Abstract
Background
Multifocal glasses (bifocals, trifocals, and progressives) increase the risk of falling in elderly people, but how they do so is unclear. To explain why glasses with progressive addition lenses increase the risk of falls and whether this can be attributed to false projection, this study aimed to 1) map the prismatic displacement of a progressive lens, and 2) test whether this displacement impaired reaction time and accuracy.
Methods
The reaction times of healthy ≥75-year-olds (31 participants) were measured when grasping for a bar and touching a black line. Participants performed each test twice, wearing their progressives and new, matched single vision (distance) glasses in random order. The line and bar targets were positioned according to the maximum and minimum prismatic displacement effect through the progressive lens, mapped using a focimeter.
Results
Progressive spectacle lenses have large areas of prismatic displacement in the central visual axis and edges. Reaction time was faster for progressives compared with single vision glasses with a centrally-placed horizontal grab bar (mean difference 101 ms, P=0.011 [repeated measures analysis]) and a horizontal black line placed 300 mm below center (mean difference 80 ms, P=0.007). There was no difference in accuracy between the two types of glasses.
Conclusion
Older people appear to adapt to the false projection of progressives in the central visual axis. This adaptation means that swapping to new glasses or a large change in prescription may lead to a fall. Frequently updating glasses may be more beneficial.
Introduction
Based on World Health Organization statistics, falls are the second leading cause of unintentional injury-related deaths worldwide.Citation1 Around 424,000 people globally die every year from unintentional falls, second only to road traffic deaths. Injuries sustained from falls are unfortunately quite common in the elderly population; for instance, in the United Kingdom 57% of all injury-related hospitalizations in the elderly are related to falls.Citation2
Multifocal glasses in the form of bifocals have been available since 1784. Benjamin Franklin converted his glasses into bifocals, allowing him to see which French politician was speaking and at the same time eat his meal.Citation3 Multifocal glasses are convenient for activities such as cooking, shopping, and driving. However, multifocal glasses are a known contributor to falls in elderly people.Citation4 When multifocal glasses are worn while negotiating steps, in outdoor environments and around the home, they increase the chance of a fall. Given that 52% of elderly people wear multifocal glasses, a large proportion of falls may be preventable.Citation5 Why and how multifocal glasses increase falls is not completely understood. The reading portion may affect depth perception and contrast sensitivity;Citation4 additionally, the clear corridor of vision is smaller in progressives due to the large amounts of astigmatism at the edges.Citation6
Of particular interest is the prismatic displacement effect of multifocal glasses on correcting postural stability. Displacement of the image of an object when viewed through a prism and the illusion of false projection is due to the amount of prismatic displacement it creates. The amount a light ray will deviate when it passes through a prism depends on the apical angle, the index of refraction of the material (and the material surrounding it), the wavelength of the light, and the angle from which the light approaches the prism.Citation7 Although the prismatic displacement effect of multifocal glasses is alluded to as a potential cause of falls,Citation4,Citation8–Citation11 to our knowledge no one has tested this effect. The aim of this study was to 1) map the prismatic displacement of a progressive lens, and 2) test whether the displacement of a progressive addition lens (PAL) impairs reaction time and accuracy.
Methods
A case crossover trial was conducted in the School of Physiotherapy Balance Clinic at the University of Otago, Dunedin, New Zealand. Participants’ reaction times and accuracy were compared while wearing both PALs and single (distance) vision glasses. Initial investigation established where PALs had areas of largest displacement.
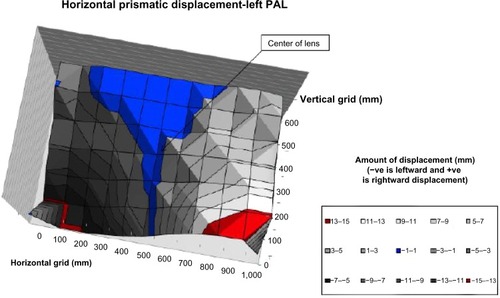
Preliminary investigation
Initial work illustrated the largest areas of prismatic displacement in a plano, +4 D powered PAL, which was mapped using the Nikon projection focimeter (Nikon Corporation, Tokyo, Japan). A +4 D lens was chosen so that the area(s) of maximal prismatic displacement was more apparent. A plastic “mask”, 40 mm in diameter, with a grid of holes 3 mm apart (each hole 1 mm in diameter and 2 mm deep), vertically and horizontally (seven by eleven holes, respectively) was placed on top of the PAL. shows the area of the PAL that was mapped and the prismatic displacement measurements that were recorded in diopters, and then converted to millimeters of displacement (diopter × 666/100= “mm of displacement”). Of note, the measure 666 is the distance in millimeters from the participant to the target they reached for in this study and the value 100 is a factor to convert the displacement to millimeters. Both the right and left PALs were measured and the right PAL was inverted and averaged with the left PALs’ results. The measurements showed that PALs had larger displacements at certain points. At the center of the lens the largest mean difference was 8.15 mm (95% confidence interval [CI] 6.54–9.75) of vertical displacement. At positions at the periphery of the glasses the difference was small, around 2.23 mm (95% CI 0.37–4.09) of horizontal displacement (at 200 mm below center) and 1.83 mm (95% CI 0.52–3.14) of vertical displacement (at 100 mm below center). There was no difference in horizontal displacement at the center and vertical displacement at 300 mm below center between the two glasses (P=0.271 and P=0.258), respectively ( and ).
Figure 1 A flight of stairs viewed through a left, plano + 4D power progressive lens.
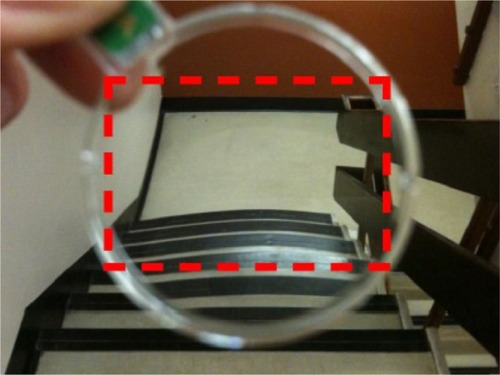
Figure 2 Vertical prismatic displacement measured by the focimeter.
Abbreviation: PAL, progressive addition lens.
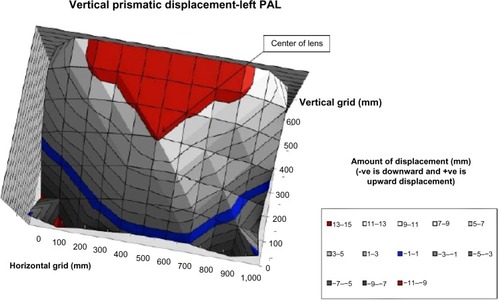
Figure 3 Horizontal prismatic displacement measured by the focimeter.
Abbreviation: PAL, progressive addition lens.
Study design
Community dwelling participants were recruited through optometric practices in Dunedin, New Zealand. Participants were residents 75-years-old or older from the Dunedin and Mosgiel communities who had acquired a new or updated prescription for a PAL within the last 12 months. The study received ethical approval from the Lower South Regional Ethics Committee.
Exclusion criteria were: 1) poorer than 6/12 vision in one eye or 6/12 with binocular vision when corrected with glasses;Citation12 2) ocular/retinal problems (ie, age-related macular degeneration, cataracts, diabetic retinopathy, glaucoma, field defects, and ocular-motor disorders); 3) >2 diopter difference of spherical anisometropia; 4) >4 diopter of oblique astigmatism; 5) deformities of the arms, neck, or head; 6) inability to stand; 7) suffering from dizziness or a recent injury or medical condition that affected coordination and ability to grasp; 8) not being able to understand the study requirements; and 9) a Mini Mental State Examination (MMSE)Citation13 score lower than 26.
Baseline information was collected from the participant’s optometrist’s notes and a home visit conducted by the investigator. Information was recorded about demographics, living arrangement, medical conditions, medication use, and visual acuity plus physical functioning. The order of the tests of the two types of glasses was randomized with the investigator blinded to the order; the position of the bar/black line at the maximal or minimal prismatic displacement was randomized. A statistician not involved with the study prepared a computer-generated randomization schedule and opaque envelopes with instructions for the order of glasses to be worn. The schedule was made available on testing day and explained to the participant by a person independent of the study, to preserve blinding of the investigator. Numbered tags were placed on the frames of each pair of glasses to allow the participant to wear the glasses in the correct order. Each pair of glasses were adjusted and measured so that the eye was 20 mm away from the vertex of the lens. The investigator restated the need for the participant to “refrain from describing the glasses as progressives or single distance” as it is imperative that the investigator did not know the order during and after the test.
It was not possible for an inexperienced observer to tell if the glasses were PALs or single vision glasses. Because of this the investigator remained blind to the subsequent analysis of the order of glasses. Any adjustment of the participant’s new single vision glasses frames occurred before blinding.
Single vision glasses
The participants acquired their single vision glasses on testing day so that they did not have time to adapt to this pair of glasses. Each new prescription of single vision glasses was identical and matched to the distance part of the individual’s PAL prescription and frame style. Where this was not possible due to a lack of supply, the make, model, size, and style of frame was matched as closely as possible to the participant’s chosen frame. The single vision glasses were not matched for scratch resistant lens coating and/or transitional tints, due to budget constraints. However, this was deemed unlikely to affect performance in the trials.
Outcomes
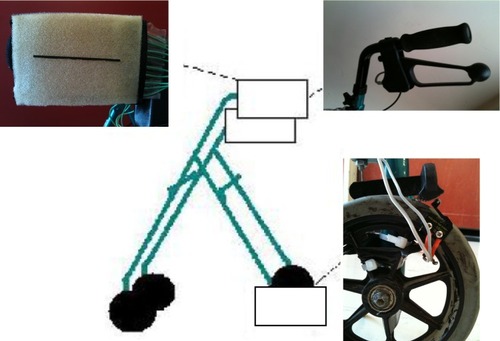
The PowerLab® 4SP data acquisition system and the Lab-Chart Pro® version 7 programCitation14 (ADInstruments, Dunedin, New Zealand) were used to measure reaction time and accuracy. Accuracy measurements were recorded using the LabChart® program mentioned and a series of nine wire switches under a foam pad (see ). The LabChart® program could measure which switch or switches were pushed first and therefore the distance from the black line (see ). The participant’s finger movements when pushing a black line on a foam pad were also recorded by a video camera behind the participant. Participants were asked to wear a hard collar fitted to their neck. This was done to ensure only their extraocular eye movements were used to visualize the bar/black line and light emitting diode (LED). Participants were asked to sit comfortably on a chair with their arms by their side in a neutral position and stare at an LED placed 1 meter in front of them. They were instructed to reach out with their dominant hand and grab the whole bar or push the black line with their index finger when the LED turned on, as quickly as possible. Enough strength to grip the bar or push the black line was needed to generate an input to the LabChart® and end the test. The bar/black line was placed horizontally and vertically in front and to the dominant hand side of the participant, at a distance of 666 mm. The bar and the black line were attached to a walking frame (Mobilis® Quad [Cubro Ltd, Tauranga, New Zealand], see ). The areas of visual fixation through the glasses were based on the focimeter results from the preliminary investigation, which showed the areas of maximal and minimal prismatic displacement. The coordinates (500, 300), (100, 100), (100, 200), (900, 100), (900, 200), and (500, 0) from and indicate where participants fixated through their glasses on the bar/black line. The bar/black line was placed at the horizontal and vertical center of the lens (500, 300). The bar/black line was placed vertically only at coordinate (100, 100) or (900, 100) depending on the participant’s dominant hand; this position was 35° peripherally and 200 mm below center. The bar was placed horizontally at coordinate (100, 200) or (900, 200), once again depending on the participant’s dominant hand; this position was 35° peripherally and 100 mm below center. Finally, the black line was placed horizontally at coordinate (500, 0), which was 300 mm below center. The main outcome was reaction time when grasping the bar and reaction time plus accuracy when pushing the black line at different points of fixation through the glasses. Each test was repeated three times and the fastest time plus its associated accuracy were used in the analyses.
Figure 4 A diagram that represents the equipment used to measure accuracy.
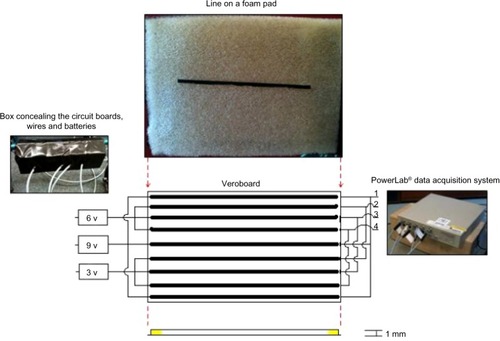
Figure 5 LabChart® display window.
Abbreviation: v, voltage.
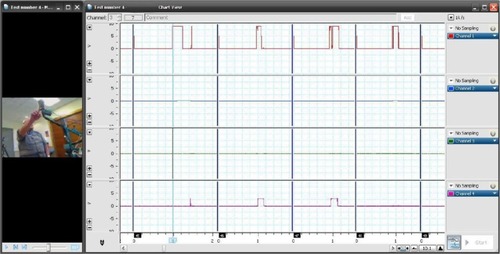
Figure 6 Diagram illustrating the Mobilis® Quad walking frame in the center and the three major components attached to the frame.
Statistical analysis
Data were analyzed using the Statistical Package for the Social Sciences version 18 (IBM Corporation, Armonk, NY, USA) and presented as mean (standard deviation [SD]), mean difference (95% confidence interval [CI]), or number (percentage). To test whether measures of reaction time differed between the two types of glasses, repeated measures analysis of variance and covariance were used, controlling for length of time since updating their glasses, prismatic displacement, and order of glasses. Accuracy measurements were compared for the two types of glasses using the chi-squared McNemar test. The LabChart® measurements were verified from the video recordings, to confirm whether the participant pushed the black line. The prismatic displacement measures were analyzed using paired t-tests.
Results
Thirty-one participants were recruited for the study (see ) and their characteristics are summarized in .
Figure 7 Participant recruitment.
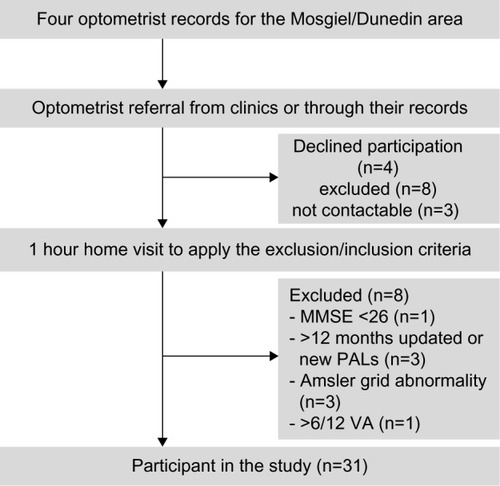
Table 1 Characteristics of participants (n=31), where values are numbers (percentages) unless otherwise stated
When wearing PALs, participants had a significantly faster reaction time compared to when they were wearing single vision glasses. This improved reaction time was noted when localizing the bar/line through two areas: 1) at the center of the lens, when grasping a horizontal bar, PALs were faster by 101 ms, P=0.011 (repeated measures for order effect, time to update their PALs, and prismatic displacement); 2) at 300 mm below center, when pushing a horizontal black line, PALs were faster by 80 ms, P=0.007. This study found no statistically significant differences for reaction time for pushing a black line and grasping a bar at the other positions tested, fixating through the two different glasses (see ). and represent graphical interpretations of the reaction time measurements and illustrate the significant differences between the two glasses in the central visual axis.
Figure 8 Reaction time measurements for grasping a bar at the various points of fixation while wearing the two glasses.
Abbreviation: PALs, progressive addition lenses; R, right; s, second.
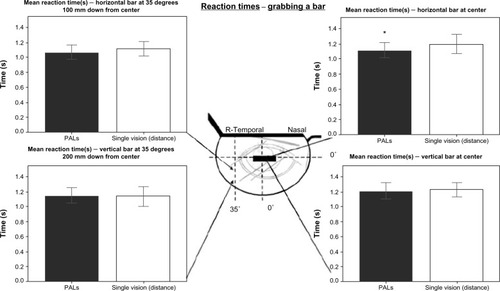
Figure 9 Reaction time measurements for pushing a black line at the various points of fixation while wearing the two glasses.
Abbreviations: PALs, progressive addition lenses; T, temporal; N, nasal.
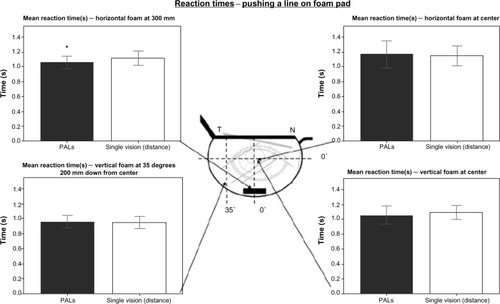
Table 2 Reaction times (seconds) for reaching the targets and the difference in displacement between the two glasses (millimeters) at each position tested
and illustrate accuracy at the specific points that participants localized through the lens. Differences between measurements did not reach statistical significance; however, participants showed a tendency to be less accurate when wearing PALs compared with single vision glasses at the edges of the glasses. At the center of the lens, PALs showed a tendency to be more accurate when the black line was placed vertically; accuracy between the two glasses was similar when the black line was placed horizontally (see and ). The video tape recordings of participants pushing the foam pad with a black line on it endorsed the findings of the switches using the LabChart® and PowerLab® data acquisition systems.
Figure 10 The pie graphs represent accuracy of the participant when pushing the black line on a foam pad at the various points of fixation.
Abbreviations: PALs, progressive addition lenses; T, temporal; N, nasal.
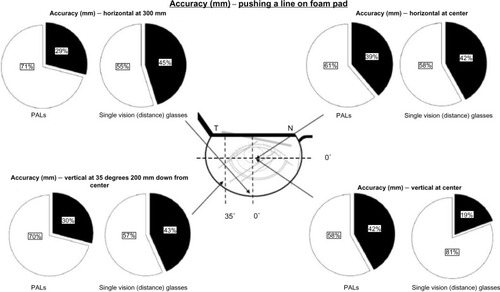
Table 3 Accuracy measurements in binomial distribution for each of the positions tested
Discussion
It has been shown that elderly people who can grasp a support stick at a distance further away from them have a lower incidence of falls.Citation18 The ability to reach out and grab a support with accuracy and without hesitation is important in a fall. To our knowledge this is the first study to look at the prismatic displacement effect on reaction time and accuracy when an elderly person extends their arm to touch a target. In our study, participants were faster at grasping a bar and pushing a black line placed in the central visual axis when wearing PALs compared with single vision glasses. This primary finding is consistent with the study by Lord et al on falls among long-term multifocal wearers.Citation4 One of the secondary measures of Lord et al’s trial was reaction time with a light as a stimulus and participants wearing their preferred eyewear. The study showed that participants who wore multifocal glasses had a tendency to react faster compared with non-multifocal glasses wearers; mean (SD) time to react was 276 (57) and 288 (58) ms, respectively.
Results from our study showed that reaction time tested in the majority of areas of fixation and all of the accuracy measurements were non-significant between the two types of glasses, which is consistent with the VISIBLE trial. The VISIBLE trial suggests that swapping multifocal glasses with single vision distance glasses had no overall effect on fall- prevention (incidence rate ratio [IRR] 0.92 [95% CI 0.73–1.16]).Citation8 Additionally, preplanned subgroup analysis showed that by replacing multifocal with single vision glasses there was a significant increase in falls in older frail people compared with controls who continued wearing their multifocal glasses, especially in an outdoor (unfamiliar) environment (IRR 1.56; 95% CI 1.11–2.19).Citation8 However, the VISIBLE trial did illustrate through the same subgroup analysis that active older people benefit from replacing their multifocal glasses with single vision glasses (IRR 0.60; 0.42–0.87), specifically when in an outdoor environment (IRR 0.61; 95% CI 0.42–0.87).Citation8
Anecdotal evidence suggests that when first prescribed multifocal glasses, the person experiences a significant undulating effect, which decreases with time. The sensation of inappropriate motion (oscillopsia) seems to be most present around the initial time of adaptation.Citation19
Furthermore, it has been shown that people can adjust to glasses that invert the image seen; once the glasses are removed, they simply adjust back within 30 minutes.Citation20 It is suggested that this is due to the brain accommodating the change, through recalibration of the proprioception receptors in the upper and lower limbs and extra retinal eye movements (egocentric and oculocentric visual directions), rather than a correction of the vision. With that in mind, the participants in this trial may have adapted to their PALs, having worn them for a mean of 228 days (SD 146 days), and were thus able to react more quickly than with a new pair of single vision glasses. In changing glasses and thus reversing the prismatic effect, the participant is required to readjust to the prismatic change. However, this effect was not specifically tested in our study and it is not unreasonable to postulate that the effect of replacing PALs with single vision glasses may work in reverse, but this would need further study.
The findings from the study by Cumming et al suggest caution should be taken with a sudden change in older people’s vision.Citation21 In this study the intervention was aimed at improving vision (eg, arranging for new eyeglasses) and this increased rather than decreased the number of falls by participants over a 12 month period. The majority of the intervention participants that required visual improvement acquired a new pair of glasses (92 of 146, 63%). Furthermore, most participants in the intervention arm had their glasses changed ≥13 months before the trial started (209 of 309, 68%); perhaps a more gradual process of updating is required to allow for adjustment to the change in vision. The increase in fall rate seen in the intervention arm was most prominent within the first 3 months of updating their glasses. However, the length of time needed to adapt to multifocal glasses has not been defined.
When an older person walks into an unfamiliar environment, he or she unconsciously remembers the potential support objects in space in that room, spatial memory known as stored central visual spatial information;Citation22 it is possible that this information is stored incorrectly when replacing glasses with different prismatic displacements. Therefore, when a trip, slip, or loss of balance does occur and the older person needs to rely on that stored information, they may miss the support object. According to our study, this would be true only for the vertical displacement in the center and the horizontal bar placed at this position for reaction time.
Our results found a difference in reaction time when the black line was placed at a position of 300 mm down from center, but this cannot be explained by the prismatic displacement effect as there was no statistically significant vertical displacement between the two glasses at this point (P=0.258). Alternatively the result at this position could be explained by the reading portion of PALs because the black line was placed 666 mm away from the participants. This is the optimal focus – that is, around 600 mm – for the reading power of multifocal glasses.Citation4 The mean focal distance of participants’ PAL reading portion in this study was 395 mm (range, 500–333 mm). Therefore, the reading portion brought the line closer to the participant and the resolution may be clearer, enabling the participant to push the line more quickly.
There are alternative explanations for why multifocal glasses have an effect on falls in the elderly population. Timmis et al’s work suggests that participants wearing single vision glasses had more control when stepping down from a block height when compared with individuals who were well adapted to multifocal lenses.Citation9 The study compared kinematic mechanics in 20 older people and found that those participants wearing single vision glasses had reduced vertical center of mass velocity, increased single-limb support time, and reduced peak ankle and knee angular velocities. This suggested that landing occurred in a more controlled manner when wearing single vision glasses. Another study by Elliott et al involved ten elderly participants and their stepping kinematics onto a raised surface when wearing a positive or negative blurring.Citation23 The study found that stepping movements were refected by the magnification effect of the lens on the position and size of the step. The step looked closer with a positive lens, which influenced the participant’s trailing foot to be placed further away and increased their leading vertical toe clearance. With a negative lens the reverse was true. They recommend that partial changes in correction should be prescribed and that updating glasses should therefore occur more frequently.
Replacing multifocal glasses with single vision glasses could be harmful for other reasons. In the VISIBLE trial, secondary measures were recorded of non-fall-related injuries such as lacerations, lifting or twisting injuries, burns or scalds, eye injuries, collisions, and pedestrian injuries.Citation8 They found that 26% of participants replacing multifocal glasses with single vision glasses had a non-fall related injury, compared with 17% of the control group (P=0.01). This effect could be due to the convenience of multifocal glasses when carrying out everyday tasks such as cooking, driving, shopping, or similar activities.
It is acknowledged that this study had limitations. The study population were healthy, active participants, which may not enable generalizability to the older population at greatest risk of a fall. The technique used to map the prismatic displacement was limited to the mask used to map the section of the lens. There was a balance between mapping the largest prismatic displacement at the edge of the glasses, while testing had to occur within the spectacle frame. The general trend was for the prismatic displacement to increase the further out from the center of the lens tested. Therefore, if the targets used to test accuracy and reaction time were placed in a more peripheral position, they could have potentially shown a larger effect compared with the areas of fixation that were tested. However, this was not possible due to the frames of the participants’ glasses. Although the frames of the new single vision glasses were matched to the participant’s PALs, there could have been a slight differences in tilt, vertex, adjustment, and size of the new pair of glasses. These differences could account for the small difference seen in reaction time. Another limitation with this study is that a light stimulus was used instead of a trip, slip, or loss of balance. Therefore, there was no heightened awareness through a fight-or-flight response. A one-off trial which involves a perturbation rather than a light stimulus would possibly be a better method to simulate a fall.Citation22,Citation24
Conclusion
Our study expands on the paper by Lord et alCitation4 and examines the influence on response to a loss of balance when replacing multifocal glasses with single vision (distance) glasses. To our knowledge, this is the first study to test prismatic displacement and fall risk in older people. In conclusion, this study suggests that updating glasses should possibly occur more often in the elderly population to avoid abrupt changes in prismatic displacement.
Acknowledgments
We would like to extend our gratitude to all the optometrists from Dunedin. Thanks are also owed to Mike Jowsey, Moaz AlShaikhi, Terry Costard, and Ralph Harvey; the Department of Medicine, Department of Psychology and the School of Physiotherapy at the University of Otago; and ADInstruments Ltd. This work was supported by a grant from the Ophthalmological Society of New Zealand’s Postgraduate Education Trust. The content within this manuscript has not been published or submitted for publication elsewhere.
Disclosure
The authors report no conflicts of interest in this work.
References
- Fact Sheet No 344, Oct 2012 [webpage on the internet]GenevaWorld Health Organization2014 [cited April 28, 2013]. Available from: http://www.who.int/mediacentre/factsheets/fs344/en/Accessed February 11, 2011
- ScuffhamPChaplinSLegoodRIncidence and costs of unintentional falls in older people in the United KingdomJ Epidemiol Community Health200357974074412933783
- KronfeldPCAlbertDMO’ConnellMOphthalmology in the United States at the time of the revolutionSurv Ophthalmol19772214856333650
- LordSDayhewJHowlandAMultifocal glasses impair edge contrast sensitivity and depth perception and increase the risk of falls in older peopleJ Am Geriatr Soc200250111760176612410892
- HaranMJLordSRCameronIDPreventing falls in older multifocal glasses wearers by providing single-lens distance glasses: the protocol for the VISIBLE randomised controlled trialBMC Geriatr200991019321012
- JalieMProgressive lenses Part 1: how progressive power is obtainedContinuing Education and Training200523140
- Characteristics of a prism Optical Formulas Tutorial [webpage on the internet]Allen Park, MINational Federation of Opticianry Schools1998 [cited April 28, 2013]. Available from: http://www.nfos.org/degree/opt11/module_12b.htmlAccessed September 12, 2011
- HaranMJCameronIDIversRQEffect on falls of providing single lens distance vision glasses to multifocal glasses wearers: VISIBLE randomised controlled trialBMJ2010340c226520501583
- TimmisMAJohnsonLElliottDBBuckleyJGUse of single-vision distance spectacles improves landing control during step descent in well-adapted multifocal lens-wearersInvest Ophthalmol Vis Sci20105183903390820207976
- JohnsonLElliottDBBuckleyJGEffects of gaze strategy on standing postural stability in older multifocal wearersClin Exp Optom2009921192618637106
- CampbellAJSandersonGRobertsonCPoor vision and fallsBMJ201034013131314
- New Zealand Ministry of TransportLand Transport (Driver Licensing) Rule 1999. NZ road safety committeeWellingtonMinistry of Transport1999 Available from: http://nzta.thomsonreuters.co.nz/REG-NZL-PUB-Y.1999-100.pdfAccessed June 9, 2011
- CockrellJRFolsteinMFMini Mental State ExaminationAbou-SalehMTKatonaCLEKumarAPrinciples and Practice of Geriatric Psychiatry2nd edHoboken, NJJohn Wiley and Sons2002140141
- ADinstruments [homepage on the Internet]CanberraADinstruments2014 Available from: http://www.adinstruments.comAccessed June 22, 2011
- Rossiter-FornoffJEWolfSLWolfsonLIBuchnerDMA cross-sectional validation study of the FICSIT common data base static balance measures. Frailty and Injuries: Cooperative Studies of Intervention TechniquesJ Gerontol A Biol Sci Med Sci1995506M291M2977583799
- YardleyLBeyerNHauerKKempenGPiot-ZieglerCToddCDevelopment and initial validation of the Falls Efficacy Scale-International (FES-I)Age Ageing200534661461916267188
- ClarkMSBondMJThe Adelaide Activities Profile: a measure of the life-style activities of elderly peopleAging (Milano)1995741741848541368
- ButlerAALordSRFitzpatrickRCReach distance but not judgment error is associated with falls in older peopleJ Gerontol A Biol Sci Med Sci201166889690321593015
- DemerJLPorterFIGoldbergJJenkinsHASchmidtKAdaptation to telescopic spectacles: vestibulo-ocular reflex plasticityInvest Ophthalmol Vis Sci19893011591702912909
- TuanKMJonesRAdaptation to the prismatic effects of refractive lensesVision Res19973713185118579274770
- CummingRGIversRClemsonLImproving vision to prevent falls in frail older people: a randomized trialJ Am Geriatr Soc200755217518117302652
- KingECLeeTAMckaySMDoes the eyes lead the hand principle apply to reach-to-grasp movements evoked by unexpected balance perturbations?Hum Mov Sci201130236838321035219
- ElliottDBChapmanGJAdaptive gait changes due to spectable magnification and dioptric blur in older peopleInvest Ophthalmol Vis Sci201051271872219797224
- AllumJHTangKSCarpenterMGOude NijhuisLBBloemBRReview of first trial responses in balance control: influence of vestibular loss and Parkinson’s diseaseHum Mov Sci201130227929521435732
