Abstract
Purpose
To evaluate the effects of the different fragmentation patterns for the lens nucleus in terms of the effective phacoemulsification time (EPT) and power.
Setting
Shinagawa LASIK Center, Tokyo, Japan.
Design
Comparison study.
Methods
Seventy-one eyes of 71 patients had preoperative lens opacity grading based on the Emery-Little Classification (Grade 1 and Grade 2). Eyes underwent femtosecond laser-assisted cataract surgery (Catalys™ Precision Laser System), for capsulotomy and lens fragmentation. For the lens fragmentation, either the quadrants softened (Quadrant) or the quadrants complete (Complete) pattern was used. The mean EPT and phacoemulsification (phaco) power for each cutting pattern of Grades 1 and 2 cataracts were evaluated.
Results
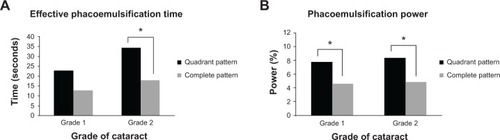
The mean EPT was 28.96 seconds in the Quadrant Group and 16.31 seconds in the Complete Group (P=0.006). The mean phaco power was 8.07% in the Quadrant Group and 4.77% in the Complete Group (P=0.0002). Comparing the Quadrant and Complete Groups of Grade 1 cataract showed no significant difference in EPT (P=0.16), but showed a significant difference in phaco power (P=0.033). Comparing the Quadrant and Complete patterns of Grade 2 cataract showed significant differences in both EPT (P=0.012) and phaco power (P=0.003). Using the Complete pattern showed a 44.7% reduction in EPT and a 40.9% reduction in phaco power when compared to the Quadrant Group.
Conclusion
Using the smaller fragmentation pattern in femtosecond laser cataract surgery, the phaco time and power were reduced significantly when compared to the procedure with the larger fragmentation pattern.
Introduction
Laser has been used in cataract surgery since the 1970s. In 1975, KrasnovCitation1 reported on the use of phacopuncture with a Q-switched ruby laser (694 nm) to create micro-perforations on the anterior capsule, allowing a gradual release and absorption of the lens material over time. The femtosecond laser has been used clinically in a variety of anterior segment applications. These include the creation of a corneal flap for laser in situ keratomileusis refractive surgery, arcuate incisions for modifying corneal astigmatism, and penetrating keratoplasty for corneal transplantation.
In the past 4 years, femtosecond lasers have been used in cataract surgery for capsulotomy creation, lens fragmentation, and corneal incision. This appears to be a rapidly evolving technology which attracts worldwide attention because cataract procedures are the most frequently performed surgery in ophthalmology.Citation2 The femtosecond laser guarantees the stability, precision, length, shape, and width of the corneal incisions.Citation3 Another unique advantage is the possibility of imaging the cutting process, which can easily be done before, during, and after surgery. This is because the laser process is a three-dimensional (3-D) scanning process and the essential 3-D beam delivery for acquiring a 3-D image is already part of the system. Thus, the target tissue can be scanned easily without making room for additional scanning mirrors and lenses for imaging using optical coherence tomography (OCT) imaging or other imaging technologies.Citation4 Cataract surgeons are adopting femtosecond technology to perform laser capsulotomy, lens fragmentation, clear cornea incisions, and limbal relaxing incisions.Citation5 Precise central continuous circular capsulotomy is a prerequisite for good postoperative effective lens position. Irregular capsulotomies might cause refractive surprises such as myopic or hyperopic shifts, unwanted surgically-induced astigmatism (SIA), posterior chamber lens tilt, increase in higher order aberrations, and glare and halo phenomena as well.Citation2 Additionally, femtosecond lasers are currently used to address some of the remaining issues associated with manual cataract surgery by improving precision and reducing risks.Citation6–Citation8
This study evaluates the difference of two laser fragmentation patterns in terms of the duration, or effective phacoemulsification time (EPT), and phacoemulsification (phaco) power for the different grades of cataract. The purpose was to estimate the effect of the different fragmentation patterns in terms of the EPT and power, in order to make the surgery more safe and effective.
Patients and methods
Seventy-one eyes of 71 patients were included in the study. All patients provided written informed consent in accordance with the Declaration of Helsinki. Institutional review board (Matsumoto Clinic, Tokyo, Japan) approval was obtained for this study. The mean age of all patients was 60±6.66 years (range: 45 to 75 years) for 27 males and 44 females. All enrolled subjects underwent standard preoperative examinations. Two groups were created based on the femtosecond laser-assisted lens fragmentation pattern (): Group I, with Quadrant fragmentation pattern and Group II, with Complete fragmentation pattern. Each group was divided into subgroups according to the Emery-Little Classification System of nuclear opacity grade. Since all the patients’ cataracts were either grade 1 or grade 2, each group included only two subgroups (Grade 1 and Grade 2). All laser surgery was performed using the Catalys® Precision Laser System (OptiMedica, Sunnyvale, CA, USA), which has been described in detail.Citation6 presents the demographics of the patients in the study.
Figure 1 Fragmentation pattern during cataract surgery (A) Complete pattern and (B) Quadrant pattern.
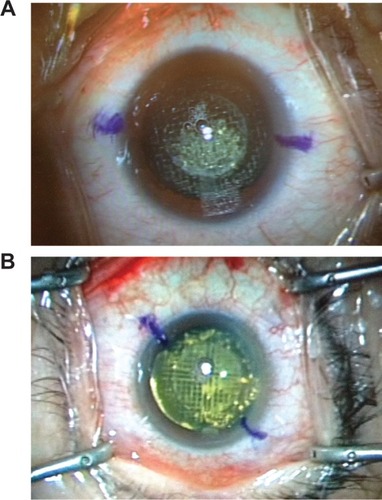
Table 1 Patients demographic
Surgical technique
The surgery had a double set-up procedure – the first part included the femtosecond laser surgery and the second part subjected the patient for phaco. Laser capsulotomy and lens fragmentation were carried out by the CATALYS (Catalys™ Precision Laser System; OptiMedica, Sunnyvale, CA, USA) machine. Femtosecond laser-assisted cataract surgery was performed in one eye of each patient. After pupil dilation (phenylephrine 2.5% and tropicamide 0.5%) and corneal anesthesia (Oxybuprocaine hydrochloride, Conjucain EDO 0.4%; Bausch & Lomb Incorporated, Rochester, NY, USA), the patient was placed in a supine position in the operating chair. No eye speculum was used. After the patient was docked to the system, the OCT imaged the anterior chamber and the system created a 3-D treatment plan. In all cases, the laser created a 5.0 mm diameter curvilinear capsulotomy (4 mJ pulse energy). The lens was segmented into quadrants and softened with a grid spacing of 350 mm (9 mJ pulse energy), and segmentation-softening spacing was 300 mm. After the laser procedure was completed, the patient was transferred to the operating table and phaco procedure proceeded.
The manual surgical cataract procedure was performed directly after laser treatment and measurements. A modified divide and conquer technique was done using the (Infiniti® Ozil® Alcon Laboratories, Inc., Fort Worth, TX, USA), with the phaco settings seen in .
Table 2 Phacoemulsification settings (surgeon’s nomogram)
The softened nucleus was aspirated. Residual cortex removal and posterior capsule polishing were performed through the nasal and temporal incisions using bimanual irrigation/aspiration. After cortical removal, a multifocal (Acriva Reviol; VSY Biotechnology, Amsterdam, the Netherlands; or RESTOR®; Alcon Laboratories, Inc.) or a monofocal (Acrysof®; Alcon Laboratories, Inc.) intraocular lens (IOL), depending on the patient’s IOL preference, was placed in the posterior chamber.
Postoperative protocol
In all cases, the following post-operative medications were given as follows: oral levofloxacin 500 mg tablet once a day for 3 days; topical diclofenac sodium 0.1%, dexa methasone sodium m-sulfobenzoate 0.1%, and moxifloxacin hydrochloride 0.5% five times a day for 1 week. After 1 week, diclofenac was reduced to four times a day for 1 month, while the latter two were then replaced with topical fluorometholone 0.1% and ofloxacin 0.3%, prescribed as four times a day, up to 1 month, then discontinued.
Postoperative examinations were performed at 1 day, 1 week, 1 month, and 3 months and included visual acuity and biomicroscopy.
Statistical analysis
The EPT and phaco power were recorded for all cases. The results were expressed as mean ± standard deviation (SD). The normality of the data was tested by the Shapiro–Wilk test and was performed using JMP statistical software (version 9, SAS Institute Inc., Cary, NC, USA). Unpaired t-test was used to compare the difference between normally-distributed groups; in those cases with data that were not normally-distributed, the Mann–Whitney U test was performed. The level for statistical significance was set at P<0.05.
Results
We evaluated the groups based on the femtosecond laser-assisted lens fragmentation pattern () in terms of EPT and power. The mean EPT was 28.96 seconds in the Quadrant Group and 16.31 seconds in the Complete Group. The mean phaco power was 8.07% in the Quadrant Group and 4.77% in the Complete Group. Using the complete pattern, there was a 44.7% reduction in EPT and a 40.9% reduction in phaco power when compared to the Quadrant Group. The mean values of the EPT and phaco power for each subgroup of the two groups are shown in . There was no significant difference in the EPT between the Complete and Quadrant Groups for Grade 1 cataract subgroup (P=0.16), but there was a significant difference in the phaco power (P=0.03). Comparing the Grade 2 subgroup of both groups with the different patterns showed significant differences in the EPT (P=0.01) and phaco power (P=0.003). Additionally, we performed a statistical analysis of the differences in uncorrected distance visual acuity (UDVA), corrected distance visual acuity (CDVA), spherical equivalent (SE), and endothelial cell density between the Quadrant and Complete Groups. No significant differences were found.
Discussion
Femtosecond lasers are being used to address some of the remaining issues associated with manual cataract surgery. Excess energy that occurs with phaco may cause capsule complications as well as damage to the corneal epithelium at the probe insertion site; thus it is beneficial to try to limit the ultrasound (US) energy exposure.Citation6,Citation9 It was found that the femtosecond laser assistance significantly reduced the EPT and mean phaco energy.Citation10–Citation12
Initial results by Palanker et alCitation13 indicate an approximate 40% reduction in US energy used during phaco (cumulative dissipated energy) compared with manual cataract surgery. Abell et alCitation10 report a 70% reduction in mean EPT compared with the manual technique. Studies of femtosecond laser lens fragmentation by Conrad-Hengerer et alCitation11 found a significant reduction (>96%) in EPT using the femtosecond laser technique compared with the manual technique. With the growing experience of the femtosecond laser technique and the optimal use of the different fragmentation patterns for different cataract grades, we anticipate reducing the EPT using this laser system.
We evaluated the different laser fragmentation patterns used in laser cataract surgeries in terms of EPT and power. The primary endpoint was EPT. Reduced phaco time reduces the total number of joules of energy delivered to the eye and may lead to better preservation of ocular structures. Less energy delivered to the eye may be associated with earlier improvement of postoperative visual acuity due to less endothelial cell loss and corneal edema, with less anterior chamber cells and flare caused by the alteration of the blood–aqueous barrier. Phaco time has been shown to be directly correlated with endothelial cell loss.Citation14 Several studies have used phaco time or energy (power × time) to compare aspects of phaco procedures.Citation15–Citation20 Many kinds of surgical trauma during phaco have been reported to injure corneal endothelial cells,Citation14,Citation21–Citation23 demonstrating that US energy and irrigation directly injure the endothelium.Citation14,Citation21,Citation22 In this study, we paid particular attention to the role of nucleus firmness, laser fragmentation patterns, and US energy in endothelial cell loss. The firmness of the nucleus was the most significant risk factor for endothelial injury. The size of the nucleus was also significantly associated with the risk. That is to say, the harder and larger the nucleus, the greater the degree of endothelial injury. Although the total US energy was proportional to the grade of the nucleus, US energy was not an independent predictor. Therefore, the nucleus itself was considered to injure the endothelial cells. Our results showed no significant difference in endothelial cell density loss (P=0.77) between the two groups with different laser fragmentation patterns. In addition, phaco time and average phaco power are known to have a positive correlation with the nuclear opalescence.Citation24 It was published that reductions in power and time may be seen when laser phacofragmentation is performed in conjunction with phaco.Citation7
Furthermore, we created subgroups based on the hardness of the cataract. There was a significant difference in phaco power and EPT between the two patterns with grade 2 cataracts. Based on the mean value, we may consider that the quadrant pattern fragmentation for grade 2 cataracts expends more phaco power with a high EPT. For grade 1 cataracts, the difference between the two patterns lies only in the phaco power, but not in EPT.
In summary, we may conclude that in cataract surgeries, using the smaller fragmentation pattern (Complete) of the femtosecond laser is more beneficial with significantly reduced phaco time and power when compared with the larger fragmentation pattern (Quadrant). However, further studies are needed to compare the advantages and disadvantages of each fragmentation pattern in relation to the size of the phaco tip, lumen, and the system used.
Disclosure
The authors report no conflicts of interest in this work.
References
- KrasnovMMLaser-phacopuncture in the treatment of soft cataractsBr J Ophthalmol197559296981131350
- NagyZZFemtolaser cataract surgery: how to evaluate this technology, read the literature, and avoid possible complicationsJ Refract Surg2012281285585723231735
- SugarAUltrafast (femtosecond) laser refractive surgeryCurr Opin Ophthalmol200213424624912165709
- GibsonEAMasihzadehOLeiTCAmmarDAKahookMYMultiphoton microscopy for ophthalmic imagingJ Ophthalmol2011201187087921274261
- UyHSEdwardsKCurtisNFemtosecond phacoemulsification: the business and the medicineCurr Opin Ophthalmol2012231333922081031
- HeLSheehyKCulbertsonWFemtosecond laser-assisted cataract surgeryCurr Opin Ophthalmol2011221435221150606
- NagyZTakacsAFilkornTSaraybaMInitial clinical evaluation of an intraocular femtosecond laser in cataract surgeryJ Refract Surg200925121053106020000286
- Naranjo-TackmanRHow a femtosecond laser increases safety and precision in cataract surgery?Curr Opin Ophthalmol2011221535721150605
- ErnestPRhemMMcDermottMLaveryKSensoliAPhacoemulsification conditions resulting in thermal wound injuryJ Cataract Refract Surg200127111829183911709258
- AbellRGKerrNMVoteBJFemtosecond laser-assisted cataract surgery compared with conventional cataract surgeryClin Experiment Ophthalmol201341545546223078347
- Conrad-HengererIHengererFHSchultzTDickHBEffect of femtosecond laser fragmentation on effective phacoemulsification time in cataract surgeryJ Refract Surg2012281287988323231739
- Conrad-HengererIHengererFHSchultzTDickHBEffect of femtosecond laser fragmentation of the nucleus with different softening grid sizes on effective phaco time in cataract surgeryJ Cataract Refract Surg2012381888189422980639
- PalankerDVBlumenkranzMSAndersenDFemtosecond laser-assisted cataract surgery with integrated optical coherence tomographySci Transl Med201025858ra85
- PolackFMSugarAThe phacoemulsification procedure. II. Corneal endothelial changesInvest Ophthalmol1976156458469931690
- ZetterstromCLaurellCGComparison of endothelial cell loss and phacoemulsification energy during endocapsular phacoemulsification surgeryJ Cataract Refract Surg199521155587722904
- HayashiKNakaoFHayashiFCorneal endothelial cell loss after phacoemulsification using nuclear cracking proceduresJ Cataract Refract Surg199420144478133479
- BrintSFBlaydesJEBloombergLInitial experience with the HydroSonics instrument to soften cataracts before phacoemulsificationJ Cataract Refract Surg19921821301351564649
- LaveryKTMcDermottMLErnestPHEndothelial cell loss after 4 mm cataract surgeryJ Cataract Refract Surg19952133053087674168
- KlemenUMV-style phacoemulsificationJ Cataract Refract Surg19931945485508355166
- PirazzoliGD’EliseoDZiosiMAcciarriREffects of phacoemulsification time on the corneal endothelium using phacofracture and phaco chop techniquesJ Cataract Refract Surg19962279679699041091
- DickHBKohnenTJacobiFKJacobiKWLong-term endothelial cell loss following phacoemulsification through a temporal clear corneal incisionJ Cataract Refract Surg199622163718656366
- OlsonLEMarshallJRiceNSAndrewsREffects of ultrasound on the corneal endothelium: I. The acute lesionBr J Ophthalmol1978623134144638104
- EdelhauserHFVan HornDLHyndiukRASchultzROIntraocular irrigating solutions. Their effect on the corneal endotheliumArch Ophthalmol1975938648657239670
- BencicGZoric-GeberMSaricDCorakMMandicZClinical importance of the Lens Opacities Classification System III (LOCS III) in phacoemulsificationColl Antropol200529Suppl 1919416193685