DED symptoms. Future studies enrolling a larger number of diabetic subjects that also include analysis of corneal sensitivity and other markers of DED will be helpful in diagnosis and treatment of dry eye disease in this population.
Conclusion
Approximately half of our diabetic subjects had a tear osmolarity consistent with dry eye disease and 52% reported DED symptoms consistent with at least mild dry eye disease, but we found that subjects with higher tear osmolarity reported fewer dry eye symptoms. We also found that subjects with a longer duration of diabetes reported fewer dry eye symptoms. Therefore, health care providers should be aware that patients with long-standing diabetes may not experience symptoms and seek care. It is important that diabetics receive regular eye exams not only to check for signs of diabetic retinopathy, but also to evaluate patients for occult dry eye disease which could be affecting their vision.
Acknowledgment
Nicole Fuerst and Nicole Langelier contributed equally to this work.
Supplementary materials
Figure S1 Average tear osmolarity versus OSDI.
Note: Subjects with a higher average tear osmolarity trended toward having a lower OSDI value.
Abbreviation: OSDI, ocular surface disease index.
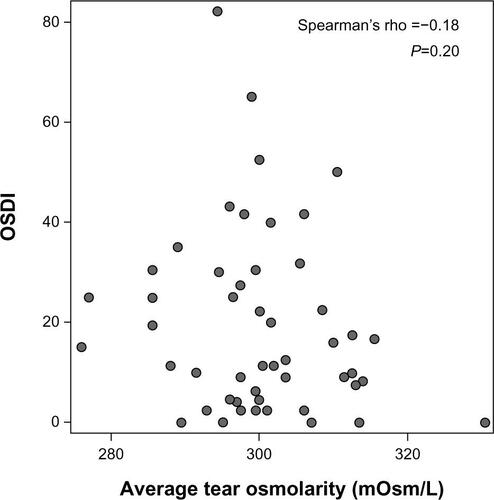
Table S1 Differences in categorical variables by either tear osmolarity or OSDI
Table S2 Correlations between continuous variables and either tear osmolarity or OSDI
Disclosure
Mina Massaro-Giordano receives funding support from Research to Prevent Blindness. Vatinee Y Bunya has received research supplies from TearLab® for a separate study and receives support from the National Eye Institute (K12-EY-015398) and Research to Prevent Blindness. Maxwell Pistilli receives support from a grant from the National Eye Institute (P30 EY001583). The remaining authors have no conflicts of interest to report.
References
- The definition and classification of dry eye disease: Report of the definition and classification subcommittee of the International Dry Eye WorkShop (2007)The Ocular Surface200752759217508116
- SchaumbergDASullivanDABuringJEDanaMRPrevalence of dry eye syndrome among US womenAm J Ophthalmol2003136231832612888056
- SchaumbergDADanaRBuringJESullivanDAPrevalence of dry eye disease among US men: estimates from the physicians’ health studiesArch Ophthalmol2009127676376819506195
- MiljanovićBDanaRSullivanDASchaumbergDAImpact of dry eye syndrome on vision-related quality of lifeAm J Ophthalmol2007143340941517317388
- LiuHBegleyCChenMA link between tear instability and hyperosmolarity in dry eyeInvest Ophthalmol Vis Sci20095083671367919324847
- VersuraPProfazioVCamposECPerformance of tear osmolarity compared to previous diagnostic tests for dry eye diseasesCurr Eye Res201035755356420597641
- KeechASenchynaMJonesLImpact of time between collection and collection method on human tear fluid osmolarityCurr Eye Res201338442843623402632
- TomlinsonAKhanalSRamaeshKDiaperCMcFadyenATear film osmolarity: determination of a referent for dry eye diagnosisInvest Ophthalmol Vis Sci200647104309431517003420
- JacobiCJacobiAKruseFECursiefenCTear film osmolarity measurements in dry eye disease using electrical impedance technologyCornea201130121289129222001814
- LempMABronAJBaudouinCTear osmolarity in the diagnosis and management of dry eye diseaseAm J Ophthalmol20111515792798. e121310379
- Alves MdeCCarvalheiraJBMóduloCMRochaEMTear film and ocular surface changes in diabetes mellitusArqs Bras Oftalmol200871696103
- GoebbelsMTear secretion and tear film function in insulin dependent diabeticsBr J Ophthalmol2000841192110611093
- Figueroa-OrtizLCJiménez RodriguezEGarcia-BenAGarcia-CamposJStudy of tear function and the conjunctival surface in diabetic patientsArch Soc Esp Oftalmol2011864107112 Spanish21569919
- InoueKOkugawaKAmanoSBlinking and superficial punctate keratopathy in patients with diabetes mellitusEye (Lond)200519441842115286669
- HomMDe LandPSelf-reported dry eyes and diabetic historyOptometry2006771155455817145567
- ChiangPPLamoureuxELZhengYFrequency and risk factors of non-retinopathy ocular conditions in people with diabetes: the Singapore Malay Eye StudyDiabet Med2013302e32e4023074990
- KaisermanIKaisermanNNakarSVinkerSDry eye in diabetic patientsAm J Ophthalmol2005139349850315767060
- SeifartUStrempelIThe dry eye and diabetes mellitusOphthalmologe1994912235239 German8012143
- NeppJAbelaCPolzerIDerbolavAWedrichAIs there a correlation between the severity of diabetic retinopathy and keratoconjunctivitis sicca?Cornea200019448749110928764
- OzdemirMBuyukbeseMACetinkayaAOzdemirGRisk factors for ocular surface disorders in patients with diabetes mellitusDiabetes Res Clin Pract200359319519912590016
- SchultzROVan HornDLPetersMAKlewinKMSchuttenWHDiabetic keratopathyTrans Am Ophthalmol Soc1981791801997342400
- SağdikHMTetikoğluMUçarFUğurbasşSCUğurbasşSHTear film osmolarity in patients with diabetes mellitusOphthalmic Res20135011523445780
- AragonaPGiuffridaSDi StefanoGOcular surface changes in type 1 diabetic patientsAdv Exp Med Biol2002506Pt A66767212613975
- NajafiLMalekMValojerdiAEDry eye and its correlation to diabetes microvascular complications in people with type 2 diabetes mellitusJ Diabetes Complications201327545946223726741
- SullivanBDWhitmerDNicholsKKAn objective approach to dry eye disease severityInvest Ophthalmol Vis Sci201051126125613020631232
- SullivanBDCrewsLASonmezBClinical utility of objective tests for dry eye disease: Variability over time and implications for clinical trials and disease managementCornea20123191000100822475641
- MillerKLWaltJGMinkDRMinimal clinically important difference for the ocular surface disease indexArch Ophthalmol201012819410120065224
- SchiffmanRMChristiansonMDJacobsenGHirschJDReisBLReliability and validity of the ocular surface disease indexArch Ophthalmol2000118561562110815152
- TomlinsonAMcCannLCPearceEIComparison of human tear film osmolarity measured by electrical impedance and freezing point depression techniquesCornea20102991036104120577088
- Tearlab.com [homepage on the internet]TearLab™ research guide tips and recommendations. 930082 rev. B TearLab research guide Available from: http://www.tearlab.com/products/doctors/research.htmAccessed October 19, 2013
- ManaviatMRRashidiMAfkhami-ArdekaniMShojaMRPrevalence of dry eye syndrome and diabetic retinopathy in type 2 diabetic patientsBMC Ophthalmol200881018513455
- DogruMKatakamiCInoueMTear function and ocular surface changes in noninsulin-dependent diabetes mellitusOphthalmology2001108358659211237914
- SaitoJEnokiMHaraMMorishigeNChikamaTNishidaTCorrelation of corneal sensation, but not of basal or reflex tear secretion, with the stage of diabetic retinopathyCornea2003221151812502941
- NielsenNVCorneal sensitivity and vibratory perception in diabetes mellitusActa Ophthalmol (Copenh)1978563406411581131
- CousenPCackettPBennettHSwaKDhillonBTear production and corneal sensitivity in diabetesJ Diabetes Complications200721637137317967709
- YoonKCImSKSeoMSChanges of tear film and ocular surface in diabetes mellitusKorean J Ophthalmol200418216817415635831
- NitodaEKallinikosPPallikarisACorrelation of diabetic retinopathy and corneal neuropathy using confocal microscopyCurr Eye Res2012371089890622632054
- MidenaEBruginEGhirlandoASommavillaMAvogaroACorneal diabetic neuropathy: A confocal microscopy studyJ Refract Surg2006229S1047S105217444092
- MessmerEMSchmid-TannwaldCZappDKampikAIn vivo confocal microscopy of corneal small fiber damage in diabetes mellitusGraefes Arch Clin Exp Ophthalmol201024891307131220490534
- GilbardJPDry eye, blepharitis and chronic eye irritation: divide and conquerJ Ophthalmic Nurs Technol199918310911510633658