Abstract
Cataract is a significant cause of visual disability in the pediatric population worldwide and can significantly impact the neurobiological development of a child. Early diagnosis and prompt surgical intervention is critical to prevent irreversible amblyopia. Thorough ocular evaluation, including the onset, duration, and morphology of a cataract, is essential to determine the timing for surgical intervention. Detailed assessment of the general health of the child, preferably in conjunction with a pediatrician, is helpful to rule out any associated systemic condition. Although pediatric cataracts have a diverse etiology, with the majority being idiopathic, genetic counseling and molecular testing should be undertaken with the help of a genetic counselor and/or geneticist in cases of hereditary cataracts. Advancement in surgical techniques and methods of optical rehabilitation has substantially improved the functional and anatomic outcomes of pediatric cataract surgeries in recent years. However, the phenomenon of refractive growth and the process of emmetropization have continued to puzzle pediatric ophthalmologists and highlight the need for future prospective studies. Posterior capsule opacification and secondary glaucoma are still the major postoperative complications necessitating long-term surveillance in children undergoing cataract surgery early in life. Successful management of pediatric cataracts depends on individualized care and experienced teamwork. We reviewed the etiology, preoperative evaluation including biometry, choice of intraocular lens, surgical techniques, and recent developments in the field of childhood cataract.
Introduction
Pediatric cataract is one of the major causes of preventable childhood blindness, affecting approximately 200,000 children worldwide, with an estimated prevalence ranging from three to six per 10,000 live births.Citation1–Citation3 Pediatric cataracts may be congenital if present within the first year of life, developmental if present after infancy, or traumatic. Early diagnosis and treatment are of crucial importance to prevent the development of irreversible stimulus-deprivation amblyopia. The management of pediatric cataract should be customized depending upon the age of onset, laterality, morphology of the cataract, and other associated ocular and systemic comorbidities.
Recent advances in surgical techniques, intraocular lens (IOL) composition and designs, increased understanding about the neurobiology of visual development, and early postoperative use of contact lenses for optical rehabilitation have contributed to improved outcomes after pediatric cataract surgery. Furthermore, early diagnosis can be achieved by genetic counseling and testing in cases of hereditary cataracts.Citation4
However, certain issues specific to pediatric eyes, such as increased postoperative inflammation, axial growth after cataract extraction, implant-power calculation, secondary glaucoma, posterior-capsule opacification (PCO), and amblyopia management, are still major obstacles to achieving good visual outcomes in childhood cataract surgery.Citation5–Citation9
Examination of the child
The evaluation of a child with a cataract begins with a detailed history including family history; a prenatal history including maternal drug use and febrile illnesses with rash; and birth history, especially birth weight, since low birth weight may be associated with idiopathic bilateral congenital cataracts.Citation10 A developmental history should be carefully assessed, and if required, review should be sought to exclude metabolic or systemic related etiologies. A history of the onset of the lenticular opacities, laterality, and progression is also important. Unilateral cataracts are usually isolated, but they are most commonly found to be associated with persistent fetal vasculature (PFV);Citation11 also, other ocular abnormalities, such as lenticonus/lentiglobus may be associated.
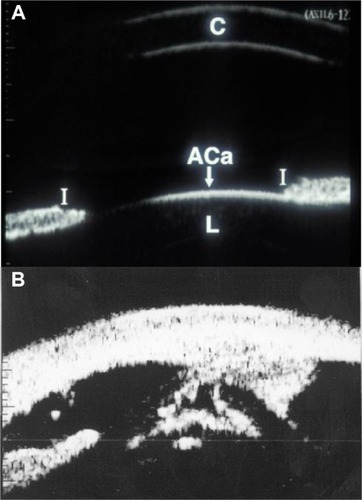
A detailed ocular examination is carried out either in the office or in the operating room. This should include slit-lamp biomicroscopy to assess the size, location, density of lenticular opacity, capsular changes, such as preexistent posterior capsular defects, and other associated anterior-segment developmental anomalies. In addition, measurement of intraocular pressures and corneal diameters are performed. Fundus examination in partial cataracts and ultrasound examination in total cataracts may reveal posterior-segment abnormalities that may affect the visual outcome. Ultrasound biomicroscopy can be informative in children with anterior-segment developmental anomalies and PFV, and also in the assessment of posterior capsular support while considering secondary IOL implantation ().Citation12–Citation14 In children under 12 months of age, it is sometimes possible to examine them after they have been fed milk.
Figure 1 Ultrasound biomicroscopy images.
Abbreviations: C, cornea; I, Iris; ACa, anterior capsule; L, lens.
In preverbal children who are uncooperative for standard visual acuity testing, fixation behavior, fixation preference, and objection to occlusion should be checked. In younger infants with poorly developed fixation, a red reflex test can be performed in a darkened room with a direct ophthalmoscope along with undilated retinoscopy to assess the visual significance of the lens opacity. A central cataract larger than 3 mm in diameter, unilateral cataract associated with strabismus, and bilateral cataract with nystagmus are considered visually significant.Citation15 Asking about the visual interaction of the child at home with the family members, also helps in determining the severity of visual dysfunction.
It is important to check the visual acuity in older cooperative children, if possible with preferential looking cards (Teller acuity card, Keeler, etc), or other vision tests such as “E” charts or Snellen chart appropriate to the age of the child. In cases of lamellar or posterior subcapsular cataracts, the visual acuity in an examination lane with dim light may appear normal or reasonable, but glare testing where visual acuity drops by two or more lines, will reveal potential difficulty in daylight. The glare test is performed by shining a bright light to the side of each eye as the child attempts to read the vision chart.
Visual evoked potential
For preverbal, less cooperative, or developmentally delayed children, pattern visual evoked potential (VEP) can be used to assess the effect of the opacity on the visual pathway, thereby indirectly reflecting visual significance of the opacity.Citation16–Citation18 Flash VEPs may be useful in complete cataracts to establish the gross integrity of the visual pathways.Citation19
Family-album tomography scan
The parents can be asked to bring the family photograph album if they are unsure about the onset of cataract. Especially when an older child presents with unilateral cataract, inspection of the red reflex in old photographs may give a clue as to whether the cataract was present during the critical period of visual development, or not.Citation19
Examine the family members
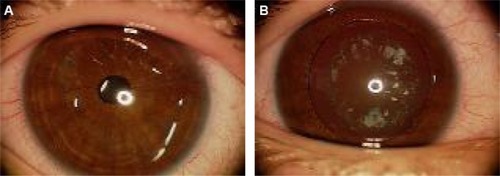
A dilated slit-lamp examination of the parents and any sibling should be performed, which may reveal previously undiagnosed lenticular changes indicative of an inherited cause for the child’s cataract (). Female carriers of X-linked conditions associated with males presenting with congenital cataracts may show lenticular changes. Some important examples are punctate lens opacities in a mother of a male child with Lowe syndrome, and Y-sutural opacities in a mother of a male child with Nance–Horan syndrome.Citation16,Citation20,Citation21
Morphology of pediatric cataract: specific diagnostic
A detailed description of the morphology of a pediatric cataract may not only help in the diagnosis of a specific condition but also in planning the management with regard to surgical as well as nonsurgical treatment. Morphologically, pediatric cataracts can be broadly classified into the cataracts involving the entire lens, central cataracts, anterior cataracts, posterior cataracts, punctate lens opacities, coralline cataracts, sutural cataracts, wedge-shaped cataract, and cataracts associated with PFV.Citation11 In this review, we want to highlight cataracts with typical morphology specific to certain systemic conditions or syndromes that may be helpful to diagnosis.
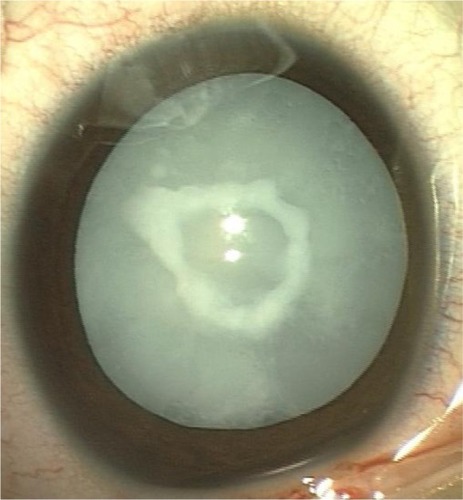
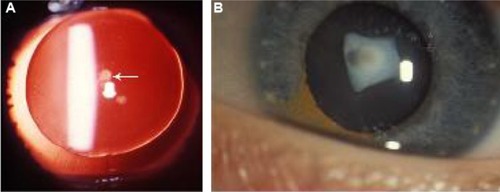
Total cataracts can be sporadic or hereditary in nature (); they can also be seen in Down’s syndrome and congenital rubella syndrome.Citation11 Early surgical intervention is mandatory to prevent the development of amblyopia.
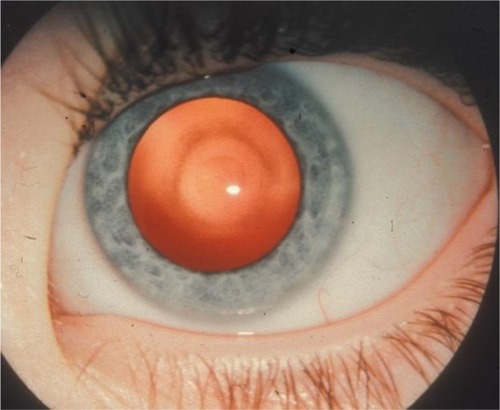
Anterior polar cataracts are not pathognomonic of any particular condition, but are commonly seen in patients with aniridiaCitation9 (). They can appear as dot-like, plaque-like, or in the form of a pyramid. Pyramidal cataracts are the severe form of anterior capsulolenticular opacities in the form of a pyramid protruding into the anterior chamber, and have also been described in children with retinoblastoma and Ehlers–Danlos syndrome ().Citation22,Citation23
Figure 4 Anterior polar cataract.
Anterior subcapsular cataracts are associated with uveitis, trauma, irradiation, and atopic dermatitis. Anterior lenticonus is a bilateral condition seen in Alport syndrome, and rarely in Waardenburg syndrome.Citation24,Citation25
Oil-droplet cataracts are the nuclear opacities typically seen in infants with galactosemia (). However, other forms of cataract, such as posterior subcapsular or small nuclear and cortical opacification, are also described in galactosemia.Citation26 The changes are reversible with early dietary modification.
Sunflower cataract is a type of anterior subcapsular cataract almost only seen in Wilson’s disease, an autosomal-recessive condition with a defect in the metabolism of copper leading to accumulation of copper in the liver and basal ganglia. These lenticular opacities are also reversible with treatment with penicillamine.Citation27
Posterior subcapsular cataract can be drug-induced (steroids most commonly) or a complication of radiation therapy for ocular and periocular tumors.Citation28,Citation29 It has also been reported in systemic conditions, such as Turner’s syndrome, Fabry’s disease, Bardet–Biedl syndrome, and neurofibromatosis type 2.Citation30–Citation34
Membranous cataracts are the disk-like opacities formed after spontaneous resorption of lens material. These are typically seen in Hallermann–Streiff syndrome.Citation35 This condition has also been described in children with congenital rubella syndrome, Lowe syndrome, and PFV.Citation36–Citation38
Wedge-shape cataracts are partial lenticular opacities, typically associated with Stickler syndrome in addition to Conradi–Hünermann syndrome, neurofibromatosis type 2, and Fabry’s disease.Citation11,Citation39
Punctate cortical opacities sparing the nucleus are characteristically seen in carriers of X-linked recessive Lowe syndrome and in children with Down’s syndrome.Citation11,Citation21,Citation40 Radiating spoke-like cortical punctate opacities are also consistent with Fabry’s disease.Citation31
Sutural cataracts are visually insignificant opacities along the Y-sutures of the lens. They are often found as an incidental finding on routine examination. They have been described in female carriers of Nance–Horan syndrome, with affected males presenting with dense visually significant cataracts.Citation20
Investigations
Although 60% of pediatric cataracts are idiopathic,Citation40 based on the antenatal history, family history, and the type of cataract, a baseline laboratory workup may be required in some cases. Extensive laboratory investigations are not usually indicated for unilateral cataracts, as most of them are isolated, nonhereditary, and without any systemic associations.Citation40,Citation41 However, in any child with a positive maternal antenatal history suggestive of infection or the presence of microcephaly, deafness, cardiac abnormalities, and/or developmental delay should be investigated for varicella, herpes simplex, toxoplasmosis, rubella, and syphilis (TORCHS).Citation42–Citation45 Traumatic etiology, particularly of nonaccidental cause, must always be ruled out in any case of unilateral cataract.
Children with bilateral cataracts may be considered in the following way: 1) well infant – rule out galactosemia and TORCHS; 2) well toddler – rule out galactokinase deficiency; 3) jaundiced infant with failure to thrive – rule out galactosemia, urine screening for reducing substances and erythrocyte assays are effective ways to diagnose galactosemia;Citation26,Citation46 4) unwell infant or child, eg, in a child with coexistent congenital glaucoma, hypotonia, and developmental delay, oculocerebrorenal syndrome (Lowe syndrome) should be ruled out by checking the urine for amino acids.Citation21 Specific conditions may need specific testing, eg, serum calcium, phosphorus, and glucose testing should be tailored based on the child’s systemic exam.Citation47,Citation48 All of these investigations are usually best performed in conjunction with general health assessment of the child by a pediatrician.
Genetic evaluation
Evaluation by a geneticist is helpful for determining the inheritance pattern and to identify associated syndromes. Genetically based cataracts account for 8%–29% of all congenital cataracts, with the majority being autosomal-dominant in inheritance.Citation49 Autosomal-recessive and X-linked patterns have also been isolated.Citation50,Citation51 Clinical and genetic heterogeneity is well documented in autosomal-dominant cataracts.Citation52 More than 40 different genes and various loci have been identified with congenital cataracts.Citation53 Mutations in the genes responsible for the maintenance of lens clarity, such as the crystallin and connexin genes, are the most commonly described in the etiology of nonsyndromic inherited cataracts.Citation49,Citation54 Mutations in the genes coding for transcription factors, aquaporin (Maf), beaded filament structural protein, vimentin, and lens intrinsic membrane proteins have also been reported.Citation49,Citation54
Mutations in the α-crystallin gene tend to cause nuclear, lamellar, zonular, and posterior polar cataracts. In addition to primary cataract, mutation in CRYAA has been associated with microcornea. Phenotypic variability is commonly observed with mutations in the β-crystallin genes.Citation55 Mutations in the developmental genes, such as PAX6, FOXE3, PITX3, and MAF have also been implicated with cataract as a part of anterior-segment developmental anomalies.Citation53 Anterior polar cataracts are commonly seen with PAX6 mutations with or without aniridia, whereas PITX3 mutations predominantly cause posterior polar cataracts.Citation56,Citation57
Furthermore, genes responsible for major syndromic cataracts include OCRL (Lowe syndrome),Citation21,Citation58 GALK117q (galactosemia),Citation58 GLA (Fabry’s disease), and NHS (Nance– Horan cataract–dental syndrome).Citation59
Management
Nonsurgical management
Indication for cataract surgery depends upon how much visual function is affected. The mere presence of a lenticular opacity does not indicate surgical removal. Peripheral lens opacities, punctate opacities with intervening clear zones, and opacities less than 3 mm in diameter can be observed closely and successfully managed by treating the associated amblyopia by patching and glasses.Citation60 For example, anterior polar and pyramidal cataracts are not visually significant per se, but can be associated with significant progressive corneal astigmatism, which can lead to decreased visual acuity and amblyopia.Citation61 In addition, in small central opacities, a larger area of clear visual axis can be achieved by pharmacological dilatation.Citation62 In a recent report, Birch et al found that abnormal visual acuity and contrast sensitivity in young children with partial cataracts was associated with poor long-term visual acuity outcomes.Citation63 This suggests that while conservative treatment can be used, it must be done so with caution, and ancillary tests such as glare testing must be utilized to ensure the lens opacity is not visually significant.
Surgical management
A critical period for visual development has been described in the first 6 weeks of life, during which the vision is subcortically mediated and the infant is relatively resistant to amblyopia.Citation64 Extraction of unilateral congenital cataracts by 4–6 weeks and bilateral congenital cataracts within the first 6–8 weeks of life can prevent the development of stimulus-deprivation amblyopia, strabismus, and nystagmus.Citation65,Citation66 Prompt optical rehabilitation and occlusion therapy can result in good visual acuity with fusion and stereopsis.Citation67
A child’s eye is unique
Pediatric eyes are different from adult eyes. They are smaller in size at birth, with changing axial length and corneal curvature over a period of time. The mean axial length of a newborn eye is 16.5 mm. There is rapid growth of eyes in the first 18 months, which increases to 23 mm by 13 years of age.Citation68 Similarly, there is a change in the corneal curvature: from 51.2 D in newborns to 43.5 D in adults.Citation69,Citation70 They have a thin and less rigid sclera, a more elastic capsule, and a risk of severe inflammatory response after surgery. Furthermore, a child has a longer life span after cataract removal, with a potential for irreversible visual loss due to amblyopia. Therefore, presurgical evaluation of a growing child’s eye is a little complex. Moreover, the process of emmetropization is potentially disrupted.
Preoperative evaluation: biometry
Optical correction after pediatric cataract surgery may be achieved by aphakic glasses, contact lenses, or primary IOL implantation. Despite the increasing popularity of primary IOL implantation, particularly in young infants, prediction of eye growth over a period of time and choosing an appropriate IOL power to prevent the unexpected refractive change is still a challenge. In a recent survey, approximately 70% of the American Association of Pediatric Ophthalmology and Strabismus members worldwide preferred to implant an IOL in children.Citation70,Citation71 Because of the myopic shift over a period of time, it is essential to predict eye growth and have an accurate biometry in order to choose the appropriate IOL power suited for each child at the time of surgery and well into the future. Accurate measurements of axial length and keratometry in the office setting may be difficult because of poor patient cooperation and poor fixation, and most of the time biometry has to be performed under sedation or general anesthesia in the operating room. Immersion biometry has been shown to be more predictable than the contact method for IOL-power calculation children.Citation72
IOL power
While the general consensus among pediatric cataract surgeons worldwide is partial undercorrection at the time of surgery to balance the postoperative myopic shift, some studies have reported a reduction in axial elongation, and some have reported an increase in axial elongation in young children.Citation73–Citation75 Axial elongation has been reported to be more after unilateral cataract extraction in the operated eye than bilateral cataract surgery.Citation5 Recent work has documented axial growths in children operated on at 10 years of age, and advised a refractive target of residual mild hyperopia at the time of surgery in older children.Citation76 Considering these issues, the choice of IOL power should be individualized based on the child’s need and refractive status of the other eye in unilateral cases.
An accurate IOL-calculation formula is required for proper selection of IOL power. SRK II, Holladay 1, Holladay 2, Hoffer Q, SRK/T, and Pediatric IOL Calculator (a computer program) have been used to calculate the desired IOL power in children, with variable results.Citation6,Citation7,Citation77 Various factors, including inaccuracies of axial length measurements in the supine position, biometry technique, keratometry values, phenomenon of pseudoaccommodation, variability in IOL position due to capsule fibrosis, and increased corneoscleral elasticity in children, have been suggested to contribute to prediction errors.Citation77–Citation81 Additionally, in children younger than 2 years, smaller axial lengths, shallower anterior chambers, and changes in corneal curvature and corneal thickness may lead to higher prediction errors.Citation7,Citation82 In the Infant Aphakia Treatment Study (IATS), less than half of the children were within 1.00 D of target refraction, with the greatest prediction errors in eyes with axial lengths of 18 mm or less.Citation83 The recent report of IATS recommended Holladay 1 and SRK/T formulae for infant eyes.Citation84 However, at 5 years, they found refractive errors ranging from +5.00 to −19.00 D, and the authors believe that the inability to predict axial elongation in infantile eyes was the primary reason for such a wide range of refractive errors.Citation75,Citation85
Absolute prediction errors are common even after secondary IOL implantation, and are reported to range from 0.9±0.9 D to 2.15±1.68 D.Citation86–Citation89 Refraction-based formulae by Hug, Khan and Algeed for estimation of secondary posterior-chamber IOL power provide comparable results to those obtained by standard biometry-based formulas, and can be useful in difficult situations when standard biometry cannot be performed or when it is not available in the operating room.Citation86 It is important to note that the Hoffer Q equation relies on an anterior-chamber depth (ACD) value and not on the A-constant. The ACD value is the predicted postoperative ACD. The value given by pharmaceutical companies for each IOL is that for adults. It is larger than that expected for children and especially infants. To use a more accurate ACD value, the author measures the ACD of both eyes and then predicts the ACD, using this value for the Hoffer Q. As a rule of thumb, 1 mm is added to the preoperative ACD, but this may be modified in unilateral cases, depending on what the ACD is of the unaffected eye. The author uses an empiric rule whereby children under the age of 3 months are left +8.00 D, 3 months to 1 year +6.00 D, 1–2 years +4.00 D, 2–3 years +3.00 D, 3–5 years +2.00 D, 5–7 years +1.00 D, and 7 years and after +0.5 D until the age of 11 years. These numbers may be modified in unilateral cases, depending upon the refraction of the other eye, so as to cause minimal anisometropia 2 years after surgery.
Type of IOL
In recent years, acrylic IOLs have gained popularity over polymethyl methacrylate (PMMA) IOLs, which had remained the IOL of choice for many years.Citation71,Citation90,Citation91 In children, AcrySof IOLs are considered better than PMMA IOLs in terms of greater biocompatibility and smaller incision size with use of foldable design, with late onset and lower rate of PCO formation. Hydrophobic acrylic IOLs are used by 93% of pediatric cataract surgeons. The one-piece lenses (SA or SN series) for in-the-bag fixation and three-piece lenses (MA series) for sulcus fixation are preferred.Citation71 In children with uveitic cataracts, decreased postoperative inflammation has been reported with the use of heparin-surface-coated PMMA IOLs.Citation92 Silicone IOLs are used less frequently, because of an increased rate of capsule contraction.Citation93
In special situations, such as in children with dislocated lenses either due to trauma or systemic conditions, such as Marfan’s syndrome (), transscleral sutured monofocal or multifocal IOLs may be considered for visual rehabilitation. However, limited studies in children have been reported, with a 12%–24% rate of spontaneous dislocation of IOL from suture breakage over a follow-up period of 10 years. This is concerning in the pediatric population because of their longevity.Citation94–Citation96 Secondly, transscleral sutured IOL is considered a blind procedure with low accuracy of placement of haptics in the sulcus.Citation97
Alternatively, iris-fixated IOLs, such as iris-sutured IOLs and iris-claw IOLs, have been reported with short-term success with complications, including retinal detachment after dislocation, hyphema, synechiae, ectopic pupil, fibrinous uveitis, and vitreous strands in the wound.Citation98,Citation99 Few studies exist that report the use of angle-supported anterior-chamber IOLs in older children.Citation100,Citation101 A modified capsular tension ring with posterior-chamber IOL implantation is another option in children with partial loss of zonular support.Citation102 The indications for multifocal IOLs in children are debatable. Simultaneous distance and near vision without the aid of glasses or contact lenses can be achieved with the use of multifocal IOLs. This is especially important in children, as they lose accommodation once the cataract is removed. Refractive shift during eye growth as well as amblyopia due to loss of contrast sensitivity associated with multifocal IOLs are the main concerns of most pediatric cataract surgeons.Citation71 Although limited studies in children have shown improved stereopsis and spectacle independence with the use of multifocal IOLs, studies with long-term follow-up are warranted.Citation103–Citation105
Surgical technique
Wound
Cataract surgery in children is challenging, because of increased scleral elasticity, thicker corneas, increased risk of trauma from eye rubbing, less compliance with activity restriction, and most importantly the effect of postoperative astigmatism on amblyopia. While scleral tunnel incision was preferred by most pediatric cataract surgeons because it was thought to induce less postoperative astigmatism, recent studies have shown clinically insignificant difference between the two types of incisions, with spontaneous regression of astigmatism over a period of time.Citation106 Superior incisions are commonly performed compared to the temporal approach, probably in view of less risk of injury and postoperative endophthalmitis. As the flattening of the cornea occurs along the incisional meridian, there is a tendency toward with-the-rule astigmatism with the temporal approach in young children.Citation107 The temporal approach is desirable in deep-seated eyes and in children with previous or planned filtration surgery superiorly. However, there is no study comparing the astigmatic outcome after pediatric cataract surgery with the superior and temporal approaches. Lensectomy through pars plana approach can also be done if IOL insertion is not intended immediately.
To prevent wound leakage due to the reasons mentioned, suturing of all the wounds, including paracentesis with either a 10-0 or 9-0 Vicryl or nylon suture, is recommended. Absorbable sutures are preferred, in order to avoid a second visit to the clinic or operating room for suture removal. Research has shown that the use of 10-0 Vicryl caused astigmatism, but that this astigmatism dissipated after 6 weeks.Citation108
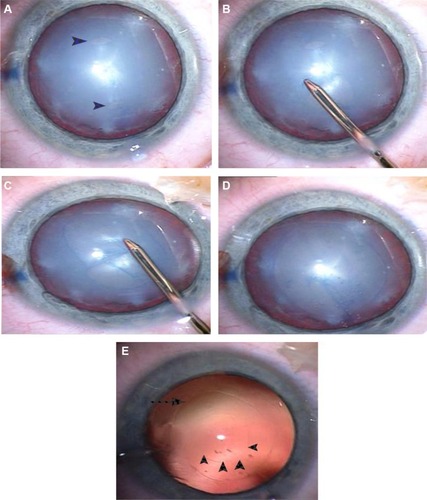
Capsulotomy
Continuous, smooth, and well-centered anterior capsulotomy is a prerequisite for safe lens implantation. Currently used techniques for pediatric anterior capsulotomies include vitrectorhexis, manual continuous curvilinear capsulorhexis (CCC), can-opener, and radio-frequency diathermy.Citation109–Citation112 Other devices, such as the plasma blade, diacapsutom, and pulsed-electron avalanche knife, have been suggested to minimize zonular tension and prevent peripheral CCC extension, but have not become popular.Citation113 Elasticity and thickness of the anterior capsule in young children makes manual CCC the most difficult technique, with a steep learning curve. It can be performed either with a cystotome or forceps. Manual CCC has been shown to produce the most extensible capsulotomy and the smoothest edge with scanning electron microscopy evaluation in a porcine model.Citation114 Although manual CCC has been the gold standard, some surgeons prefer to use the vitrector for very young patients and manual CCC for older children.Citation109 The problem with the vitrectorhexis technique is that it is not robust compared to manual CCC. Traditional manual CCC has a very steep learning curve in children. The two-incision push–pull technique developed by Nischal has been shown to produce consistent-size capsulorhexis openings with minimal risk of extension or tears ().Citation115,Citation116 Recently, Dick and Schultz described promising results with femtosecond laser-assisted anterior and posterior capsulotomies in four children.Citation117 Titiyal et al advocate postage-stamp multiple anterior capsulorhexisotomies to prevent anterior-capsule phimosis.Citation118 For proper centration of the IOL, the anterior capsulotomy should be smaller than the IOL optic. An ideal capsulotomy for an IOL with optic diameter 5.5–6 mm should be 4–5 mm. Smaller capsulotomies may result in severe capsular phimosis, as 15% shrinkage of the capsular bag diameter occurs over 6 months.Citation119
Figure 7 The technique of two-incision push–pull anterior capsulorhexis.
Techniques for cataract extraction
Surgical techniques for pediatric cataract are constantly evolving to minimize the complication rate. Soft consistency of pediatric cataracts makes phacoemulsification unnecessary.Citation120 Lens removal can be conducted through an anterior approach by manual irrigation and aspiration or through the pars plana using a vitrector. In rare cases with membranous cataracts or retrolenticular membranes in PFV, intraocular scissors are required.Citation120 An anterior-chamber maintainer used for continuous irrigation prevents the collapse of the anterior chamber during withdrawal of the instruments during the surgery.Citation121 It also aids in pupillary dilatation with the use of 1:1,000 epinephrine added to the balanced salt solution.Citation122 The use of heparin in the balanced salt solution and intracameral recombinant tissue-plasminogen activator has been shown to reduce the fibrinous reaction and pigment deposits on the IOL.Citation123,Citation124 However, the beneficial effect of heparin on early postoperative inflammation has been questioned in a recent randomized controlled trial.Citation125 Recently, the use of a transconjunctival 25-gauge vitrectomy system has been gaining popularity for lens removal in pediatric patients.Citation126
Posterior-capsule management
Maintenance of a clear visual axis is critical for a good postoperative visual outcome after pediatric cataract extraction. If the posterior capsule is left intact, 100% of eyes less than 4 years of age develop significant PCO.Citation127,Citation130 The anterior vitreous face acts a scaffold for the proliferation of lens epithelial cells (LECs); therefore, it is essential to combine primary posterior capsulotomy (PPC) with anterior vitrectomy in infants and young children.Citation128,Citation129 It can also be considered in older children who are poor candidates for possible neodymium-doped yttrium aluminum garnet (Nd:YAG) laser capsulotomy. PPC can be performed either through a limbal or pars plana approach. The opening for PPC should be smaller than the anterior capsulotomy. Staining of the posterior capsules with trypan blue 0.1% may facilitate the procedure of PPC.Citation130 PPC using the two-incision push–pull technique has been shown to give consistent results without vitreous loss during the procedure.Citation115,Citation116 Praveen et al reported triamcinolone-assisted vitrectomy for visualization of the anterior vitreous during pediatric cataract surgery.Citation131
Optic capture of the IOL was considered another surgical technique that would obviate the need for anterior vitrectomy and prevent the development of PCO.Citation132 However, Vasavada et al believed that anterior vitrectomy was necessary with optic capture even in older children.Citation133 Furthermore, it is a difficult technique to perform with single-piece IOLs without haptic angulation. Posterior vertical capsulectomy with optic entrapment by Grieshaber et al showed promising results in 68 children aged 2 months to 8 years, with clear visual axes for 5–12 years postoperatively. Although this procedure is technically challenging, anterior vitrectomy is seldom required.Citation134
Postoperatively, subconjunctival or intracameral steroids are recommended to suppress inflammation in the immediate postoperative period.Citation135,Citation136 Intracameral recombinant tissue-plasminogen activator has also been shown to reduce the fibrinous reaction and pigment deposits on the IOL after pediatric cataract surgery, though there is a risk of hyphema.Citation124 Decrease in the rates of postoperative endophthalmitis in adults has been reported with the intracameral use of antibiotics. However, there is no study showing its effectiveness in the pediatric population.
Complications
Postoperative increased inflammatory response in children can lead to fibrinous reactions, pigment deposits on the IOL, decentration of the IOL, and posterior synechiae. Toxic anterior-segment syndrome, which is a well-recognized complication after uneventful adult cataract surgery, has also been reported in children.Citation137 Even capsular blockage syndrome has been reported following pediatric cataract surgery.Citation138 Secondary glaucoma is the most feared complication of pediatric cataract surgery, and is commonly seen in infants. Studies, including a recent report of the IATS, showed that IOL implantation does not seem to protect from the development of secondary glaucoma.Citation85,Citation139 However, in a recent meta-analysis, Mataftsi et al found that glaucoma risk after infantile cataract surgery appears to be associated with surgery within the first month of life and additional intraocular surgical procedures, but not with primary IOL implantation. Therefore, the factors influencing the risk for postoperative glaucoma remain an unresolved issue.Citation8
Measurement of central corneal thickness in aphakic as well as pseudophakic eyes is essential to diagnose true glaucoma.Citation140 Therefore, monitoring for glaucoma is mandatory for any child undergoing cataract surgery early in life. Retinal detachment is a rare late complication of pediatric cataract surgery.Citation141 It is not known whether the pars plana approach is associated with increased risk for retinal detachment.
Visual axis opacification remains the most common complication after pediatric cataract surgery. Although PPC, anterior vitrectomy, use of hydrophobic acrylic IOL, or in-the-bag IOL implantation have been effective in preventing or delaying the occurrence of PCO, it is still a major concern in infantile eyes. Severe capsular phimosis can also occlude the visual axis. Nd:YAG laser capsulotomy or surgical membranectomy can be performed to clear the visual axis. Sealed-capsule irrigation using either distilled water or 5-fluorouracil has been shown to be successful in reducing the incidence of visual axis opacification in adult eyes by killing the LECs.Citation142,Citation143 This device may help pediatric cataract surgeons to overcome the problem of PCO, but the risk of endothelial cell loss cannot be underestimated. The development of the bag-in-the-lens technique by Tassignon et al shows promise, because by using this lens the LECs are trapped between the anterior and posterior capsules, thus reducing dramatically the rate of PCO.Citation144
Vision rehabilitation
The modalities for visual rehabilitation after pediatric cataract extraction include IOL implantation, aphakic glasses, and contact lenses. Aphakic glasses are an efficient method for visual rehabilitation in children up to 4 years of age. Addition of a bifocal segment is needed in children 4 years of age or older. Contact lenses are usually well tolerated, and the power can be changed until the child is ready for IOL implantation with predictable postoperative refraction. Rigid gas-permeable contact lenses are preferred by the majority of clinicians.Citation145 Good visual acuity can be achieved with contact lens fitting within 3 weeks of surgery in unilateral aphakes.Citation146 A recent report of the IATS comparing outcomes of contact lens and IOL correction showed no significant difference in median visual acuity between two groups at 5 years,Citation85 but showed more complications in the IOL group. No matter what rehabilitation method is used, surveillance is needed.
Unlike adults, visual outcome after a successful cataract surgery in children finally depends on the timely management of amblyopia, especially after unilateral cataract extraction. Generally, patching after pediatric cataract surgery is continued until it is believed that the child is no longer at risk of developing amblyopia. However, there is no consensus about the amount and duration of patching therapy necessary to achieve a good visual result. Extensive occlusion therapy during early infancy may disrupt the development of binocularity.Citation147 Compliance with patching has been shown to be associated with good postoperative visual outcomes in unilateral and bilateral cataracts, more so in monocular cataract.Citation148 Therefore, educating the parents about the importance of amblyopia therapy postsurgery is crucial.
Future directions
Despite the better understanding of pathophysiology of visual maturation in children and advancements in surgical technology and instrumentation, childhood cataract remains a challenge to pediatric ophthalmologists.
Prevention of PCO is a major problem faced by the entire pediatric ophthalmology community worldwide. Capsule-irrigating devices customized for pediatric eyes, which will reduce the speed and severity of proliferation of LECs, or future research discovering the drugs antagonizing the effect of factors responsible for PCO are warranted.Citation142,Citation143 Recently, the results in an animal model indicated that there was a beneficial effect on postoperative inflammation with dexamethasone-coated IOLs.Citation149 It is reasonable to assume that IOLs will be designed that can deliver slow-release molecules to reduce inflammation and obviate the need for topical anti-inflammatory treatment.
Post-operative prediction error is another issue, and there is a need to develop an IOL-calculation formula customized for pediatric eyes to minimize it. Furthermore, future studies are needed to look for the factors, other than secondary glaucoma, affecting postoperative axial growth, so that surgeons will have the ability to predict postoperative refraction and implant an accurately powered IOL in pediatric eyes. There may also be a place for modified implantation techniques and modified IOL designs, such as multicomponent adjustable IOLs (Infinite Vision Optics, Strasbourg, France) to combat refractive surprises.Citation150
Appropriate measures, such as immunization programs for rubella and measles and neonatal screening, can reduce the incidence in developing countries. Finally, continued genetic studies that will allow clinicians to better understand the natural history and likely outcome of the cataract are required.
Disclosure
The authors report no conflicts of interest in this work.
References
- FosterAGilbertCRahiJEpidemiology of cataract in childhood: a global perspectiveJ Cataract Refract Surg199723Suppl 16016049278811
- HolmesJMLeskeDABurkeJPHodgeDOBirth prevalence of visually significant infantile cataract in a defined US populationOphthalmic Epidemiol2003102677412660855
- StayteMReevesBWorthamCOcular and vision defects in preschool childrenBr J Ophthalmol19937742282328494859
- LeeKAParkMHKimYJChunSHIsolated congenital hereditary cataract in a dizygotic twin: prenatal ultrasonographic diagnosisTwin Res Hum Genet201316599499723931615
- VasavadaARRajSMNihalaniBRate of axial growth after congenital cataract surgeryAm J Ophthalmol2004138691592415629281
- JasmanAAShaharuddinBNoorRAIsmailSGhaniZAEmbongZPrediction error and accuracy of intraocular lens power calculation in pediatric patient comparing SRK II and Pediatric IOL CalculatorBMC Ophthalmol2010102020738840
- KekunnayaRGuptaASachdevaVRaoHLVaddavalliPKOm PrakashVAccuracy of intraocular lens power calculation formulae in children less than two yearsAm J Ophthalmol201215411319.e222336039
- MataftsiAHaidichABKokkaliSPostoperative glaucoma following infantile cataract surgery: an individual patient data meta-analysisJAMA Ophthalmol201413291059106724921712
- LimZRubabSChanYHLevinAVManagement and outcomes of cataract in children: the Toronto experienceJ AAPOS20126324925422681941
- HaargaardBWohlfahrtJRosenbergTFledeliusHCMelbyeMRisk factors for idiopathic congenital/infantile cataractInvest Ophthalmol Vis Sci20054693067307316123403
- AmayaLTaylorDRussell-EggittINischalKKLengyelDThe morphology and natural history of childhood cataractsSurv Ophthalmol200348212514412686301
- El ShakankiriNMBayoumiNHAbdallahAHEl SahnMMRole of ultrasound and biomicroscopy in evaluation of anterior segment anatomy in congenital and developmental cataract casesJ Cataract Refract Surg200935111893190519878821
- De SilvaDJNischalKKPackardRBPreoperative assessment of secondary intraocular lens implantation for aphakia: a comparison of 2 techniquesJ Cataract Refract Surg20053171351135616105606
- MackeenLDNischalKKLamWCLevinAVHigh-frequency ultrasonography findings in persistent hyperplastic primary vitreousJ AAPOS20004421722410951297
- ZetterströmCLundvallAKugelbergMCataracts in childrenJ Cataract Refract Surg200531482484015899463
- McCullochDLSkarfBPattern reversal visual evoked potentials following early treatment of unilateral, congenital cataractArch Ophthalmol199411245105188155050
- LloydICGoss-SampsonMJeffreyBGKrissARussell-EggittITaylorDNeonatal cataract: aetiology, pathogenesis and managementEye (Lond)19926Pt 21841961624043
- NucciPPattern reversal visual evoked potentials following early treatment of unilateral, congenital cataractArch Ophthalmol199511344044067710383
- TaylorDWrightKWAmayaLShould we aggressively treat unilateral congenital cataracts?Br J Ophthalmol20018591120112611520768
- DingXPatelMHerzlichAASievingPCChanCCOphthalmic pathology of Nance-Horan syndrome: case report and review of the literatureOphthalmic Genet200930312713519941417
- LavinCWMcKeownCAThe oculocerebrorenal syndrome of LoweInt Ophthalmol Clin19933321791918325732
- KostickAMRomanchuckKGBeebeDCAnterior pyramidal cataracts in Ehlers-Danlos syndromeCan J Ophthalmol19963131331368743223
- BrownGCShieldsJAOglesbyRBAnterior polar cataracts associated with bilateral retinoblastomaAm J Ophthalmol1979873276434085
- LiuZSunCBYaoKAnterior internal lenticonus accompanied by congenital nuclear cataractChin Med J (Engl)2011124234119412022340358
- StevensPRAnterior lenticonus and the Waardenburg syndromeBr J Ophthalmol19705496216235458254
- BeigiBO’KeefeMBowellRNaughtenEBadawiNLaniganBOphthalmic findings in classical galactosaemia – prospective studyBr J Ophthalmol19937731621648457508
- RamJGuptaAKayser-Fleischer ring and sunflower cataract in Wilson diseaseJAMA Ophthalmol2014132787324809467
- SuhSYKimJHKimSJYuYSSystemic steroid-induced cataracts in children: long-term changes in morphology and visual acuityJ AAPOS201317437137323911128
- HoehnMEIrshadFKerrNCWilsonMWOutcomes after cataract extraction in young children with radiation-induced cataracts and retinoblastomaJ AAPOS201014323223420399694
- EshagianJRaffertyNSGoossensWHuman cataracta complicata. Clinicopathologic correlationOphthalmology19818821551637231901
- SodiAIoannidisASMehtaADaveyCBeckMPitzSOcular manifestations of Fabry’s disease: data from the Fabry Outcome SurveyBr J Ophthalmol200791221021416973664
- SchachatAPMaumeneeIHBardet-Biedl syndrome and related disordersArch Ophthalmol198210022852887065946
- McLaughlinMEPepinSMMaccollinMChoopongPLessellSOcular pathologic findings of neurofibromatosis type 2Arch Ophthalmol2007125338939417353411
- EshagianJHuman posterior subcapsular cataractsTrans Ophthalmol Soc U K1982102Pt 33643686964282
- FallsHFSchullWJHallermann-Streiff syndrome, a dyscephaly with congenital cataracts and hypotrichosisArch Ophthalmol196063340942013821451
- BogerWP3rdPetersenRARobbRMSpontaneous absorption of the lens in the congenital rubella syndromeArch Ophthalmol19819934334347213159
- WegenerJKSogaardHPersistent hyperplastic primary vitreous with resorption of the lensActa Ophthalmol (Copenh)19684621711755755674
- TripathiRCCibisGWTripathiBJPathogenesis of cataracts in patients with Lowe’s syndromeOphthalmology1986938104610513763153
- SeeryCMPruettRCLiberfarbRMCohenBZDistinctive cataract in the Stickler syndromeAm J Ophthalmol199011021431482378378
- LimZRubabSChanYHLevinAVPediatric cataract: the Toronto experience – etiologyAm J Ophthalmol2010149688789220430363
- HaargaardBWohlfahrtJFledeliusHCRosenbergTMelbyeMA nationwide Danish study of 1027 cases of congenital/infantile cataracts: etiological and clinical classificationsOphthalmology2004111122292229815582089
- RaghuHSubhanSJoseRJGangopadhyayNBhendeJSharmaSHerpes simplex virus-1-associated congenital cataractAm J Ophthalmol2004138231331415289153
- LardennoisCRadi-BencteuxSTrestardLMarretSGrangeot-KerosLBuffet-JanvresseCCongenital rubella with bilateral cataract detected at 5 weeksActa Paediatr20049311155015513590
- MahalakshmiBThereseKLShyamalaGDevipriyaUMadhavanHNToxoplasma gondii detection by nested polymerase chain reaction in lens aspirate and peripheral blood leukocyte in congenital cataract patients: the first report from a tertiary eye hospital in IndiaCurr Eye Res2007327–865365717852189
- VijayalakshmiPKakkarGSamprathiABanushreeROcular manifestations of congenital rubella syndrome in a developing countryIndian J Ophthalmol200250430731112532496
- BeutlerEMatsumotoFKuhlWGalactokinase deficiency as a cause of cataractsN Engl J Med197328823120312064700553
- PohjolaSOcular manifestations of idiopathic hypoparathyroidismActa Ophthalmol (Copenh)196240325526514487411
- MerinSCrawfordJSHypoglycemia and infantile cataractArch Ophthalmol19718654954985165486
- HejtmancikJFCongenital cataracts and their molecular geneticsSemin Cell Dev Biol200819213414918035564
- CraigJEFriendKLGeczJA novel locus for X-linked congenital cataract on Xq24Mol Vis20081472172618431456
- PonnamSPRameshaKTejwaniSMataliaJKannabiranCA missense mutation in LIM2 causes autosomal recessive congenital cataractMol Vis2008141204120818596884
- IonidesAFrancisPBerryVClinical and genetic heterogeneity in autosomal dominant cataractBr J Ophthalmol199983780280810381667
- ChurchillAGrawJClinical and experimental advances in congenital and paediatric cataractsPhilos Trans R Soc Lond B Biol Sci201136615681234124921402583
- FrancisPJMooreATGenetics of childhood cataractCurr Opin Ophthalmol2004151101514743013
- GillDKloseRMunierFLGenetic heterogeneity of the Coppock-like cataract: a mutation in CRYBB2 on chromosome 22q11.2Invest Ophthalmol Vis Sci200041115916510634616
- BurdonKPMcKayJDWirthMGThe PITX3 gene in posterior polar congenital cataract in AustraliaMol Vis20061236737116636655
- HeYPanZLuoFA novel PAX6 mutation in Chinese patients with severe congenital aniridiaCurr Eye Res2012371087988322621390
- YasmeenARiazuddinSAKaulHAutosomal recessive congenital cataract in consanguineous Pakistani families is associated with mutations in GALK1Mol Vis20101668268820405025
- BurdonKPMcKayJDSaleMMMutations in a novel gene, NHS, cause the pleiotropic effects of Nance-Horan syndrome, including severe congenital cataract, dental anomalies, and mental retardationAm J Hum Genet20037351120113014564667
- ChoiJKimJHKimSJYuYSClinical characteristics, course, and visual prognosis of partial cataracts that seem to be visually insignificant in childrenJ AAPOS201216216116722525173
- BouzasAGAnterior polar congenital cataract and corneal astigmatismJ Pediatr Ophthalmol Strabismus19922942102121512660
- DrummondGTHinzBJManagement of monocular cataract with long-term dilation in childrenCan J Ophthalmol19942952272307859175
- BirchEESubramanianVPatelCCStagerDJrPreoperative visual acuity and contrast sensitivity in children with small, partial, or non-central cataractsJ AAPOS201317435736223993715
- ElstonJSTimmsCClinical evidence for the onset of the sensitive period in infancyBr J Ophthalmol19927663273281622940
- BirchEEStagerDRThe critical period for surgical treatment of dense congenital unilateral cataractInvest Ophthalmol Vis Sci1996378153215388675395
- BirchEEChengCStagerDRJrWeakleyDRJrStagerDRSrThe critical period for surgical treatment of dense congenital bilateral cataractsJ AAPOS2009131677119084444
- LambertSRDrackAVInfantile cataractsSurv Ophthalmol19964064274588724637
- HussainRNShahidFWoodruffGAxial length in apparently normal pediatric eyesEur J Ophthalmol201424112012323787457
- GordonRADonzisPBRefractive development of the human eyeArch Ophthalmol198510367857894004614
- WoodICHodiSMorganLLongitudinal change of refractive error in infants during the first year of lifeEye (Lond)19959Pt 55515578543071
- WilsonMETrivediRHChoice of intraocular lens for pediatric cataract surgery: survey of AAPOS membersJ Cataract Refract Surg20073391666166817720093
- TrivediRHWilsonMEPrediction error after pediatric cataract surgery with intraocular lens implantation: contact versus immersion A-scan biometryJ Cataract Refract Surg201137350150521333874
- FanDSRaoSKYuCBWongCYLamDSChanges in refraction and ocular dimensions after cataract surgery and primary intraocular lens implantation in infantsJ Cataract Refract Surg20063271104110816857495
- GrienerEDDahanELambertSREffect of age at time of cataract surgery on subsequent axial length growth in infant eyesJ Cataract Refract Surg19992591209121310476503
- LambertSRLynnMJDuBoisLGAxial elongation following cataract surgery during the first year of life in the Infant Aphakia Treatment StudyInvest Ophthalmol Vis Sci201253127539754523074203
- TrivediRHWilsonMEBandyopadhyayDRefractive shift in pseudophakic eyes during the second decade of lifeJ Cataract Refract Surg201238110210722153093
- MooreDBBen ZionINeelyDEAccuracy of biometry in pediatric cataract extraction with primary intraocular lens implantationJ Cataract Refract Surg200834111940194719006742
- MezerERootmanDSAbdolellMLevinAVEarly postoperative refractive outcomes of pediatric intraocular lens implantationJ Cataract Refract Surg200430360361015050256
- NeelyDEPlagerDABorgerSMGolubRLAccuracy of intraocular lens calculations in infants and children undergoing cataract surgeryJ AAPOS20059216016515838444
- NihalaniBRVanderVeenDKComparison of intraocular lens power calculation formulae in pediatric eyesOphthalmology201011781493149920466430
- NischalKKSoleboLRussell-EggittIPaediatric IOL implantation and postoperative refractive state: what role do study methodology and surgical technique play?Br J Ophthalmol201094552953120447961
- NihalaniBRVanderveenDKAccuracy of intraocular lens power calculation formulae in children less than two yearsAm J Ophthalmol2012154475976022995562
- VanderVeenDKNizamALynnMJPredictability of intraocular lens calculation and early refractive status: the Infant Aphakia Treatment StudyArch Ophthalmol2012130329329922411658
- VanderveenDKTrivediRHNizamALynnMJLambertSRPredictability of intraocular lens power calculation formulae in infantile eyes with unilateral congenital cataract: results from the Infant Aphakia Treatment StudyAm J Ophthalmol2013156612521260.e224011524
- LambertSRLynnMJHartmannEEComparison of contact lens and intraocular lens correction of monocular aphakia during infancy: a randomized clinical trial of HOTV optotype acuity at age 4.5 years and clinical findings at age 5 yearsJAMA Ophthalmol2014132667668224604348
- Abdel-HafezGTrivediRHWilsonMEBandyopadhyayDComparison of aphakic refraction formulas for secondary in-the-bag intraocular lens power estimation in childrenJ AAPOS201115532434
- MooreDBBen ZionINeelyDERobertsGJSprungerDTPlagerDARefractive outcomes with secondary intraocular lens implantation in childrenJ AAPOS200913655155420006814
- NihalaniBRVanderveenDKSecondary intraocular lens implantation after pediatric aphakiaJ AAPOS201115543544022108355
- ShenoyBHMittalVGuptaASachdevaVKekunnayaRRefractive outcomes and prediction error following secondary intraocular lens implantation in children: a decade-long analysisBr J Ophthalmol201397121516151923467789
- RamJJainVKAgarwalAKumarJHydrophobic acrylic versus polymethyl methacrylate intraocular lens implantation following cataract surgery in the first year of lifeGraefes Arch Clin Exp Ophthalmol201425291443144924947548
- RoweNABiswasSLloydICPrimary IOL implantation in children: a risk analysis of foldable acrylic v PMMA lensesBr J Ophthalmol200488448148515031160
- BastiSAasuriMKReddyMKHeparin-surface-modified intraocular lenses in pediatric cataract surgery: prospective randomized studyJ Cataract Refract Surg199925678278710374157
- PavlovicSJacobiFKGraefMJacobiKWSilicone intraocular lens implantation in children: preliminary resultsJ Cataract Refract Surg2000261889510646153
- BuckleyEGSafety of transscleral-sutured intraocular lenses in childrenJ AAPOS200812543143918706839
- AsadiRKheirkhahALong-term results of scleral fixation of posterior chamber intraocular lenses in childrenOphthalmology20081151677217481735
- JacobiPCDietleinTSJacobiFKScleral fixation of secondary foldable multifocal intraocular lens implants in children and young adultsOphthalmology2002109122315232412466177
- KamalAMHanafyMEhsanATomerakRHUltrasound biomicroscopy comparison of ab interno and ab externo scleral fixation of posterior chamber intraocular lensesJ Cataract Refract Surg200935588188419393888
- SminiaMLOdenthalMTWenniger-PrickLJGortzak-MoorsteinNVölker-DiebenHJTraumatic pediatric cataract: a decade of follow-up after Artisan aphakia intraocular lens implantationJ AAPOS200711655555817720570
- YenKGReddyAKWeikertMPSongYHamillMBIris-fixated posterior chamber intraocular lenses in childrenAm J Ophthalmol2009147112112618790471
- EpleyKDShainbergMJLuederGTTychsenLPediatric secondary lens implantation in the absence of capsular supportJ AAPOS20015530130611641640
- MorrisonDSternbergPDonahueSAnterior chamber intraocular lens (ACIOL) placement after pars plana lensectomy in pediatric Marfan syndromeJ AAPOS20059324024215956943
- CionniRJOsherRHMarquesDMMarquesFFSnyderMEShapiroSModified capsular tension ring for patients with congenital loss of zonular supportJ Cataract Refract Surg20032991668167314522284
- CristobalJARemonLDel BueyMAMontes-MicoRMultifocal intraocular lenses for unilateral cataract in childrenJ Cataract Refract Surg201036122035204020952155
- JacobiPCDietleinTSKonenWMultifocal intraocular lens implantation in pediatric cataract surgeryOphthalmology200110881375138011470687
- RamJAgarwalAKumarJGuptaABilateral implantation of multifocal versus monofocal intraocular lens in children above 5 years of ageGraefes Arch Clin Exp Ophthalmol2014252344144724441952
- Bar-SelaSMSpiererAAstigmatism outcomes of scleral tunnel and clear corneal incisions for congenital cataract surgeryEye (Lond)20062091044104816179936
- LamHYYenKGChange in astigmatism after temporal clear corneal cataract extraction in the pediatric populationOpen Ophthalmol J20082434519478907
- Bar-SelaSMSpiererOSpiererASuture-related complications after congenital cataract surgery: Vicryl versus Mersilene suturesJ Cataract Refract Surg200733230130417276274
- BartholomewLRWilsonMEJrTrivediRHPediatric anterior capsulotomy preferences of cataract surgeons worldwide: comparison of 1993, 2001, and 2003 surveysJ Cataract Refract Surg200733589390017466867
- GimbelHVNeuhannTDevelopment, advantages, and methods of the continuous circular capsulorhexis techniqueJ Cataract Refract Surg199016131372299571
- WilsonMEJrTrivediRHBartholomewLRPershingSComparison of anterior vitrectorhexis and continuous curvilinear capsulorhexis in pediatric cataract and intraocular lens implantation surgery: a 10-year analysisJ AAPOS200711544344617532240
- WoodMGSchelonkaLPA porcine model predicts that a can-opener capsulotomy can be done safely in pediatric patientsJ AAPOS19993635636210613580
- GrueterichMLackerbauerCAKampikAPerformance of the Acri. Smart 46S intraocular lens in pediatric microincision cataract surgeryJ Cataract Refract Surg200834459159518361980
- TrivediRHWilsonMEJrBartholomewLRExtensibility and scanning electron microscopy evaluation of 5 pediatric anterior capsulotomy techniques in a porcine modelJ Cataract Refract Surg20063271206121316857511
- NischalKKTwo-incision push-pull capsulorhexis for pediatric cataract surgeryJ Cataract Refract Surg200228459359511955896
- HamadaSLowSWaltersBCNischalKKFive-year experience of the 2-incision push-pull technique for anterior and posterior capsulorrhexis in pediatric cataract surgeryOphthalmology200611381309131416877070
- DickHBSchultzTFemtosecond laser-assisted cataract surgery in infantsJ Cataract Refract Surg201339566566823608565
- TitiyalJSSinhaRSharmaNVajpayeeRBPostage stamp multiple anterior capsulorhexisotomies in pediatric cataract surgeryBMC Ophthalmol20055315752433
- TehraniMDickHBKrummenauerFPfirrmannGBoyleTStoffelnsBMCapsule measuring ring to predict capsular bag diameter and follow its course after foldable intraocular lens implantationJ Cataract Refract Surg200329112127213414670421
- AmayaLTaylorDRussellINischallKPhacoaspiration in childrenJ Cataract Refract Surg200127101534153511687336
- DahanEIntraocular lens implantation in childrenCurr Opin Ophthalmol2000111515510724828
- DharmarajSAzarNControversies of implanting intraocular lenses in infancyInt Ophthalmol Clin2005454618116199967
- BayramlarHTotanYBorazanMHeparin in the intraocular irrigating solution in pediatric cataract surgeryJ Cataract Refract Surg200430102163216915474831
- SiatiriHBeheshtnezhadAHAsghariHSiatiriNMoghimiSPiriNIntracameral tissue plasminogen activator to prevent severe fibrinous effusion after congenital cataract surgeryBr J Ophthalmol200589111458146116234453
- VasavadaVAPraveenMRShahSKTrivediRHVasavadaARAnti-inflammatory effect of low-molecular-weight heparin in pediatric cataract surgery: a randomized clinical trialAm J Ophthalmol20121542252258.e422541652
- CheeKYLamGCManagement of congenital cataract in children younger than 1 year using a 25-gauge vitrectomy systemJ Cataract Refract Surg200935472072419304095
- StagerDRJrWeakleyDRJrHunterJSLong-term rates of PCO following small incision foldable acrylic intraocular lens implantation in childrenJ Pediatr Ophthalmol Strabismus2002392737611911547
- JensenAABastiSGreenwaldMJMetsMBWhen may the posterior capsule be preserved in pediatric intraocular lens surgery?Ophthalmology20021092324327 discussion 32811825817
- KugelbergMZetterströmCPediatric cataract surgery with or without anterior vitrectomyJ Cataract Refract Surg200228101770177312388026
- SainiJSJainAKSukhijaJGuptaPSarohaVAnterior and posterior capsulorhexis in pediatric cataract surgery with or without trypan blue dye: randomized prospective clinical studyJ Cataract Refract Surg20032991733173714522292
- PraveenMRShahSKVasavadaVATriamcinolone-assisted vitrectomy in pediatric cataract surgery: intraoperative effectiveness and postoperative outcomeJ AAPOS201014434034420637663
- GimbelHVDeBroffBMPosterior capsulorhexis with optic capture: maintaining a clear visual axis after pediatric cataract surgeryJ Cataract Refract Surg19942066586647837081
- VasavadaARTrivediRHSinghRNecessity of vitrectomy when optic capture is performed in children older than 5 yearsJ Cataract Refract Surg20012781185119311524188
- GrieshaberMCPienaarAStegmannRPosterior vertical capsulotomy with optic entrapment of the intraocular lens in congenital cataracts – prevention of capsule opacificationJ Cataract Refract Surg200531588689415975452
- ClearyCALaniganBO’KeeffeMIntracameral triamcinolone acetonide after pediatric cataract surgeryJ Cataract Refract Surg201036101676168120870112
- MataftsiADabbaghAMooreWNischalKKEvaluation of whether intracameral dexamethasone predisposes to glaucoma after pediatric cataract surgeryJ Cataract Refract Surg201238101719172322841425
- HuangYDaiYWuXLanJXieLToxic anterior segment syndrome after pediatric cataract surgeryJ AAPOS201014544444621035074
- MedsingeANischalKKCapsular blockage syndrome in a child: a case reportEye (Lond)201327111333133423928881
- TrivediRHWilsonMEJrGolubRLIncidence and risk factors for glaucoma after pediatric cataract surgery with and without intraocular lens implantationJ AAPOS200610211712316678745
- SimsekTMutluayAHElginUGurselRBatmanAGlaucoma and increased central corneal thickness in aphakic and pseudophakic patients after congenital cataract surgeryBr J Ophthalmol20069091103110616707519
- RabiahPKDuHHahnEAFrequency and predictors of retinal detachment after pediatric cataract surgery without primary intraocular lens implantationJ AAPOS20059215215915838443
- MilvertonEJIrrigation of the capsular bag using a sealed-capsule irrigation device and 5-fluorouracilEye (Lond)20092381746174718978726
- RekasMKluśAKosatkaMSealed-capsule irrigation with distilled deionized water to prevent posterior capsule opacification – prospective, randomized clinical trialCurr Eye Res201338336337023167738
- TassignonMJDe VeusterIGodtsDKosecDVan den DoorenKGobinLBag-in-the-lens intraocular lens implantation in the pediatric eyeJ Cataract Refract Surg200733461161717397732
- Baradaran-RafiiAShirzadehEEslaniMAkbariMOptical correction of aphakia in childrenJ Ophthalmic Vis Res201491718224982736
- ChenYCHuACRosenbaumASpoonerSWeissmanBALong-term results of early contact lens use in pediatric unilateral aphakiaEye Contact Lens2010361192519935425
- WrightKWMatsumotoEEdelmanPMBinocular fusion and stereopsis associated with early surgery for monocular congenital cataractsArch Ophthalmol199211011160716091444921
- ChakMWadeARahiJSLong-term visual acuity and its predictors after surgery for congenital cataract: findings of the British Congenital Cataract StudyInvest Ophthalmol Vis Sci200647104262426917003414
- KugelbergMShafieiKvan der PloegIZetterströmCIntraocular lens as a drug delivery system for dexamethasoneActa Ophthalmol201088224124419173684
- PortaliouDMKymionisGDPallikarisIGMulti-component adjustable intraocular lenses: a new concept in pediatric cataract surgeryJ Refract Surg2014301626624168786