Abstract
Background
The purpose of this study was to examine neodymium:yttrium-aluminum garnet (Nd:YAG) capsulotomy rates after combined cataract surgery with implantation of a three-piece 4% water content hydrophobic acrylic intraocular lens (X-70, Eternity®) and vitrectomy, and compare diabetic retinopathy with nondiabetic retinopathy.
Methods
Nd:YAG capsulotomy rates were evaluated for 72 eyes of 72 patients with diabetic retinopathy and 81 eyes of 81 patients with nondiabetic retinopathy (50 eyes with retinal detachment, 13 eyes with macular hole, nine eyes with epiretinal membrane, seven eyes with branch retinal vein occlusion, and two eyes with uveitis) who underwent combined cataract surgery and vitrectomy and implantation of X-70.
Results
Two years after combination surgery, four of 72 eyes (5.6%) in the diabetic retinopathy group and four of 81 eyes (5.0%) in the nondiabetic retinopathy group required Nd:YAG capsulotomies. Kaplan–Meier survival analysis showed no statistically significant differences between the two groups (P=0.30, Mantel–Cox log-rank test).
Conclusion
The rate of Nd:YAG capsulotomy did not significantly differ between diabetic retinopathy and nondiabetic retinopathy after combined cataract surgery with implantation of the X-70 and vitrectomy. X-70 is an acceptable intraocular lens for patients undergoing combined cataract surgery and vitrectomy.
Introduction
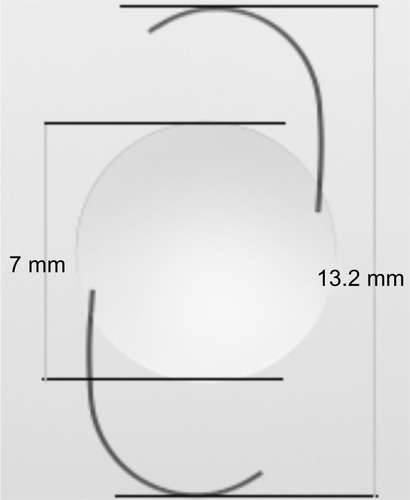
X-70 (Eternity®, Santen Co, Ltd, Osaka, Japan) is a new three-piece, 4% water content, hydrophobic acrylic intraocular lens composed of hydroxylethyl methacrylate, polyethylene glycol phenyl ether acrylate, and styrene cross-linked with ethylene glycol dimethacrylate.Citation1 X-70 has a square-edge design with an optic diameter of 7.0 mm and an overall diameter of 13.2 mm (). The large optic diameter provides stability and visibility during vitreoretinal surgery. The X-70 is often used for combined cataract surgery and vitrectomy in Japan.Citation2 In patients with diabetes mellitus, visualization and evaluation of the postoperative fundus is important in addition to visibility during surgery because of possible photocoagulation treatment requirements and reoperations.Citation3
Figure 1 X-70 (Eternity®, Santen Co, Ltd, Osaka, Japan) is a three-piece, 4% water content, and hydrophobic acrylic intraocular lens. X-70 has a square-edge design with an optic diameter of 7.0 mm and an overall diameter of 13.2 mm.
Posterior capsule opacification (PCO) is a common complication after cataract extraction with intraocular lens implantation,Citation4 which can result in decreased fundus visualization postoperatively. Previous reports have shown that PCO rates can greatly vary depending on the intraocular lens material,Citation5–Citation7 and PCO rates after combined cataract surgery and vitrectomy are considered higher than those after cataract surgery alone.Citation8 Neodymium:yttrium-aluminum garnet (Nd:YAG) capsulotomy is an effective treatment for PCO. However, this therapy has rare but significant complications,Citation9 so informed consent related to PCO is required prior to surgery.
We assumed that an investigation into Nd:YAG capsulotomy rates following implantation of the new acrylic intraocular lens, particularly in patients with diabetic retinopathy, would provide useful and important information. Thus, we conducted the current study to compare Nd:YAG capsulotomy rates in patients with diabetic and nondiabetic retinopathy after combined cataract surgery with implantation of the X-70 and vitrectomy.
Patients and methods
After obtaining institutional board approval, 153 eyes of 153 patients who underwent combined cataract surgery and vitrectomy at the Jikei University of Medicine Katsushika Medical Center between January 2009 and March 2011 were retrospectively reviewed. All patients were followed up for at least 2 years after surgery. Patients were divided into two groups, ie, a diabetic retinopathy group including 72 eyes of 72 patients and a nondiabetic retinopathy group including 81 eyes of 81 patients. Indications for surgery in the diabetic retinopathy group were proliferative diabetic retinopathy and those in the nondiabetic retinopathy group were retinal detachment (n=50), macular hole (n=13), epiretinal membrane (n=9), branch retinal vein occlusion (n=7), and uveitis (n=2). Exclusion criteria were previous intraocular surgery, trauma, silicon oil tamponade, scleral buckle, incomplete continuous curvilinear capsulorhexis, rupture of the posterior capsule, and further surgery.
All surgeries were performed by a single surgeon (YK). After a 5.5–6 mm continuous curvilinear capsulorhexis, a 3.2 mm wide and 1.5 mm long corneoscleral incision was created at the upper limbus, followed by phacoemulsification, cortex removal, and polishing of the posterior capsule. Vitrectomy was performed using a standard three-port pars plana vitrectomy technique with a 23-gauge system. The X-70 was implanted in a capsular bag after vitrectomy was completed.
PCO was identified using slit-lamp examination, grading density of the opacification from 0 to 4 (0, none; 1, minimal; 2, mild; 3, moderate; 4, severe) by the same surgeon (YK). An Nd:YAG capsulotomy was performed based on the presence of ≥grade 2 opacity and subjective patient complaints of decreased visual acuity compared with best postoperative visual acuity.Citation10
Kaplan–Meier survival distribution plots were generated to display the time of Nd:YAG capsulotomy events, and the Mantel–Cox log-rank test was used. Comparisons were considered to be statistically significant if the P-value was less than 0.05. All analyses were performed with GraphPad Prism version 6 software (GraphPad Software, Inc., San Diego, CA, USA).
Results
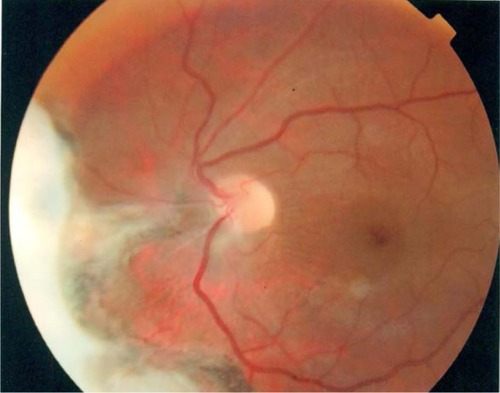
Two years after the combination surgery, four of 72 eyes (5.6%) in the diabetic retinopathy group and four of 81 eyes (5.0%) in the nondiabetic retinopathy group (three eyes with retinal detachment and one eye with branch retinal vein occlusion) required Nd:YAG capsulotomies. In total, eight of 153 (5.2%) eyes required Nd:YAG capsulotomies after combination surgery and implantation of X-70. The average patient age was 61±11 years in the diabetic retinopathy group and 62±10 years in the nondiabetic retinopathy group. There were 53 males and 19 females in the diabetic retinopathy group, and 45 males and 36 females in the nondiabetic retinopathy group. No statistically significant difference was observed between the two groups based on Kaplan–Meier survival estimates (P=0.30, ).
Figure 2 Kaplan–Meier survival distribution plots are generated to display the time of Nd:YAG capsulotomy events.
Abbreviation: Nd:YAG, neodymium:yttrium-aluminum garnet.
Discussion
Toda et al reported that the PCO rate did not significantly differ between diabetic and nondiabetic retinopathy groups after combined cataract surgery and vitrectomy.Citation8 Similarly, our results did not suggest diabetes mellitus as a significant risk factor associated with a higher Nd:YAG capsulotomy rate. Previous reports have indicated that patients with diabetes mellitus have significantly higher Nd:YAG capsulotomy rates than those without diabetes mellitus after single cataract surgery.Citation11,Citation12 Blood-aqueous barrier breakdown is reportedly more severe in the eyes of patients with diabetes mellitus,Citation13 and some chemical mediators stimulate the proliferation of lens epithelial cells that may lead to extensive PCO.Citation14,Citation15 A high rate of Nd:YAG capsulotomy after combined cataract surgery and vitrectomy has also been previously reported.Citation16,Citation17 Although we could not directly compare these reports because of the different types of intraocular lens, these accounts attributed the high rate of Nd:YAG capsulotomy to the use of silicone oil and further surgery, the absence of which may account for the fact that we found no statistically significant difference between diabetic and nondiabetic retinopathy groups.
Nishi et al reported that capsular bend formation by the intraocular lens with a square-edge design inhibits migration of lens epithelial cells, thereby decreasing the Nd:YAG capsulotomy rate.Citation18 However, Toda et al reported that there is a slight posterior pressure in eyes with no vitreous after vitrectomy; thus, it is possible that the intraocular lens edge effect in reducing PCO is minimal.Citation8 Previously reported Nd:YAG capsulotomy rates range from 3.6% to 7.5% among several hydrophobic three-piece acrylic intraocular lens with square-edge design, at 2 years after single cataract surgery.Citation7,Citation9,Citation19 Our results regarding implanted X-70 intraocular lenses are comparable with those of previous reports. We hypothesized that the inflammation and slight posterior pressure in eyes due to vitrectomy was responsible for high Nd:YAG capsulotomy rates. Previous reports have shown that the intraocular lens material plays a prominent role in preventing PCO, and the acrylic intraocular lens is associated with a significantly reduced degree of PCO.Citation6,Citation7 Our results suggest that the X-70 intraocular lens may have the potential for enhanced PCO prevention.
A limitation of our study was the use of Nd:YAG capsulotomy as a measurement of PCO. Criteria for Nd:YAG capsulotomy is subjective and largely based on patient complaints. If patients do not complain of low visual acuity (despite existence of severe PCO), Nd:YAG capsulotomy is not performed. Future studies with objective PCO measurement are definitely essential.
In conclusion, the rate of Nd:YAG capsulotomy did not significantly differ between the diabetic retinopathy group and the nondiabetic retinopathy group after combined cataract surgery with implantation of the X-70 and vitrectomy. The choice of an intraocular lens based on prevention of PCO is important. Our study suggests that the X-70 may have the potential for enhanced PCO prevention and be an acceptable intraocular lens for patients with different causes undergoing combined cataract surgery and vitrectomy.
Disclosure
No author has a financial and proprietary interest in this study.
References
- OllertonAWernerLFullerSRKavoussiSCMcIntyreJSMamalisNEvaluation of a new single-piece 4% water content hydrophobic acrylic intraocular lens in the rabbit modelJ Cataract Refract Surg201238101827183222920504
- WakabayashiMImaiAKitazawaNThe merits of 7.0 mm optics intraocular lens in phacovitrectomyJapanese Journal of Ophthalmic Surgery2010231121124 Japanese
- EbiharaYKatoSOshikaTYoshizakiMSugitaGPosterior capsule opacification after cataract surgery in patients with diabetes mellitusJ Cataract Refract Surg20063271184118716857507
- AppleDJSolomonKDTetzMRPosterior capsule opacificationSurv Ophthalmol1992372731161455302
- HollickEJSpaltonDJUrsellPGPandeMVLens epithelial cell regression on the posterior capsule with different intraocular lens materialsBr J Ophthalmol19988210118211889924308
- UrsellPGSpaltonDJPandeMVRelationship between intraocular lens biomaterials and posterior capsule opacificationJ Cataract Refract Surg19982433523609559471
- RamJKumarSSukhijaJSeveriaSNd:YAG laser capsulotomy rates following implantation of square-edged intraocular lenses: polymethyl methacrylate versus silicone versus acrylicCan J Ophthalmol200944216016419491949
- TodaJKatoSOshikaTSugitaGPosterior capsule opacification after combined cataract surgery and vitrectomyJ Cataract Refract Surg200733110410717189803
- MianSIFahimKMarcovitchAGadaHMuschDCSugarANd:YAG capsulotomy rates after use of the AcrySof acrylic three piece and one piece intraocular lensesBr J Ophthalmol200589111453145716234452
- KohnenTFabianEGerlROptic edge design as long-term factor for posterior capsular opacification ratesOphthalmology200811581308131418321585
- IonidesADowlerJGHykinPGRosenPHHamiltonAMPosterior capsule opacification following diabetic extracapsular cataract extractionEye (Lond)19948Pt 55355377835448
- HayashiKHayashiHNakaoFHayashiFPosterior capsule opacification after cataract surgery in patients with diabetes mellitusAm J Ophthalmol20021341101612095802
- MoriartyAPSpaltonDJMoriartyBJShillingJSFfytcheTJBulsaraMStudies of the blood-aqueous barrier in diabetes mellitusAm J Ophthalmol199411767687718198161
- IbarakiNLinLRReddyVNEffects of growth factors on proliferation and differentiation in human lens epithelial cells in early subcultureInvest Ophthalmol Vis Sci19953611230423127558725
- NishiONishiKFujiwaraTShirasawaEOhmotoYEffects of the cytokines on the proliferation of and collagen synthesis by human cataract lens epithelial cellsBr J Ophthalmol199680163688664236
- PinterSMSugarAPhacoemulsification in eyes with past pars plana vitrectomy: case-control studyJ Cataract Refract Surg199925455656110198863
- GrushaYOMasketSMillerKMPhacoemulsification and lens implantation after pars plana vitrectomyOphthalmology199810522872949479289
- NishiONishiKManoCIchiharaMHondaTThe inhibition of lens epithelial cell migration by a discontinuous capsular bend created by a band-shaped circular loop or a capsule-bending ringOphthalmic Surg Lasers19982921191259507255
- AppleDJPengQVisessookNEradication of posterior capsule opacification: documentation of a marked decrease in Nd:YAG laser posterior capsulotomy rates noted in an analysis of 5416 pseudophakic human eyes obtained postmortemOphthalmology2001108350551811237905