Abstract
Purpose
To measure thrombopoietin (TPO) levels in the serum and aqueous humors of patients with noninfectious acute anterior uveitis.
Methods
A prospective, comparative, controlled study. Serum and aqueous humors were obtained from the eyes of 16 patients with noninfectious acute anterior uveitis. TPO levels were measured using an enzyme-linked immunosorbent assay (ELISA). The results obtained were compared with those of a control group.
Results
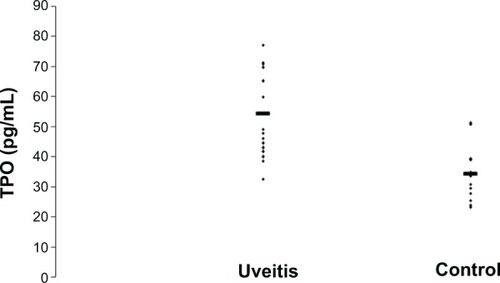
Serum concentrations of TPO were not significantly different between control individuals and patients with active anterior uveitis. Aqueous humor TPO levels were 54.46±16.24 pg/mL in the eyes of patients with uveitis, and 34.32±11.63 pg/mL in the eyes of controls. The difference between the two groups was significant (Mann–Whitney U-test for independent data, P=0.0008), with uveitis patients exhibiting significantly higher levels of TPO.
Conclusion
The high levels of TPO in the aqueous humors of uveitis patients points toward a cytoprotective role of this factor in inflammatory repair processes and the recovery of tissue homeostasis.
Introduction
The annual incidence of anterior uveitis in the United States is 8 per 100,000 inhabitants.Citation1 Its origin is generally idiopathic; the event or agent that triggers the inflammation is unknown.Citation1 There is no direct evidence that noninfectious anterior acute uveitis is an autoimmune disease, but various environmental and genetic stimuli, along with innate and adaptive immune responses, relate to this type of uveitis. Some cytokines are found in the eyes and peripheral blood of patients with uveitis.Citation2–Citation5 Some recent studies have reported increased levels of cell growth factors, such as pigment epithelium derived factor (PEDF)Citation6–Citation8 and vascular endothelial growth factor (VEGF), in the aqueous humors of patients with uveitis – both with and without macular edema, and even during periods of disease inactivity.Citation9,Citation10
Cell growth factors control cell growth and differentiation; regulating development and cell survival. They perform a crucial role in controlling cell proliferation. Alterations in signaling mediated by growth factors may be related to several inflammatory diseases. They also mutually interact to promote various healing or cell proliferation processes.Citation11–Citation18
Thrombopoietin (TPO) is a growth factor synthesized mainly in the liver. It is the main regulator of the proliferation and maturation of megakaryocytes and of the production of platelets, by which hematopoietic stem cells are regulated. It is also a positive vasculogenesis regulator,Citation19–Citation21 and its relationship with VEGF has been shown to be essential for stem cells, inducing their production and specifically promoting the production of two VEGF-A isoforms, VEGF121 and VEGF165 isoforms. VEGF also modulates the effects of TPO on hematological stem cells in an autocrine loop.Citation22 It has also been implicated in the pathophysiology of multiple inflammatory and immunoallergic conditions such as allergic asthma or inflammatory bowel disease, in which it appears to play a significant immunoregulatory role.Citation23,Citation24 Studies with experimental mice models have demonstrated that VEGF acts as an acute-phase protein, and that its synthesis is induced by interleukin (IL)-6.Citation25 However, no studies of TPO levels in the aqueous humors of patients with uveitis have been reported to date.
This factor has been implicated in the pathophysiology of multiple inflammatory and immunoallergic conditions, where it could play an immunoregulatory role. The objective of the present study was to quantitatively measure TPO levels in the aqueous humors of patients with noninfectious acute anterior uveitis to establish whether or not they are impaired in these conditions.
Materials and methods
This is a single-center, non-randomized, controlled, prospective, observational, comparative case study which evaluates TPO levels in the serum and aqueous humors of patients with noninfectious anterior uveitis referred to the Uveitis Unit of the Department of Ophthalmology of the Hospital Universitario La Fe (Valencia, Spain), a center of national reference for the study and treatment of this condition. Controls were obtained from the serum and aqueous humors of patients who were due to have cataract surgery, and who had no history of intraocular inflammatory disease, systemic disease or long-term drug therapy.
The study protocol met the requirements of the Declaration of Helsinki, and was reviewed and approved by the Ethics Committee of the Hospital Universitario La Fe. Informed consent was obtained from all participants and specified the reason for the study.
The patient inclusion and exclusion criteria for the study were as follows:Citation26
Inclusion criteria:
Diagnosis of classic acute anterior uveitis.
Untreated patients in the first episode of classic anterior uveitis, within the first 2–7 days of symptomatology. Eye inflammation (slit lamp microscopy grading of cells) rated moderate to severe (grade 2 to 4) according to the criteria of the International Ocular Inflammation Society and the Standardization Uveitis Nomenclature.Citation26,Citation27
Exclusion Criteria:
Diagnosis of hypertensive or granulomatous uveitis.
Specific clinical conditions, including Fuchs heterochromic iridocyclitisor Posner-Schlossman syndrome, uveitis caused by herpes, or toxoplasma in the aqueous humor sample, revealed by polymerase chain reaction (PCR).
Eye surgery in the 6 months prior to obtaining the sample.
Serology positive for HIV, syphilis or sarcoidosis (the latter revealed by angiotensin converting enzyme serum detection).
Cystoid macular edema, detected using optical coherence tomography (OCT).
Associated systemic diseases in the clinical history or revealed by clinical-radiological examination, or by HLA-B27 test.
Serum was obtained from peripheral blood of patients and controls.
Anterior chamber paracentesis prophylaxis, consisting of topical application of ofloxacin eye drops for three days, was performed before and after removal of aqueous humors. Immediately before removal, iodinated povidone in an ophthalmic dilution was applied to the conjunctival sac.Citation28 Paracentesis for sampling was performed at the clinic with a 30 G needle, with the aid of a slit lamp. Samples of at least 0.05–0.2 mL of aqueous humor were collected from each patient, and placed in sterile tubes and were stored immediately at −80°C for subsequent processing. The specimens were classified and labeled in a masked fashion. All specimens were assayed for TPO in a double-blind arrangement with respect to their group. In the control group, composed of patients due to undergo cataract surgery, aqueous humors were removed immediately prior to surgery. The control group was age-matched with the uveitis group.
Quantitative measurement of protein concentrations in serum and aqueous humor samples was performed using the enzyme-linked immunosorbent assay (ELISA), marketed by Searchlights Human Angiogenesis Array® (Pierce Biotechnology, Inc., Rockford, IL, USA).
The TPO value in standard curves was in the range of 12–3,000 pg/mL and the sensitivity of TPO measurement was 5.9 pg/mL. All procedures were performed on the same day, and according to the manufacturer’s instructions.
The demographic data of the subjects were analyzed using the Windows statistical package SPSS Statistics for Windows, Version 19.0 (IBM Corp., Armonk, NY, USA). The Mann–Whitney U-test for independent data was used to compare TPO levels in the groups, accepting P<0.05 as a significant value.
Results
A total of 32 serum and aqueous humor samples were obtained from 16 patients with uveitis (nine male and seven female), and 16 controls (ten male and six female). All patients were Caucasian. No statistically significant differences were detected between the mean ages of the patients with uveitis (mean ± standard deviation [SD]; 51.6±12.5 years, range 35–79 years), and controls (59.2±11.2 years, range 44–79 years), Student’s t-test for independent data, P=0.08.
With respect to the control group, the sensitivity of the ELISA test used was 5.9 pg/mL. shows the values obtained for TPO levels according to the ELISA technique in both groups. The mean TPO level measured in serum samples was 35.4±12.94 pg/mL (range 21.1–61.2 pg/mL) in patients with uveitis, and 32.87±9.8 pg/mL (range 15.3–50.7 pg/mL) in controls. No statistically significant difference was found between the control group and the individualized patients with anterior uveitis (Mann–Whitney U-test, P=0.82).
Table 1 TPO levels in the serum and aqueous humor of uveitis patients and the control group measured by enzyme-linked immunosorbent assay, presented along with the age and sex of subjects
The mean TPO level measured in the aqueous humor samples was 54.46±16.24 pg/mL (range 32.50–86.30 pg/mL) in patients with uveitis, and 34.32±11.63 pg/mL (range 14.80–51.20 pg/mL) in controls. A significant difference was found between the two groups (Mann–Whitney U-test, P=0.0008), with the patients with uveitis exhibiting significantly higher levels of TPO than the control group ().
Figure 1 Thrombopoietin (TPO) levels in the aqueous humors of 16 patients with uveitis and 16 controls.
Discussion
The observation of higher levels of TPO in patients with noninfectious acute anterior uveitis raises questions relating to the cause and possible consequences of this condition.
Although TPO plays an important multifunctional regulatory role in hematopoiesis and vasculogenesis that is closely related to VEGFCitation29 there are many data that also relate it to inflammatory conditions. TPO is activated through the release of various proinflammatory cytokines, such as IL-1, IL-3, IL-6 and IL-11. These proinflammatory cytokines play a critical role in the triggering and development of multiple autoimmune conditions caused by dysregulation of the autoimmune response. All these cytokines interfere actively with cell immune and biochemical mediators at many levels. The regulation of this proinflammatory activity appears to be mediated by anti-inflammatory and immunosuppressive cytokines, such as IL-4, IL-10 or transforming growth factor (TGF)-β.Citation30 There are several reports of a significant increase in the expression of the TPO gene under inflammatory conditions, which suggests that it acts as an acute-phase protein.Citation31 It is also established that the synthesis of TPO in the liver can be induced by IL-6, while IL-6 stimulates thrombopoiesis through the action of TPO, and that the reactive thrombocytosis associated with some inflammatory conditions is mediated by IL-6 through the action of TPO.Citation32–Citation34 A significant correlation between IL-6 and TPO is evident in the fact that the administration of IL-6 in patients with cancer produces an increase in TPO serum levels.Citation35
Positive correlations have been found between TPO and C-reactive protein (CRP), but do not appear to affect platelet count. TPO acts as an acute-phase protein, and appears to be closely related to the action of IL-6 in inflammatory conditions.Citation36,Citation37
In some inflammatory diseases, such as Schönlein–Henoch disease, an increase in TPO has also been described along with IL-6, which is thought to be an acute-phase reactant; in fact, a secondary increase in the production of TPO has been reported in this condition.Citation38 TPO increases related to IL-6 have also been reported in the coronary disease inflammatory condition.Citation39
The regulatory function of TPO has also been described in the differentiation of mast cells and its increase in patients with allergic asthma, which points to its involvement in immunoallergic conditions.Citation21,Citation22,Citation40,Citation41 The importance of platelets as major agents in the defense against infection and the induction of tissue inflammation and repair has been confirmed.Citation42 Increases of IL-6 and TPO in the plasma of patients with inflammatory bowel disease and in sufferers of rheumatoid arthritis have also been documented.Citation42,Citation43
This body of evidence suggests that the increase of TPO – characteristic of uveitis, is associated with increments of other growth factors present in the aqueous humors of patients with this inflammatory condition, such as PEDF and VEGF.Citation6–Citation9
Compared to the control group, TPO levels in the aqueous humor in patients with noninfectious acute anterior uveitis were significantly higher, but there was no difference detected between plasma levels of TPO in patients vs controls.
We cannot directly determine the source of TPO in aqueous humors, but we think it is possible that its increase is not a result of the rupture of the blood–aqueous barrier, but rather derived from an increase in local production. It would be important to know whether this may be related to the pathophysiology of the disease, either as a cause or consequence, since many studies have shown that TPO expression increases during many inflammatory processes. Further studies are required to consider this possibility.
On the other hand, we should also contemplate the consequences that this increase in TPO may cause in the outcome of uveitis. Several studies in experimental models of autoimmune anterior uveitis have suggested that apoptosis plays a significant role in the resolution of uveitis, since apoptosis followed by phagocytosis is critical in the reduction of cell infiltration and subsequent resolution of the condition.Citation44–Citation49
In addition, other studies have related an increase in TPO to the inflammatory changes occurring in some central nervous system (CNS) infections, suggesting a proapoptotic activity and a different regulation of production in the CNS to that in the liver, where it mostly occurs.Citation50,Citation51
One possible clinical application of this increase in TPO is its use in the modulation or resolution of uveitis. Indeed, unlike other growth factors, it is already commercially available.Citation52
The statistically significant increase (P>0.001) of the cell growth factor TPO in the aqueous humors of patients with noninfectious acute anterior uveitis indicates an involvement of this factor in this ocular inflammatory condition, perhaps as a mechanism of the repair process and linked to apoptosis. Any further knowledge of this and other cell growth factors is likely to lead to a better understanding of the pathophysiology of uveitis and other inflammatory conditions of the eye, and will no doubt be of great help in designing new therapeutic approaches involving new molecules, such as Romiplostim or Eltrombopag, which mimic the effect of TPO.Citation53,Citation54
In conclusion, the enhanced levels of TPO in the aqueous humor of patients with uveitis observed in this study lead us to support a cytoprotective role of this factor in inflammatory repair processes and the recovery of tissue homeostasis.
Disclosure
The authors have no conflicts of interest in this work.
References
- ReevesSWSloanFALeePPJaffeGJUveitis in the elderly; epidemiological data from the National Long-term care Survey Medicare cohortOphthalmology200611330732116406541
- ReadSMauzeSAssemanCCD38+CD45RB (low) CD4+ T cells: a population of T cells with immune regulatory activities in vitroEur J Ophthalmol19982834353437
- DickADImmune mechanism of uveitis: insights into disease and pathogenesis and treatmentInt Ophthalmol Clin20004011810791254
- CurnowSJFalcianiFDurraniOMMultiplex bead immunoassay analysis of aqueous humor reveals distinct cytokine profiles in uveitisInvest Ophthalmol Vis Sci2005464251425916249505
- SimonDDennistonAKTomlinsPJSoluble gp130, an antagonist of IL-6 transsignaling, is elevated in uveitis aqueous humorInvest Ophthalmol Vis Sci2008493988399118469182
- CurnowSJMurrayPIInflammatory mediators of uveitis: cytokines and chemokinesCurr Opin Ophthalmol200617653253717065921
- YoshidaYYamagishiSMatsuiTPositive correlation of pigment epithelium derived factor and total antioxidant capacity in aqueous humor of patients with uveitis and proliferative diabetic retinopathyBr J Ophthalmol2007911133113417389742
- YoshidaYYamagishiSMatsuiTIncreased levels of pigment epithelium derived factor in aqueous humor of patients with uveítisBr J Ophthalmol20079114915016973658
- FineHFBaffiJReedGFCsakyKGNussenblattRBAqueous humor and plasma vascular endothelial growth factor in uveitis-associated cystoids macular edemaAm J Ophthalmol200113279479611704050
- ParoliMPTeodoriCD’AlessandroMMarianiPIannucciGParoliMIncreased vascular endothelial growth factor levels in aqueous humor and serum of patients with quiescent uveitisEur J Ophthalmol20071793894218050120
- AraiKLeeFMiyajimaSMiyatakeNCytokines; Coordinators of immune and inflammatory responsesAnn Rev Biochem1990597838361695833
- YanaiRYamadaNMitogenic and antiapoptotic effects of various growth factors on human corneal fibroblastsInvest Ophthalmol Vis Sci2002432122212612091406
- RobertsABThe ever-increasing complexity of TGF-β signalingCytokine Growth Factor Rev2002133511750874
- KuhlPRGriffith-CimaGTethered epidermal growth factor as a paradigm for growth factor-induced stimulation from the solid phaseNat Med19962102210278782461
- DinbergsIDBrownLCellular response to transforming growth factor 1 and basic fibroblast growth depends on release kinetics and extracellular matrix interactionsJ Biol Chem199627129822298298939921
- NathanCSpornMCytokines in contextJ Cell Biol19911139819862040651
- MaldonadoBFurchtLTEpidermal growth factor stimulates integrin-mediated cell migration of cultured human corneal epithelial cells on fibronectin and arginineglycine-aspartic acid peptideInvest Ophthalmol Vis Sci199536212021267544783
- ImanishiJKamiyamaKGrowth factors: importance in wound healing and maintenance of transparency of the corneaProg Retin Eye Res20001911312910614683
- WillmJAkkermanNThrombopoietin and platelet functionSemin Thromb Hemost20063229530416673285
- BegleyCGBasserRLBiologic and structural differences of thrombopoietin growth factorsSemin Hematol200037192710831285
- KuterDJBegleyCGRecombinant human thrombopoietin basic biology and evaluation of clinical studiesBlood200210035473569
- KaushanskyKThrombopoietin and the hematopoietic stem cellAnn NY Acad Sci2005104413914115958707
- Kemona-ChetnikIBodzenta-LukaszykAButkiewiczADymnicka-PiekarskaVKemonaHThrombocytopoiesis in allergic asthmaPol Arch Med2007117913
- HeitsFStahlMLudwigDStangeEFJelkmannWElevated serum thrombopoietin and intreleukin-6 concentrations in thrombocytosis associated with inflammatory bowel diseaseJ Interferon Cytokine Res19991975776010454346
- BurmesterHWolberEMFreitagPFandreyJJelkmannWThrombopoietin production in wild-type and interleukin-6 knockout mice with acute inflammationJ Interferon Cytokine Res20052540741316022585
- Bloch-MichelENussenblattRBInternational uveitis study group recommendations for the evaluations of intraocular inflammatory diseaseAm J Ophthalmol19871032342353812627
- JabsDANussenblattJTThe standardization of uveitis nomenclature (SUN) Working group. Standardization of uveitis nomenclature for reporting clinical data. Results of the first international workshopAm J Ophthalmol200514050951616196117
- CheungCMGDurraniOMMurrayPIThe safety of anterior chamber paracentesis in patients with uveitisBr J Ophthalmology200488582583
- EguchiMMasudaHKwonSLesion-targeted thrombopoietin potentiates vasculogenesis by enhacing motility and enlivenment of transplanted endothelial progenitor cells via activation of Akt/mTOR/p70s6kinase signaling pathwayJ Mol Cell Cardiol20084566166918773906
- KimEYMoudgilKDRegulation of autoimmune inflammation by pro-inflammatory cytokinesImmunol Lett20081201518694783
- CeruttiACustodiPDurantiMNorisPBalduiniCLThrombopoietin levels in patients with primary and reactive thrombocytosisBr J Haematol1997992812849375739
- BurmesterHWolberEMFreitagPThrombopoietin production in wild-type and interleukin-6 knockout mice with acute inflammationJ Interferon Cytokine Res20052540741316022585
- KaserABrandacherGSteurerWInterleukin-6 stimulates thrombopoiesis through thrombopoietin: role in inflammatory thrombocytosisBlood2001982720272511675343
- CeresaIFNorisPAmbaglioCThrombopoietin is not uniquely responsible of thrombocytosis in inflammatory disordersPlatelets20071857958218041648
- HollenCWHenthornJKoziolJAElevated serum interleukin-6 levels in patients with reactive thrombocytosisBr J Haematol1991792862901958487
- CeruttiACustodiPDurantiMCazzolaMBalduiniCLCirculating thrombopoietin in reactive conditions behaves like an acute phase reactantClin Lab Haematol19992127127510583330
- IshiguroASuzukiYMitoMElevation of serum thrombopoietin precedes thrombocytosis in acute infectionsBr J Haematol200211661261811849220
- LinCYYangYHLeeCCHuangCLWangLCChiangBLThrombopoietin interleukin-6 levels in Henoch-Schönlein purpuraJ Microbiol Immunol Infect20063947648217164950
- CottonJMHongYHaweERise of circulating thrombopoietin following cardiothoracic surgery is potentiated in patients with coronary atherosclerosis: correlation with a preceding increase in levels of interleukin-6Thromb Haemost20038953854312624639
- WolberEMFandreyJFrackowskiVJelkmannWHepatic thrombopoietin mRNA is increased in acute inflammationThromb Haemost2001861421142411776309
- MigliaccioARRole of thrombopoietin in mast cell differentiationAnn NY Acad Sci20072715217417468237
- KlingerMHJeikmannWRole of blood platelets in infection and inflammationJ Interferon Cytokine Res20072291392212396713
- HeitsFStahlMLudwigDStangeEFJelkmannWElevated serum thrombopoietin and intreleukin-6 concentrations in thrombocytosis associated with inflammatory bowel diseaseJ Interferon Cytokine Res19991975776010454346
- YuHGChungHLeeWJApoptosis of CD4+ T cells occurs in experimental autoimmune anterior uveitis (EAAU)Clin Exp Immunol199911835736310594552
- YangPHerzbergNHZhouHBroersmaLde SmetMKijlstraAApoptosis of infiltrating cells in experimental autoimmune uveoretinitisChin Med J (Engl)200011364364611776038
- PoulakiVMitsiadesNMastorakosGCaspiRRChrousosGPBouzasEFas/Fas ligand-associated apoptosis in experimental autoimmune uveoretinitis in rodents: role of proinflammatory corticotropin-releasing hormoneExp Eye Res20017262362911384150
- SmithJRHartPHStandfieldSDCosterDJWingSJWilliamsKAApoptosis is a prominent feature of acute anterior uveitis in the Fischer 344 ratBr J Ophthalmol20008420521110655199
- LiQSunBMattesonDMO’BrienTPChanCCCytokines and apoptotic molecules in experimental melanin-protein induced uveitis (EMIU) and experimental autoimmune uveoretinitis (EAU)Autoimmunity19993017118210520900
- JhaPMattaBLyzogubovLTytarenkoRBoraPSBoraNSCrucial role of apoptosis in the resolution of experimental autoimmune anterior uveitisInvest Ophthalmol Vis Sci2007485091510017962461
- ReinholAZhangJGessnerRFelderhoff-MueserUObladenMDameCHigh thrombopoietin concentration in the cerebrospinal fluid of neonate with sepsis and intraventricular hemorrhage may contribute to brain damageJ Interferon Cytokine Res20072713714517316141
- ErtenliIKirazSOztúrkMAHaznedarogluICelikICalgüneriMPathologic thrombopoiesis of rheumatoid arthritisRheumatol Int200323495012634936
- StasiREvangelistaMLAmadoriSNovel thrombopoietic agents: a review of their use in idiopathic thrombocytopenic purpuraDrugs20086890191218457458
- HaznedarogluICGokerHTurgutMBuyukasikYBenekliMThrombopoietin as a drug: biological expectations, clinical realities, and future directionsClin Appl Thrombosis/Hemostasis20028193212
- WadhwaMThorpeRHaematopoietic growth factors and their therapeutic useThromb Haemost20089986387318449415
