Abstract
Leber hereditary optic neuropathy (LHON) is one of the most common inherited optic neuropathies causing bilateral central vision loss. The disorder results from point mutations in mitochondrial DNA and subsequent mitochondrial dysfunction. The primary cell type that is lost in LHON is the retinal ganglion cell, which is highly susceptible to disrupted ATP production and oxidative stress. Inheritance of LHON follows that of mitochondrial genetics, and it has a highly variable clinical phenotype, as other genetic and environmental factors also play a role. Although LHON usually presents with isolated vision loss, some patients suffer other neurological sequelae. For ill-defined reasons, male LHON mutation carriers are more affected than females. Most LHON patients remain legally blind, but a small proportion can experience spontaneous partial recovery, often within the first year of symptom onset. Unfortunately, at this time there are no established curative interventions and treatment is largely supportive. Patients should be offered low vision services and counseled on mitigating risk factors for additional vision loss, such as smoking and consuming alcohol. Encouraging treatments currently undergoing investigation includes ubiquinone analogs, such as idebenone, as well as gene therapy and stem cells to restore ATP synthesis and provide neuroprotection to surviving retinal ganglion cells.
Introduction
Mitochondrial diseases were once thought of as rare disorders, in part due to failure to recognize the diagnosis because of the wide variability among phenotypes. They are increasingly recognized as a common cause of neurologic and visual dysfunction. Ophthalmic manifestations are frequent among mitochondrial disorders and can result in retinopathy, ocular motility disorders, or optic neuropathy. It is important for ophthalmologists to remain cognizant of mitochondrial disease when a patient presents with vision loss. Among the mitochondrial diseases, Leber hereditary optic neuropathy (LHON) is often considered a prototypical disorder. It was the first mitochondrial disease to be recognized by Dr Albrecht von Graefe in 1858, but it was named after Dr Theodore Leber who described 15 patients with the disease among four families.Citation1 LHON was the first disorder recognized to be maternally inherited and the first to be attributed to a point mutation in mitochondrial DNA (mtDNA).Citation2,Citation3 Vision loss from LHON results from selective degeneration of retinal ganglion cells (RGCs), which are highly sensitive to mitochondrial dysfunction and metabolic insult.Citation4 The mechanisms involved in the pathogenesis of LHON continue to be elucidated, paving the way for research into potential therapeutic interventions.
Epidemiology
LHON is the most common optic neuropathy caused by a primary mutation in mtDNA.Citation5–Citation7 The minimum prevalence of vision loss due to the three most common pathogenic point mutations in LHON is one in 31,000 in the northern UK.Citation8 Other epidemiological studies report a prevalence of one in 39,000 and one in 50,000 in the Netherlands and Finland, respectively.Citation9,Citation10 LHON affects predominantly males (in 80%–90% of cases).Citation5 Symptom onset typically occurs in the second and third decades of life. LHON carriers rarely lose vision after the age of 50 years, but there have been reports of LHON onset from 2 to 87 years of age.Citation5,Citation7,Citation11,Citation12 Most LHON patients are aware of a family member with LHON-compatible vision loss, although 40% deny a known family history. Given that de novo mutations are rare, this relatively high percentage without a family history could be attributable to unrecognized mutation carriers in the family who had never lost vision or to the innate difficulty in accurately tracing family history.Citation8,Citation13
Clinical features of vision loss
LHON usually presents as painless, subacute, central visual loss in one eye. Weeks to months later, the second eye becomes involved, with a median delay of 6–8 weeks.Citation7,Citation14 Within 1 year, 97% of those affected have involvement of the second eye, such that a patient presenting with a unilateral optic neuropathy for longer than 1 year is highly unlikely to suffer from LHON-related vision loss.Citation5,Citation12,Citation15 Approximately 25% have bilateral simultaneous vision loss, but in some individuals it may be that vision loss in the first eye is not noticed before the second eye becomes involved.Citation5,Citation12,Citation14
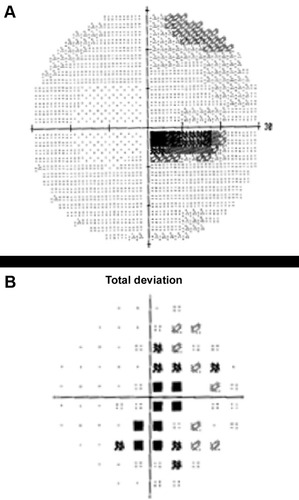
The majority of individuals progress to a visual acuity of 20/200 or worse.Citation16 Due to preferential involvement of the papillomacular bundle, the earliest visual field abnormality is a cecocentral scotoma (), which can enlarge to become a larger central defect.Citation16 Dyschromatopsia is common and usually parallels the degree of visual acuity loss.Citation5,Citation12,Citation16 Pupillary light reflexes usually remain intact due to relative sparing of melanopsin-containing RGCs. This subset of RGCs are thought to be more resistant to metabolic insult from mitochondrial dysfunction when compared with all RGCs.Citation4,Citation17,Citation18 In cases of asymmetric bilateral or monocular vision loss, however, a relative afferent pupillary defect can occur.Citation19
Figure 1 Automated 30-2 protocol Humphrey visual field study of the right eye showing a dense cecocentral scotoma on the grayscale (A) and total deviation map (B) in a patient with acute LHON-related vision loss.
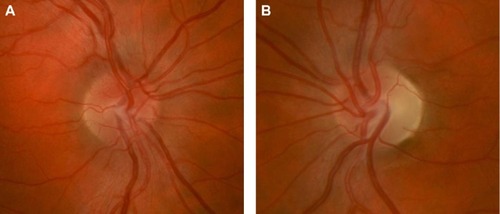
On fundus examination preceding or during the acute stage of vision loss, there can be characteristic findings, including optic disc hyperemia, peripapillary telangiectatic blood vessels, vascular tortuosity, and swelling of the retinal nerve fiber layer (RNFL) around the optic disc () without corresponding leakage on fluorescein angiography (sometimes termed “pseudoedema”). The fundus can look normal in 20%–40% of those in the active stage of vision loss, which can delay diagnosis.Citation12,Citation20,Citation21 Eventually, as the disease progresses, disc hyperemia, peripapillary telangiectasias, and pseudoedema resolve. Approximately 6 weeks after onset of vision loss, optic disc pallor develops and can be accompanied by cupping of the optic disc, reflecting the death of RGCs that occurs in the chronic atrophic phase ().Citation5,Citation22
Figure 2 Right optic nerve (A) of a patient with acute LHON-related vision loss showing mild hyperemia, blurring of the disc margin, and elevation of the optic nerve head from swelling of the peripapillary retinal nerve fiber layer. LHON-related vision loss in the left eye had occurred 6 months prior leading to prominent temporal optic nerve pallor (B) from atrophy of the retinal nerve fiber layer.
Fundus changes seen in LHON can be further characterized and quantified through optical coherence tomography. In the acute phase, the RNFL thickens first in the temporal and inferior quadrants, then the superior and nasal quadrants.Citation23 This is consistent with early preferential involvement of the papillomacular bundle of RGCs. RNFL thickening is related to axonal swelling from impaired mitochondrial function and axonal transport.Citation4 The RNFL then becomes thinned during the chronic phase in the months following the onset of vision loss.Citation24 Macular thickness may thin before the RNFL, suggesting that disease progression could be better monitored with both macular thickness and RNFL measurements by optical coherence tomography.Citation25
Visual evoked potentials (VEPs) and electroretinograms (ERGs) are often abnormal in affected LHON patients, as they reflect optic nerve fiber degeneration and RGC loss, respectively. In a study of two brothers with LHON who had normal VEP latencies and configurations prior to the onset of symptoms, earliest abnormalities included prolonged VEP latency and abnormal VEP morphology. With symptom progression, there was a progressive prolongation of VEP latency.Citation26 In a Brazilian family with a strong history of LHON, three affected members had increased latencies, decreased amplitudes, or absent responses for pattern-reversal VEP. Two family members also had reduced ERG cone responses.Citation27 Another study found that affected LHON patients had increased VEP latency and decreased VEP amplitude that was associated with a decreased pattern ERG N50–N95 amplitude.Citation28 Notably, VEPs were normal in unaffected carriers in these studies. VEPs and ERGs can therefore be useful in diagnosing and monitoring disease progression in affected patients.
Magnetic resonance images of the brain and orbits are usually normal in affected LHON patients.Citation29 There are, however, reports of patients with non-specific increased signal in the retrobulbar optic nerve on T2-weighted fast spin echo and short time inversion recovery sequences months after vision loss.Citation30,Citation31 Intravenous gadolinium magnetic resonance imaging contrast leads to optic nerve enhancement in pathologic states in which there is disruption of the blood–brain barrier within the optic nerve.Citation32 Patients with LHON have rarely demonstrated optic nerve enhancement on post-contrast images, suggesting that in some cases there may be an inflammatory component to the pathogenesis of LHON.Citation32
Interestingly, unaffected LHON point mutation carriers can display subclinical signs of disease on fundus examination, including peripapillary microangiopathy, zones of mild disc pseudoedema, and telangiectasias.Citation33 Some seemingly asymptomatic carriers do exhibit subclinical dyschromatopsia.Citation34 Among asymptomatic carriers, temporal RNFL thickening on optical coherence tomography may be present, further highlighting early involvement of the papillomacular bundle in subclinical LHON.Citation35 One study that recorded the pattern ERG in asymptomatic LHON mutation carriers showed a significant decline in N95 amplitude by ~40% from baseline over 36 months, suggesting that subclinical RGC loss is progressive in unaffected carriers and precedes the onset of visual field defects.Citation36 Pattern ERG may therefore be a useful tool to monitor subclinical disease progression in LHON mutation carriers.
Prognosis
The visual prognosis in LHON is poor. Most individuals have permanent vision loss and are legally registered as visually impaired.Citation37 Although vision loss is unlikely to progress after the active phase of the disease, patients report that the acute phase vision loss has a strong negative impact on quality of life.Citation37 Spontaneous visual improvement is a well described phenomenon in LHON, usually occurring within the first year following vision loss. Recovery can also occur decades later.Citation5 Recovery typically presents first with the appearance of small islands of vision within the central defect bilaterally.Citation20,Citation21 Spontaneous visual recovery is more common in patients with the 14484 mutation, with a partial recovery rate of 37%–58%, while the 11778 mutation has the lowest partial recovery rate of 4%.Citation7,Citation8,Citation14,Citation38 Patients with the 3460 mutation have an intermediate prognosis, with an approximate 20% partial recovery rate.Citation39 Earlier age of onset (younger than 20 years), a subacute time course of vision loss, and a larger optic disc are all associated with a better visual prognosis.Citation24,Citation40,Citation41
Mitochondrial function and oxidative phosphorylation
Mitochondria are double-membraned intracellular organelles present in nucleated eukaryotic cells that play a vital role in energy generation through production of ATP used for cell growth and function.Citation42,Citation43 The number of mitochondria present in a particular cell type depends on the energy demands of the cell. Cells in highly metabolically active tissues, including RGCs within the papillomacular bundle, the cardiac conduction system, pancreas, kidney, liver, and muscle, have high ATP requirements and high numbers of mitochondria. Therefore, mitochondrial diseases predominantly affect these tissues, as they are most susceptible to disrupted ATP production.Citation4,Citation44,Citation45
ATP generation occurs via oxidative phosphorylation (OXPHOS) through the mitochondrial respiratory chain. The respiratory chain is made of five complexes (I–V) embedded in the inner membrane. Complexes I–IV oxidize NADH and FADH2 generated from glycolysis and beta-oxidation of fatty acids. Complex V, also known as ATP synthase, then pumps protons into the intermembrane space and generates an electrochemical gradient that facilitates phosphorylation of ADP to ATP. Several cofactors, including ubiquinone, play an important role in shuttling electrons between respiratory chain complexes.Citation4,Citation15,Citation45–Citation47
While ATP production is an essential task of mitochondria, the organelles also play other vital roles for the cell, including detoxification of reactive oxygen species (ROS), iron metabolism, fatty acid oxidation, amino acid biosynthesis, and regulation of cellular apoptosis.Citation4,Citation48 Although dysfunction of the OXPHOS pathway is one of the most important factors in the pathogenesis of mitochondrial diseases, defects of other cofactors or in the cell machinery that assembles mitochondrial components can also disrupt the ATP supply and increase production of ROS, which can have devastating effects on cells.
Mitochondrial genetics
The genetics of the mitochondria reflect the organelle’s evolutionary origins; autonomous proto-mitochondrial prokaryotic organisms were thought to be phagocytosed by larger eukaryotic cells, forming an endosymbiotic relationship in which the proto-mitochondria supplied ATP and detoxified ROS for the eukaryotic cell.Citation48,Citation49 Similar to their proposed prokaryotic origin, mitochondria also have a genome in the form of circular double-stranded mtDNA. Importantly, mitochondria rely heavily on nuclear DNA to encode proteins required for mitochondrial function. More than 80 subunits required for the OXPHOS system are encoded in the nuclear genome and are imported into mitochondria.Citation4 Diseases with mutations in the nuclear genome often follow Mendelian inheritance (eg, autosomal dominant, autosomal recessive, or X-linked inheritance). In contrast, those with primary mutations in mtDNA have unique patterns of inheritance and penetrance governed by the principles of maternal inheritance, heteroplasmy, replicative segregation, and the critical threshold.Citation50
Transmission of the mitochondrial genome occurs from a mother to her progeny. There is no paternal contribution, as the few mitochondria present in sperm are proteolytically destroyed by the zygote.Citation51 Therefore, LHON results when a mother carrying the mutation transmits it to her children, while fathers cannot transmit the mutation to offspring.
Unlike nuclear DNA, mtDNA replicates continuously and independently of the cell cycle in both dividing and non-dividing cells. Often there are several thousands of mtDNA molecules present, and all copies are identical. This is called homoplasmy. However, a mutation can arise in one copy of mtDNA, resulting in coexistence of both mutant and wild-type mtDNA within a mitochondrion, termed heteroplasmy.Citation45 The principle of heteroplasmy is critical when host cells divide and the mitochondria are separated between daughter cells. This process is termed replicative segregation and occurs stochastically. The proportion of mutant and wild-type mtDNA between daughter cells is subject to random segregation and therefore unequal. Heteroplasmy and replicative segregation contribute to the heterogeneity of mitochondrial disease phenotypes, even among related individuals.
In the case of heteroplasmy, a certain amount of wild-type mtDNA can compensate for the mutant mtDNA in a cell or tissue. If the effects of the mutant mtDNA exceed a certain threshold, however, the wild-type mtDNA can no longer compensate. This critical threshold level is often tissue-specific; metabolically active tissues, particularly the RGCs, which constitute the optic nerve and the cells of the retinal pigment epithelium, have a lower threshold than less metabolically active tissues.Citation52 In addition, post-mitotic cells like neurons accumulate more mutant mtDNA copies over time, which eventually exceed the critical threshold and account for the age-dependent expression of many mitochondrial diseases.Citation44
Over 200 point mutations in mtDNA account for mitochondrial diseases. Most point mutations that cause disease are heteroplasmic. However, there are several exceptions, including the common mutations in LHON, which are usually homoplasmic. Deletions and duplications in mtDNA can also lead to mitochondrial diseases including mitochondrial myopathies, which are often sporadic.Citation15,Citation45,Citation53
Genetics and incomplete penetrance of LHON
Ninety percent of all cases of LHON are due to one of three point mutations in mtDNA, which are located at nucleotide positions 3460, 11778, and 14484.Citation5 The most common point mutation is 11778, which accounts for 70% of all cases.Citation5 The 14484 and 3460 mutations account for ~14% and ~13%, respectively.Citation20,Citation50 An exception is among those of French Canadian descent, in which the 14484 mutation accounts for about 90% of cases within that population due to a founder effect.Citation54 Other relatively rare mutations have also been discovered but occur in single families.Citation20,Citation21 All of the mutations occur in genes encoding subunits for complex I in the respiratory chain, particularly in those encoding the ND1 and ND6 subunits.Citation55,Citation56
LHON is notable for incomplete penetrance, meaning that not all mutation carriers will develop vision loss. While the mechanisms involved have not been fully elucidated, it appears that complex genetic and environmental factors play a role.
Like several other mitochondrial disorders, heteroplasmy is thought to influence the penetrance of LHON. For instance, it has been observed that offspring born to mothers with less than 80% mutated mtDNA present in their blood are less likely to be symptomatic than offspring born to homoplasmic mothers.Citation57 Even more variability is present because tissue-specific segregation of mutant mtDNA is stochastic during embryogenesis. Considering that 80%–90% of all LHON individuals carry homoplasmic mutations, heteroplasmy alone does not explain the incomplete penetrance of LHON.Citation8,Citation14
Another risk factor for vision loss is the set of inherited genes that commonly segregate with the pathogenic mtDNA mutation. Over the course of evolution, mtDNA polymorphisms have clustered together in groups called haplogroups, which tend to be inherited together. The other polymorphisms present within a haplogroup can have deleterious effects on the OXPHOS pathway, including decreased levels of protein synthesis and ATP production, which could then synergize with the deleterious effect of the primary LHON mutation.Citation58,Citation59 For instance, among Caucasians, haplogroup J is associated with increased penetrance for the 11778 and 14484 mutation carriers, while haplogroup K is associated with increased penetrance for the 3460 mutation carriers.Citation60 Chinese carriers of the 11778 mutation had an increased risk of vision loss when inherited with haplogroup M7b1′2 and a decreased risk with haplogroup M8a.Citation61
Differences in mitochondrial mass have also been postulated to play a role in the incomplete penetrance of LHON. Unaffected LHON mutation carriers have significantly higher mtDNA copy numbers in leukocytes than affected mutation carriers. Comparison of fibroblasts from unaffected, affected, and control patients has shown that cells from unaffected carriers have increases in mitochondrial transcripts, respiratory chain proteins, enzyme activity, and mitochondrial biogenesis factors relative to controls and affected carriers. Higher levels of mtDNA in leukocytes in unaffected carriers were also associated with milder signs of ocular pathology. Thus, mitochondrial mass increases in unaffected carriers may be protective, whereby the increased amount of mitochondria can compensate for complex I dysfunction. Although the specific factors that activate mitochondrial biogenesis remains to be discovered, these observations could have implications for the treatment of LHON.Citation62
LHON is maternally inherited. Men cannot transmit the mutation. Both male and female offspring can, however, inherit the mutation, yet 50% of males and only 10% of females experience vision loss; this sex predilection cannot be explained solely by the principles of mitochondrial inheritance.Citation7 It has been hypothesized that there is a recessive X-linked susceptibility gene that works in concert with the mitochondrial mutation, which could explain the male predominance among carriers who lose vision. Those female carriers who do lose vision may either have homozygosity at the X-linked locus or may have experienced an unfortunate X chromosome inactivation.Citation63 Recent linkage analyses have discovered a region on the long arm of the X chromosome that may contain the susceptibility gene, but the actual gene responsible has not yet been identified.Citation64–Citation66
Hormonal differences between males and females have also been hypothesized to influence the male predominance in LHON. In females, estrogens are thought to modify the severity of mitochondrial dysfunction, including defective ATP synthesis, oxidative stress, and apoptosis. In cybrid cell lines containing homoplasmic LHON mutations, addition of 17β-estradiol led to activation of mitochondrial biogenesis, increased superoxide dismutase 2 (SOD2) activity, decreased production of ROS, and reduction of apoptosis. Estrogen receptor β was also shown to be particularly abundant in RGCs and their axons within the RNFL.Citation67 The data obtained from the cybrid cell model may approximate the effects of estrogen on the in vivo target tissue affected in LHON.
Environmental factors have been implicated as contributing to vision loss in LHON mutation carriers. Alcohol consumption and tobacco smoking have been associated with the onset of vision loss in those genetically predisposed to LHON. A retrospective study of 125 European LHON pedigrees showed an association between smoking and vision loss, in which heavy smokers were more likely to experience vision loss than light smokers.Citation68 The study showed a 93% penetrance of vision loss in male smokers versus a 66% penetrance in male non-smokers. Cigarette smoke can compromise complex I activity, reduce cytochrome c oxidase activity, and increase production of ROS. Heavy alcohol intake was also associated with a greater likelihood of vision loss, but this relationship was less significant than that of smoking. Other associated environmental triggers include head trauma, industrial toxins, and drugs that have mitochondrial toxicity, such as antiretrovirals and ethambutol.Citation20 Nutritional deficiencies have also been implicated as a trigger for vision loss in LHON carriers, including low vitamin B12 levels.Citation69
Optic nerve vulnerability
In LHON, RGCs appear to be selectively vulnerable to mitochondrial dysfunction. The papillomacular bundle of RGCs responsible for central vision is affected first and more severely because of its small-diameter fibers and heavy dependence on mitochondria.Citation70 Studies of RGC axons show mitochondrial clustering in the prelaminar nerve fiber layer, and mitochondria significantly decrease in number posterior to the lamina cribrosa where the axons are myelinated. Such an uneven distribution of mitochondria partly explains why the unmyelinated portion of RGC axons is particularly affected.Citation71–Citation73 It is unclear whether the precipitation of RGC loss is due to low ATP production, increased production of ROS, or both, and there are data that support both mechanisms.Citation74 A mouse mtDNA mutant model was developed that expressed key features of LHON, including degeneration of the papillomacular bundle, axonal swelling, and dysmorphic mitochondria in unmyelinated segments. There was no reduction in ATP synthesis, but there was increased ROS production; this research suggests that oxidative stress plays a larger role in the pathogenesis of LHON than defective ATP production.Citation75
Of note, optic neuropathy can occur in other mitochondrial disorders that have prominent systemic manifestations, such as myoclonic epilepsy with ragged red fibers, mitochondrial encephalomyopathy, lactic acidosis, and stroke-like episodes (MELAS), Leigh syndrome, Friedreich ataxia, Mohr–Tranebjerg syndrome, and complicated hereditary spastic paraplegia. It remains unclear why mitochondrial mutations in other disorders lead to a phenotype with systemic disease. With time, it has become more apparent that LHON can be associated with other non-visual neurologic sequelae.Citation76
LHON plus
While the typical manifestation of LHON is vision loss, there have been other manifestations reported within select pedigrees. Cardiac arrhythmias, peripheral neuropathies, dystonia, and myoclonus can occur in LHON carriers.Citation20 Some families from Holland, Australia, and North America have particularly severe manifestations, including ataxia, juvenile onset encephalopathy, spastic dystonia, and psychiatric disturbances. These phenotypes have been called “LHON plus syndromes” and have been linked to other mtDNA point mutations that affect OXPHOS complex I activity but differ from the three commonly seen in LHON.Citation20,Citation77,Citation78
An association between the 11778 mutation in LHON and a demyelinating syndrome that is radiologically and clinically identical to multiple sclerosis was described in 1992 and named Harding syndrome after the reporting author.Citation79 This posed an interesting hypothesis that vision loss in LHON may be caused by an abnormal immune response against the optic nerve because of mtDNA mutations. In females with the 11778 mutation, this immune response may involve other myelinated axons and result in a disorder indistinguishable from multiple sclerosis. It also poses the question of whether mitochondrial genes contribute to susceptibility to multiple sclerosis. Some report that the co-occurrence of LHON mutations and multiple sclerosis is likely due to chance and note that those patients present with atypical symptoms of LHON, in which there is a higher female predominance and persisting unilateral vision loss.Citation80 Others report a risk 50 times greater than expected for developing both multiple sclerosis and LHON, but given the rarity of the syndrome, much more remains to be elucidated.Citation81
Treatment
Symptomatic and supportive treatments
The treatment of mitochondrial disorders is still in its infancy. Even though there is promising research underway, the mainstay of clinical treatment for LHON remains supportive rather than curative. Low vision aids can be of substantial benefit for those with central vision loss from LHON.Citation82 In addition, low vision rehabilitation is a viable option because most LHON patients are young adults with intact peripheral vision. Patients should also be counselled to optimize environmental risk factors for vision loss by avoiding tobacco use, heavy alcohol consumption, medications with mitochondrial toxicity, and exposure to environmental toxins.Citation20,Citation68 Other supportive measures, particularly for the LHON plus syndromes, includes screening for extraocular manifestations of LHON, such as a screening electrocardiogram and neurological surveillance.Citation83
Nutritional supplements
Several combinations of vitamins (eg, B2, B3, B12, C, E, and folic acid) and other supplements such as alpha-lipoic acid, carnitine, creatine, L-arginine, and dichloroacetate have been tried to treat mitochondrial disorders, including LHON. However, analyses have shown little proof of efficacy with these interventions.Citation83,Citation84 The rarity of mitochondrial disorders makes it particularly challenging to determine efficacy. One review noted that only 35 of 1,039 publications had trials with more than five patients.Citation85
Brimonidine
Brimonidine is a topical α2-agonist that is used to manage patients with glaucoma. Brimonidine has been shown to be antiapoptotic, and it can protect RGCs from oxidative damage in animal models.Citation86 Nine patients with monocular vision loss were treated with topical brimonidine in an open-label trial to prevent vision loss in the other eye. However, the study was stopped prematurely because all of the patients experienced vision loss in their second eye, and brimonidine did not appear to mitigate the amount of vision loss.Citation87 Nonetheless, there are reports of patients who had both glaucoma and LHON in which vision loss was accelerated or worse than expected with either disorder alone. It has been proposed that increased intraocular pressure may further exacerbate axoplasmic stasis in RGCs already under high metabolic stress.Citation88 Brimonidine could therefore be potentially useful in asymptomatic LHON carriers with glaucoma due to its pressure-lowering effects and putative neuroprotective effects.
Ubiquinone analogs
Ubiquinone is a molecule in the mitochondrial membrane that carries electrons from complexes I and II to complex III. LHON mtDNA mutations affect complex I, so the ubiquinone analog coenzyme Q10 is thought to help facilitate the flow of electrons and maximize the electrons shuttled to complex III. It has long been used in attempts to treat mitochondrial disorders, yet recent analyses have not shown significant benefit.Citation83–Citation85 Given that coenzyme Q10 is highly lipophilic, it is unlikely that oral administration allows for delivery to mitochondria.
Idebenone and EPI-743 are short-chain ubiquinone analogs that easily enter the brain and reach mitochondria, unlike coenzyme Q10. Idebenone has been shown to bypass complex I and maintain ATP production, and it inhibits lipid peroxidation to protect mitochondria from oxidative damage.Citation89,Citation90 Idebenone was initially successful in 1992 with a 10-year-old boy who had the 11778 mutation, but this is confounded by the fact that childhood-onset LHON has higher rates of spontaneous recovery.Citation40,Citation91 A randomized, double-blind, placebo-controlled trial called RHODOS (Rescue of Hereditary Optic Disease Outpatient Study) enrolled 85 LHON patients who had a disease duration of up to 5 years. After 24 weeks of idebenone 900 mg/day, the study did not show any benefit for the primary outcome of best recovery of visual acuity after 24 weeks. However, the data showed a positive trend for the secondary end points, including change from baseline in best visual acuity and change in visual acuity for both eyes, particularly for patients with discordant visual acuities.Citation92 The study also found the largest treatment effect for patients with the 11778 or 3460 mutation, while those with the 14484 mutation had a high spontaneous recovery rate in the placebo group, thought to abolish any treatment effect. In the observational follow-up study (RHODOS-OFU), 59 of the original patients were followed up 30 months later, and those who were treated with idebenone still showed beneficial effects, especially those who had a short disease history.Citation93 In a retrospective study of 103 LHON patients, 44 patients with disease onset within one year were treated with idebenone and followed for 5 years or more. Those treated with idebenone recovered vision more than the control cohort, and the improvement was more prominent with early initiation of treatment and longer duration of treatment.Citation94 Another randomized, double-blind, placebo-controlled trial of 39 LHON patients with a disease duration of less than 5 years treated patients with idebenone 900 mg/day for 24 weeks. The treatment group showed improvement in blue-yellow color vision and less impairment of red-green color vision, and this effect was more prominent in those younger than 30 years of age and with less than 1 year of symptoms.Citation95 These trials show promise, but more research is needed to determine the optimal idebenone dose and treatment duration, as well as whether asymptomatic carriers and those with long disease duration can be treated. While not as widely studied as idebenone, EPI-743 was used in a trial including five patients with a disease duration of 90 days, and four of the five patients showed disease arrest and reversal after treatment for a minimum of 1 year.Citation96
Pharmacologic activators of mitochondrial biogenesis
As noted previously, increased mitochondrial biogenesis is significantly associated with unaffected LHON mutation carriers and may have a protective effect.Citation62 Mitochondrial biogenesis is partly regulated by the transcriptional activator PGC-1α, which is controlled by peroxisome proliferator-activated receptors and AMP-activated protein kinase.Citation97 Pharmacologic activators of these proteins include fibrates, rosiglitazone, metformin, and AICAR (5-aminoimidazole-4-carboxamide ribonucleoside).Citation98 In a mouse model of mitochondrial myopathy treated with bezafibrate, there was increased mitochondrial biogenesis, a delay in onset of the myopathy, and a longer life span.Citation99 However, it remains to be seen whether pharmaceutical activation of PGC-1α will be beneficial for affected LHON patients or mutation carriers.
Gene therapy
Gene therapy has shown some promise for mitochondrial diseases. For LHON in particular, it is an even more appealing treatment option because the RGC layer in the retina can be easily accessed. However, the ability to introduce genes directly into the mitochondrial genome has not been well developed, and a large obstacle is the double membrane of the mitochondrion. Thus, researchers have utilized allotopic expression by transfecting the desired gene into the nuclear genome instead.Citation100–Citation102 For this technique, the desired wild-type gene is engineered with a mitochondria-specific targeting sequence so that the wild-type protein product is imported into the mitochondria. The gene is then transfected into the nucleus with an adeno-associated virus (AAV) vector. One of the first successful attempts in vitro was on a cybrid cell line that was homoplasmic for the 11778 mutation, in which researchers used allotopic expression to complement the mutated ND4 subunit with a wild-type one, and rescued ATP synthesis.Citation103 Two animal models expressing the mutated ND4 subunit also showed an improvement in vision and rescue of RGCs following intravitreal injection and allotopic expression of the wild-type gene for ND4.Citation104,Citation105 However, limitations remain due to inefficient mitochondrial import of the hydrophobic ND4 subunit, and allotopic expression can be optimized by targeting the mRNAs to the mitochondrial surface to couple translation and translocation for a longer duration of gene expression.Citation106 Clinical trials associated with the University of Miami, Huazhong University of Science and Technology, and Gensight Biologics are currently recruiting patients with the 11778 mutation to assess the safety of gene therapy with an AAV vector carrying the wild-type ND4 gene.Citation107–Citation109
Another gene that has been allotopically expressed in cells harboring the 11778 mutation is the SOD2 gene, which detoxifies free radicals in mitochondria. Even though the SOD2 gene is encoded in the nuclear genome and expressed in LHON carriers, SOD2 activity is attenuated in cells homoplasmic for an LHON mutation.Citation110 In LHON cybrids, overexpression of SOD2 through transfection with an AAV vector led to a decreased rate of apoptosis, which highlights how antioxidant mechanisms could improve RGC survival in LHON.Citation111
More recent approaches have shown that it is possible to introduce genes into mitochondria, although it remains technically difficult. One study isolated whole mtDNA from healthy human donors and developed a construct with recombinant mitochondrial transcription factor A protein that could gain direct entry into mitochondria. This construct was then applied to LHON cybrids that were homoplasmic for the 11778 mutation, and it stimulated mitochondrial biogenesis.Citation112 Another study used a mitochondrial targeting sequence on the AAV vector capsid that contained the wild-type ND4 gene. The mitochondrial targeting sequence led to direct introduction of the wild-type ND4 gene into mitochondria in vitro and in a mouse model, in which there was restoration of ATP synthesis.Citation113 The same researchers then discovered that the mitochondrial targeting sequence-guided gene construct did not recombine with the host mitochondrial genes but rather remained episomal in the mitochondria.Citation114 This discovery is encouraging, as it appears unlikely that the gene construct recombines with endogenous genes, which could further disrupt the OXPHOS pathway. These studies show immense therapeutic potential, but research remains preliminary and further studies are required to evaluate adverse effects and determine how long the beneficial effects would last.
Stem cells
The use of stem cells to treat mitochondrial optic neuropathies is still in the preliminary stages, but two techniques are currently under investigation. One technique involves transplantation of RGCs. However, harvesting mature and fully functioning RGCs from embryonic stem cells or induced pluripotent stem cells remains challenging, and is further compounded by the difficulty in ensuring that transplanted RGCs make the correct neuronal connections when integrated into the retina.Citation115 For now, it appears that mature RGCs derived from stem cells can be used for further in vitro research of LHON pathogenesis and potential treatments.
Also under current investigation is the use of stem cells to provide neurotrophic factors that protect RGCs.Citation116 Because some patients with LHON experience visual recovery, they have some RGCs that survive despite mitochondrial dysfunction and oxidative stress. To protect these surviving RGCs, use of mesenchymal stem cells that secrete neurotrophic factors and anti-inflammatory cytokines appears promising. Intravitreal injection of autologous mesenchymal stem cells in a rat model with glaucoma showed a neuroprotective effect with increased RGC axon survival.Citation117 Another study used intravenous infusions of autologous bone-marrow derived mesenchymal stem cells in ten patients with secondary progressive multiple sclerosis, who experienced an improvement in visual acuity and an increase in optic nerve area without significant adverse effects.Citation118 Given this proof-of-concept study, the same strategy could be employed in the future to slow the loss of RGCs in LHON. Patients should be cautioned that lucrative, unregulated stem cell treatments offered at clinics not affiliated with academic research centers may make inflated promises of efficacy and could be dangerous.
Conclusion
LHON remains the prototype mitochondrial optic neuropathy and is marked by acute onset of sequential bilateral optic neuropathy due to point mutations in mtDNA. Symptom onset typically begins in the second or third decade of life as a painless and subacute monocular loss of central vision that then progresses to involve the other eye. While partial visual recovery may occur, most patients remain legally blind and require low vision services. Optic nerve degeneration results from dysfunctional OXPHOS and increased production of ROS within mitochondria, and RGCs within the papillomacular bundle serving central vision are particularly susceptible to oxidative stress. The LHON inheritance pattern follows that of mitochondrial genetics and is maternally inherited. Incomplete penetrance occurs as a result of both genetic and environmental factors, leading to wide symptom variability among mutation carriers.
Although research for LHON is ongoing and new discoveries are continuously made, many questions remain to be answered before a curative treatment becomes first-line therapy for patients with this debilitating disease. In vitro cell studies and animal models have shown promise, and now the field is progressing to early phase clinical trials. At this point, however, the efficacy, adverse effects, and duration of treatment benefit have yet to be determined.
Disclosure
The authors report no conflicts of interest in this work.
References
- LeberTUeber hereditäre und congenital-angelegte Sehnervenleiden [About hereditary and congenital optic nerve disorders]Albrecht Von Graefes Arch Klin Exp Ophthalmol187117249291 German
- WallaceDA new manifestation of Leber’s disease and a new explanation for the agency responsible for its unusual pattern of inheritanceBrain1970931211325418396
- WallaceDSinghGLottMMitochondrial DNA mutation associated with Leber’s hereditary optic neuropathyScience1988242142714303201231
- CarelliVRoss-CisnerosFNSadunAMitochondrial dysfunction as a cause of optic neuropathiesProg Retin Eye Res200423538914766317
- NewmanNJHereditary optic neuropathies: from the mitochondria to the optic nerveAm J Ophthalmol200514051752316083845
- Riordan-EvaPNeuro-ophthalmology of mitochondrial diseasesCurr Opin Opthalmol200011408412
- Yu-Wai-ManPGriffithsPGHudsonGChinneryPFInherited mitochondrial optic neuropathiesJ Med Genet20094614515819001017
- ManPGriffithsPBrownDThe epidemiology of Leber hereditary optic neuropathy in the North East of EnglandAm J Hum Genet20037233333912518276
- SpruijtLKolbachDNde CooRFInfluence of mutation type on clinical expression of Leber hereditary optic neuropathyAm J Ophthalmol200614167668216564802
- PuomilaAHämäläinenPKiviojaSEpidemiology and penetrance of Leber hereditary optic neuropathy in FinlandEur J Hum Genet2007151079108917406640
- GiraudetSLamirelCAmati-BonneauPNever too old to harbour a young man’s disease?Br J Ophthalmol20119588789620675733
- Riordan-EvaPHardingADa CostaJSandersMGovanGSweeneyMThe clinical features of Leber’s hereditary optic neuropathy defined by the presence of a pathogenic mitochondrial DNA mutationBrain1995118Pt 23193377735876
- BiousseVBrownMNewmanNDe novo 14484 mitochondrial DNA mutation in monozygotic twins discordant for Leber’s hereditary optic neuropathyNeurology199749113611389339703
- HardingASweeneyMPedigree analysis in Leber hereditary optic neuropathy families with a pathogenic mtDNA mutationAm J Hum Genet19955777867611298
- DiMauroSSchonEAMitochondrial disorders in the nervous systemAnnu Rev Neurosci2008319112318333761
- NewmanNJBiousseVNewmanSAProgression of visual field defects in Leber hereditary optic neuropathy: experience of the LHON treatment trialAm J Ophthalmol20061411061106716765674
- La MorgiaCRoss-CisnerosFNSadunAAMelanopsin retinal ganglion cells are resistant to neurodegeneration in mitochondrial optic neuropathiesBrain2010133Pt 82426243820659957
- MouraALANagyBVLa MorgiaCThe pupil light reflex in Leber’s hereditary optic neuropathy: evidence for preservation of melanopsin-expressing retinal ganglion cellsInvest Ophthalmol Vis Sci2013544471447723737476
- JacobsonDMStoneEMMillerNRRelative afferent pupillary defects in patients with Leber hereditary optic neuropathy and unilateral visual lossAm J Ophthalmol19981262912959727524
- Yu-Wai-ManPGriffithsPGChinneryPFMitochondrial optic neuropathies – disease mechanisms and therapeutic strategiesProg Retin Eye Res2011308111421112411
- Yu-Wai-ManPVotrubaMMooreATChinneryPFTreatment strategies for inherited optic neuropathies: past, present and futureEye20142852153724603424
- MashimaYKimuraIYamamotoYOptic disc excavation in the atrophic stage of Leber’s hereditary optic neuropathy: comparison with normal tension glaucomaGraefes Arch Clin Exp Ophthalmol2003241758012605258
- BarboniPCarbonelliMSaviniGNatural history of Leber’s hereditary optic neuropathy: longitudinal analysis of the retinal nerve fiber layer by optical coherence tomographyOphthalmology201011762362720031228
- BarboniPSaviniGValentinoMLRetinal nerve fiber layer evaluation by optical coherence tomography in Leber’s hereditary optic neuropathyOphthalmology200511212012615629831
- ZhangYHuangHWeiSCharacterization of macular thickness changes in Leber’s hereditary optic neuropathy by optical coherence tomographyBMC Ophthalmol20141410525179213
- DorfmanLJNikoskelainenERosenthalARSoggRLVisual evoked potentials in Leber’s hereditary optic neuropathyAnn Neurol19771565568883769
- SalomãoSRBerezovskyAAndradeREBelfortRCarelliVSadunAAVisual electrophysiologic findings in patients from an extensive Brazilian family with Leber’s hereditary optic neuropathyDoc Ophthalmol200410814715515455797
- ZiccardiLSadunFDe NegriAMRetinal function and neural conduction along the visual pathways in affected and unaffected carriers with Leber’s hereditary optic neuropathyInvest Ophthalmol Vis Sci2013546893690124071953
- NewmanNJLeber’s hereditary optic neuropathy: new genetic considerationsArch Neurol1993505405488489411
- MashimaYOshitariKImamuraYMomoshimaSShigaHOguchiYOrbital high resolution magnetic resonance imaging with fast spin echo in the acute stage of Leber’s hereditary optic neuropathyJ Neurol Neurosurg Psychiatry1998641241279436742
- KermodeAGMoseleyIFKendallBEMillerDHMacManusDGMcDonaldWIMagnetic resonance imaging in Leber’s optic neuropathyJ Neurol Neurosurg Psychiatry1989526716742732742
- VaphiadesMSPhillipsPHTurbinREOptic nerve and chiasmal enhancement in Leber hereditary optic neuropathyJ Neuroophthalmol20032310410512616096
- SadunFDe NegriAMCarelliVOphthalmologic findings in a large pedigree of 11778/Haplogroup J Leber hereditary optic neuropathyAm J Ophthalmol200413727127714962416
- VenturaDFQuirosPCarelliVChromatic and luminance contrast sensitivities in asymptomatic carriers from a large Brazilian pedigree of 11778 Leber hereditary optic neuropathyInvest Ophthalmol Vis Sci2005464809481416303983
- SaviniGBarboniPValentinoMLRetinal nerve fiber layer evaluation by optical coherence tomography in unaffected carriers with Leber’s hereditary optic neuropathy mutationsOphthalmology200511212713115629832
- GuyJFeuerWJPorciattiVRetinal ganglion cell dysfunction in asymptomatic G11778A: Leber hereditary optic neuropathyInvest Ophthalmol Vis Sci20145584184824398093
- KirkmanMAKorstenALeonhardtMQuality of life in patients with Leber hereditary optic neuropathyInvest Ophthalmol Vis Sci2009503112311519255150
- JohnsDRHeherKLMillerNRSmithKHLeber’s hereditary optic neuropathy: clinical manifestations of the 14484 mutationArch Ophthalmol19931114954988470982
- JohnsDRSmithKHMillerNRLeber’s hereditary optic neuropathy: clinical manifestations of the 3460 mutationArch Ophthalmol1992110157715811444915
- BarboniPSaviniGValentinoMLLeber’s hereditary optic neuropathy with childhood onsetInvest Ophthalmol Vis Sci2006475303530917122117
- Ramos CdoVBellusciCSaviniGAssociation of optic disc size with development and prognosis of Leber’s hereditary optic neuropathyInvest Ophthalmol Vis Sci2009501666167419098324
- DiMauroSSchonEMitochondrial respiratory-chain diseasesN Engl J Med20033482656266812826641
- SchapiraAHMitochondrial diseasesLancet20123791825183422482939
- McFarlandRTurnbullDMBatteries not included: diagnosis and management of mitochondrial diseaseJ Intern Med200926521022819192037
- ZevianiMDi DonatoSMitochondrial disordersBrain2004127Pt 102153217215358637
- KoeneSSmeitinkJMitochondrial medicine: entering the era of treatmentJ Intern Med200926519320919192036
- WallaceDMitochondrial diseases in man and mouseScience19992831482148810066162
- SprouleDMKaufmannPMitochondrial encephalopathy, lactic acidosis, and strokelike episodes: basic concepts, clinical phenotype, and therapeutic management of MELAS syndromeAnn N Y Acad Sci2008114213315818990125
- MargulisLGenetic and evolutionary consequences of symbiosisExp Parasitol197639277349816668
- FraserJABiousseVNewmanNJThe neuro-ophthalmology of mitochondrial diseaseSurv Ophthalmol20105529933420471050
- SutovskyPMorenoRDRamalho-SantosJDominkoTSimerlyCSchattenGUbiquitin tag for sperm mitochondriaNature2005200519981999
- JenuthJPetersonAShoubridgeETissue-specific selection for different mtDNA genotypes in heteroplasmic miceNat Genet19971693959140402
- ChinneryPFDiMauroSShanskeSRisk of developing a mitochondrial DNA deletion disorderLancet200436459259615313359
- MacmillanCKirkhamTFuKPedigree analysis of French Canadian families with T14484C Leber’s hereditary optic neuropathyNeurology1998504174229484365
- ValentinoMLBarboniPGhelliAThe ND1 gene of complex I is a mutational hot spot for Leber’s hereditary optic neuropathyAnn Neurol20045663164115505787
- ChinneryPFBrownDTAndrewsRMThe mitochondrial ND6 gene is a hot spot for mutations that cause Leber’s hereditary optic neuropathyBrain200112420921811133798
- ChinneryPAndrewsRTurnbullDHowellNLeber hereditary optic neuropathy: does heteroplasmy influence the inheritance and expression of the G11778A mitochondrial DNA mutation?Am J Med Genet20019823524311169561
- Gómez-DuránAPacheu-GrauDLópez-GallardoEUnmasking the causes of multifactorial disorders: OXPHOS differences between mitochondrial haplogroupsHum Mol Genet2010193343335320566709
- Gómez-DuránAPacheu-GrauDMartínez-RomeroIOxidative phosphorylation differences between mitochondrial DNA haplogroups modify the risk of Leber’s hereditary optic neuropathyBiochim Biophys Acta201218221216122222561905
- HudsonGCarelliVSpruijtLClinical expression of Leber hereditary optic neuropathy is affected by the mitochondrial DNA-haplogroup backgroundAm J Hum Genet20078122823317668373
- JiYZhangA-MJiaXMitochondrial DNA haplogroups M7b1’2 and M8a affect clinical expression of Leber hereditary optic neuropathy in Chinese families with the m.11778G – A mutationAm J Hum Genet20088376076819026397
- GiordanoCIommariniLGiordanoLEfficient mitochondrial biogenesis drives incomplete penetrance in Leber’s hereditary optic neuropathyBrain2014137Pt 233535324369379
- BuXRotterJX chromosome-linked and mitochondrial gene control of Leber hereditary optic neuropathy: evidence from segregation analysis for dependence on X chromosomeProc Natl Acad Sci U S A199188819882021896469
- HudsonGKeersSManPIdentification of an X-chromosomal locus and haplotype modulating the phenotype of a mitochondrial DNA disorderAm J Hum Genet2005771086109116380918
- ShankarSPFingertJHCarelliVEvidence for a novel x-linked modifier locus for Leber hereditary optic neuropathyOphthalmic Genet200829172418363168
- JiYJiaXLiSXiaoXGuoXZhangQEvaluation of the X-linked modifier loci for Leber hereditary optic neuropathy with the G11778A mutation in ChineseMol Vis2010809041642420300564
- GiordanoCMontopoliMPerliEOestrogens ameliorate mitochondrial dysfunction in Leber’s hereditary optic neuropathyBrain2011134Pt 122023420943885
- KirkmanMAYu-Wai-ManPKorstenAGene-environment interactions in Leber hereditary optic neuropathyBrain2009132Pt 92317232619525327
- PottJWWongKHLeber’s hereditary optic neuropathy and vitamin B12 deficiencyGraefes Arch Clin Exp Ophthalmol20062441357135916523300
- SadunAWinPRoss-CisnerosFWalkerSCarelliVLeber’s hereditary optic neuropathy differentially affects smaller axons in the optic nerveTrans Am Ophthalmol Soc20009822323511190025
- AndrewsRMGriffithsPGJohnsonMATurnbullDMHistochemical localisation of mitochondrial enzyme activity in human optic nerve and retinaBr J Ophthalmol19998323123510396204
- BristowEGriffithsPAndrewsRJohnsonMTurnbullDThe distribution of mitochondrial activity in relation to optic nerve structureArch Ophthalmol200212079179612049585
- Yu Wai ManCYChinneryPFGriffithsPGOptic neuropathies – importance of spatial distribution of mitochondria as well as functionMed Hypotheses2005651038104216098682
- CarelliVRugoloMSgarbiGBioenergetics shapes cellular death pathways in Leber’s hereditary optic neuropathy: a model of mitochondrial neurodegenerationBiochim Biophys Acta2004165817217915282189
- LinCSSharpleyMSFanWMouse mtDNA mutant model of Leber hereditary optic neuropathyProc Natl Acad Sci U S A2012109200652007023129651
- CarelliVLa MorgiaCValentinoMLBarboniPRoss-CisnerosFNSadunAARetinal ganglion cell neurodegeneration in mitochondrial inherited disordersBiochim Biophys Acta2009178751852819268652
- GropmanAChenT-JPerngC-LVariable clinical manifestation of homoplasmic G14459A mitochondrial DNA mutationAm J Med Genet2004124A37738214735585
- HowellNKubackaIMcCulloughDLeber hereditary optic neuropathy: involvement of the mitochondrial ND1 gene and evidence for an intragenic suppressor mutationAm J Hum Genet1991489359422018041
- HardingASweeneyMMillerDOccurrence of a multiple sclerosis-like illness in women who have a Leber’s hereditary optic neuropathy mitochondrial DNA mutationBrain1992115Pt 49799891393514
- PfefferGBurkeAYu-Wai-ManPCompstonDAChinneryPFClinical features of MS associated with Leber hereditary optic neuropathy mtDNA mutationsNeurology2013812073208124198293
- PalaceJMultiple sclerosis associated with Leber’s hereditary optic neuropathyJ Neurol Sci2009286242719800080
- StelmackJTangXRedaDRineSMancilRMassofROutcomes of the veterans affairs low vision intervention trial (LOVIT)Arch Ophthalmol200812660861718474769
- NewmanNJTreatment of hereditary optic neuropathiesNat Rev Neurol2012854555622945544
- PfefferGMajamaaKTurnbullDThorburnDChinneryPTreatment for mitochondrial disordersCochrane Database Syst Rev20124004426
- PfefferGHorvathRKlopstockTNew treatments for mitochondrial disease – no time to drop our standardsNat Rev Neurol2013947448123817350
- SaylorMMcLoonLKHarrisonARLeeMSExperimental and clinical evidence for brimonidine as an optic nerve and retinal neuroprotective agentArch Ophthalmol200912740240619365015
- NewmanNJBiousseVDavidRProphylaxis for second eye involvement in Leber hereditary optic neuropathy: an open-labeled, nonrandomized multicenter trial of topical brimonidine puriteAm J Ophthalmol200514040741516083844
- ThouinAGriffithsPGHudsonGChinneryPFYu-Wai-ManPRaised intraocular pressure as a potential risk factor for visual loss in Leber hereditary optic neuropathyPloS One2013863446
- GiorgioVPetronilliVGhelliAThe effects of idebenone on mitochondrial bioenergeticsBiochim Biophys Acta2012181736336922086148
- MordenteAMartoranaGMinottiGGiardinaBAntioxidant properties of 2,3-dimethoxy-5-methyl-6-(10-hydroxydecyl)-1, 4-benzoquinone (idebenone)Chem Res Toxicol199854639477226
- MashimaYHiidaYOguchiYRemission of Leber’s hereditary optic neuropathy with idebenoneLancet19923403683691353825
- KlopstockTYu-Wai-ManPDimitriadisKA randomized placebo-controlled trial of idebenone in Leber’s hereditary optic neuropathyBrain2011134Pt 92677268621788663
- KlopstockTMetzGYu-Wai-ManPPersistence of the treatment effect of idebenone in Leber’s hereditary optic neuropathyBrain2013136Pt 2e23023388409
- CarelliVLa MorgiaCValentinoMLIdebenone treatment in Leber’s hereditary optic neuropathyBrain2011134Pt 9e18821810891
- RudolphGDimitriadisKBüchnerBEffects of idebenone on color vision in patients with Leber hereditary optic neuropathyJ Neuroophthalmol201333303623263355
- SadunAChicaniCRoss-CiscernosFEffect of EPI-743 on the clinical course of the mitochondrial disease Leber hereditary optic neuropathyArch Neurol20126933133822410442
- WenzTWilliamsSLBacmanSRMoraesCTEmerging therapeutic approaches to mitochondrial diseasesDev Disabil Res Rev20101621922920818736
- La MorgiaCCarbonelliMBarboniPSadunAACarelliVMedical management of hereditary optic neuropathiesFront Neurol2014514125132831
- WenzTDiazFSpiegelmanBMMoraesCTActivation of the PPAR/PGC-1alpha pathway prevents a bioenergetic deficit and effectively improves a mitochondrial myopathy phenotypeCell Metab2008824925618762025
- GuyJNew therapies for optic neuropathies: development in experimental modelsCurr Opin Ophthalmol20001142142911141636
- DiMauroSMancusoMMitochondrial diseases: therapeutic approachesBiosci Rep20072712513717486439
- ManfrediGFuJOjaimiJRescue of a deficiency in ATP synthesis by transfer of MTATP6, a mitochondrial DNA-encoded gene, to the nucleusNat Genet20023039439911925565
- GuyJQiXPallottiFRescue of a mitochondrial deficiency causing Leber hereditary optic neuropathyAnn Neurol20025253454212402249
- EllouzeSAugustinSBouaitaAOptimized allotopic expression of the human mitochondrial ND4 prevents blindness in a rat model of mitochondrial dysfunctionAm J Hum Genet20088337338718771762
- GuyJQiXKoilkondaRDEfficiency and safety of AAV-mediated gene delivery of the human ND4 complex I subunit in the mouse visual systemInvest Ophthalmol Vis Sci2009504205421419387075
- Cwerman-ThibaultHAugustinSEllouzeSSahelJ-ACorral- DebrinskiMGene therapy for mitochondrial diseases: Leber hereditary optic neuropathy as the first candidate for a clinical trialC R Biol201433719320624702846
- Safety Study of an Adeno-associated Virus Vector for Gene Therapy of Leber’s Hereditary Optic Neuropathy (LHON) Caused by the G11778A Mutation2015 Available from: https://clinicaltrials.gov/ct2/show/NCT02161380Accessed February 21, 2015
- Safety and Efficacy Study of rAAV2-ND4 Treatment of Leber Hereditary Optic Neuropathy (LHON)2015 Available from: https://clinical-trials.gov/ct2/show/NCT01267422Accessed February 21, 2015
- Safety Evaluation of Gene Therapy in Leber Hereditary Optic Neuropathy (LHON) Patients2015 Available from: https://clinicaltrials.gov/ct2/show/NCT02064569Accessed February 21, 2015
- FloreaniMNapoliEMartinuzziAAntioxidant defences in cybrids harboring mtDNA mutations associated with Leber’s hereditary optic neuropathyFEBS J20052721124113515720387
- QiXSunLHauswirthWWLewinASGuyJUse of mitochondrial antioxidant defenses for rescue of cells with a Leber hereditary optic neuropathy-causing mutationArch Ophthalmol200712526827217296905
- IyerSBergquistKYoungKGnaigerERaoRRBennettJPMitochondrial gene therapy improves respiration, biogenesis, and transcription in G11778A Leber’s hereditary optic neuropathy and T8993G Leigh’s syndrome cellsHum Gene Ther20122364765722390282
- YuHKoilkondaRChouTGene delivery to mitochondria by targeting modified adenoassociated virus suppresses Leber’s hereditary optic neuropathy in a mouse modelProc Natl Acad Sci U S A201210912381247
- YuHMehtaAWangGNext-generation sequencing of mitochondrial targeted AAV transfer of human ND4 in miceMol Vis2013191482149123869167
- MarchettiVKrohneTFriedlanderDFriedlanderMStemming vision loss with stem cellsJ Clin Investig20101203012302120811157
- Dahlmann-NoorAVijaySJayaramHLimbAKhawPTCurrent approaches and future prospects for stem cell rescue and regeneration of the retina and optic nerveCan J Ophthalmol20104533334120648090
- JohnsonTVBullNDHuntDPMarinaNTomarevSIMartinKRNeuroprotective effects of intravitreal mesenchymal stem cell transplantation in experimental glaucomaInvest Ophthalmol Vis Sci2010512051205919933193
- ConnickPKolappanMCrawleyCAutologous mesenchymal stem cells for the treatment of secondary progressive multiple sclerosis: an open-label phase 2a proof-of-concept studyLancet Neurol20121115015622236384
