Abstract
Trapdoor fractures, or blowout fractures, result from muscle entrapment after orbital floor fractures. The incarcerated muscles may become necrotic because of ischemia; immediate surgery is recommended for symptomatic persistent diplopia or clinical evidence of entrapment. We report a case of spontaneous resolution of diplopia in a patient with a high suspicion of a trapdoor fracture. A 15-year-old girl presented with diplopia after being hit in the eye while playing volleyball. Computed tomography did not show a fractured orbital bone, but the forced duction test was positive when the left eye was pulled forward toward the left. Magnetic resonance imaging was negative for edema and inflammation in the extraocular muscles. With observation only, the diplopia resolved 2 weeks after onset. A negative forced duction test confirmed the resolution. Observation only may be appropriate in cases with posttraumatic limited ocular movement, after imaging has excluded an emergent condition.
Background
Orbital floor fractures, also known as blowout fractures, are fractures in which the orbital bone is isolated from the orbital floor but with an intact orbital rim.Citation1 These fractures often occur during engagement in sports or play, motor vehicle accidents, or assaults.Citation2–Citation4 The trapdoor fracture, also called a “white-eyed blowout” is a blowout fracture in which a linear orbital wall fracture occurs.Citation2 A flap of bone then is displaced outwardly, and it immediately returns to its original position.Citation3 This is caused by muscle entrapment or connective tissue septa after the orbital floor fracture,Citation4,Citation5 and without emergent release, the incarcerated muscles may become necrotic because of ischemia.Citation6–Citation8 In the chronic phase, fibrosis may also develop from inflammation, causing permanent ocular movement disorders.Citation4,Citation5,Citation8,Citation9 For this reason, immediate surgery is often recommended for orbital floor fractures with symptomatic persistent diplopia or clinical evidence of entrapment.Citation7,Citation8,Citation10 We report a case of spontaneous resolution of diplopia in a patient with a high suspicion of trapdoor fracture.
Case presentation
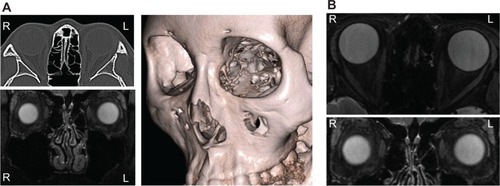
A 15-year-old girl sustained a mild blow to her left eye while playing volleyball and later noticed diplopia with mild pain at the inner canthus, with no nausea or vomiting. She presented to our clinic the day of the injury with esotropia. The Hess chart examination showed an abducent disorder of her left eye (). Both pupils were round and of equal size. The best-corrected visual acuity (BCVA) was 1.2 bilaterally; other ophthalmic examinations showed no abnormalities except for limited ocular movement of the left eye. Since a posttraumatic abducent disorder was observed in the left eye, the Radiodiagnostics Department in our hospital imaged the eye for an orbital floor fracture. However, the thin slice (1 mm) computed tomography (CT) scans were negative, and maxillary sinuses were intact with no fluid or fractures (). To identify paralysis or functional damage, we consulted specialist strabismologists in our department. The forced duction test was performed by them and was unexpectedly positive when the left eye was pulled forward to the left side, indicating the presence of incarceration, with an inapparent orbital bone fracture and suspected trapdoor fracture. Magnetic resonance imaging (MRI), including short tau inversion recovery (STIR) imaging, a modality for fat suppression and enhancement of edema and inflammation in bodily tissues,Citation11 was performed to confirm edema and inflammation in the extraocular muscles. The scan was negative for edema and inflammation and other abnormalities (). The Otolaryngology – Head and Neck Surgery Department in our hospital recommended observation without surgery because the visual acuity (VA) was good and imaging showed no fracture, muscle entrapment, edema, or active inflammation. The symptoms remained the same until 2 weeks later, when the patient reported sudden resolution of the diplopia. A Hess chart examination and a forced duction test were normal that day (). Two months later, there were no sequelae, including diplopia.
Figure 1 The Hess chart examination at the initial visit.
Abbreviations: Sup., superior; Inf., inferior; Lat., lateral; Med., medial; Rect., rectus muscle; Obl., oblique muscle.
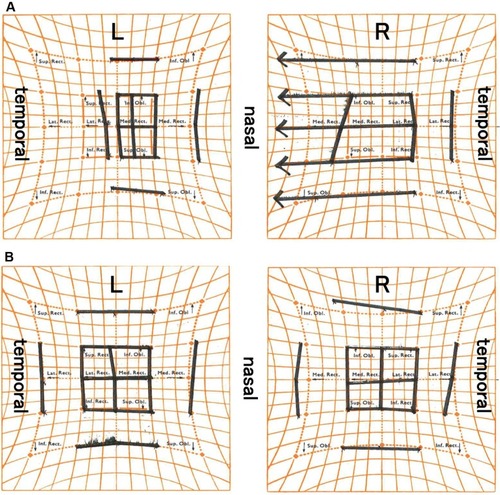
Figure 2 The orbital imaging with CT and MRI at initial visit.
Discussion
No apparent objective evidence of orbital fracture was found in this case, although we used a CT with a thin slice (1 mm). In addition, suspicious symptoms of blowout or entrapment of extraocular muscles, such as the oculocardiac reflex (nausea, vomiting, bradycardia, and syncope) were absent. We also considered psychogenic esotropia in the differential diagnosis, which is concomitant squint without any organic state and caused by a psychogenetic etiology.Citation11 However, the patient had limited abduction of her left eye and a positive forced duction test when the left eye was pulled to the left. The patient also reported discomfort of the left inner canthus when the left eye was pulled toward the left, which indicated an organic state but no psychogenic etiology. A CT generally provides excellent bone images and is highly sensitive for imaging orbital floor fractures but is imperfect (sensitivity, 96%; specificity, 71%).Citation12 We suspected that the limited movement of the left eye was caused by a trapdoor fracture, despite the absence of an apparent fracture on the CT, ie, when the left eye was hit by the volleyball, the medial orbital wall would likely have sustained a microfracture. Subsequently, orbital tissue might be entrapped in this space.
The indications for immediate surgery for orbital floor fractures are commonly symptomatic persistent diplopia, muscle or soft tissue entrapment on the CT, and positive forced ductions or other clinical evidence of entrapment, enophthalmos (>2 mm at presentation), oculocardiac reflex, fractures comprising greater than 50% of the orbital floor, or no clinical improvement over several weeks.Citation8–Citation10 Most studies have reported that earlier surgical intervention for children with entrapment results in better outcomes than does later intervention,Citation7–Citation9,Citation13–Citation18 whereas Criden and EllisCitation19 reported that recovery of extraocular motility was prolonged in children compared with adults, despite early surgical intervention. In addition, numerous possible complications are associated with surgery for orbital floor fractures in children, such as infection, hemorrhage, motility problems (restriction and persistent diplopia), implant-related complications (migration/extrusion, palpable hardware, autologous graft donor site pain), muscle or optic nerve incarceration or compression, fistula, cyst and mucocele formation, cosmesis, infraorbital dysesthesia, and lacrimal system problems (dacrocystitis, obstruction).Citation9,Citation13,Citation16,Citation17,Citation19 In the current case, following an athletic injury, there was no sign of an orbital fracture on the CT, but the patient had diplopia and positive forced duction. Ordinarily, this patient might have been a surgical candidate. However, we chose observation because results showed normal ophthalmic findings, with no ocular motility problems other than diplopia, and she was asymptomatic. In addition, STIR-MRI did not detect any abnormality that might lead to irreversible fibrosis in the extraocular muscles. In fact, the situation resolved completely without any complications, including diplopia.
In conclusion, we had an unusual experience with an orbital trapdoor fracture. Physicians may choose to observe patients without surgery in cases of posttraumatic limited ocular movement, after CT and STIR-MRI have excluded conditions that require emergent care.
Disclosure
The authors report no conflicts of interest in this work.
References
- SmithBReganWFBlow-out fracture of the orbit; mechanism and correction of internal orbital fractureAm J Ophthalmol195744673373913487709
- EthunandanMEvansBTLinear trapdoor or “white-eye” blowout fracture of the orbit: not restricted to childrenBr J Oral Maxillofac Surg201149214214720466466
- PhanLTJordan PiluekWMcCulleyTJOrbital trapdoor fracturesSaudi J Ophthalmol201226327728223961006
- KoornneefLZonneveldFWOrbital anatomy, the direct scanning of the orbit in three planes and their bearings on the treatment of motility disturbances of the eye after orbital “blow-out” fracturesActa Morphol Neerl Scand19852332292464096270
- KoornneefLCurrent concepts on the management of orbital blow-out fracturesAnn Plast Surg1982931852007137815
- BaekSHLeeEYClinical analysis of internal orbital fractures in childrenKorean J Ophthalmol2003171444912882507
- SiresBSStanleyRBLevineLMOculocardiac reflex caused by orbital floor trapdoor fracture: an indication for urgent repairArch Ophthalmol199811679559569682717
- JordanDRAllenLHWhiteJHarveyJPashbyREsmaeliBIntervention within days for some orbital floor fractures: the white-eyed blowoutOphthal Plast Reconstr Surg1998146379390
- EgbertJEMayKKerstenRCKulwinDRPediatric orbital floor fracture: direct extraocular muscle involvementOphthalmology2000107101875187911013191
- BurnstineMAClinical recommendations for repair of isolated orbital floor fractures: an evidence-based analysisOphthalmology2002109712071210 discussion 1210–1211; quiz 121212093637
- RappaportEAAnger, apathy and strabismusEye Ear Nose Throat Mon195938647348213653098
- JankSEmshoffREtzelsdorferMStroblHNicasiANorerBUltrasound versus computed tomography in the imaging of orbital floor fracturesJ Oral Maxillofac Surg200462215015414762746
- WangNCMaLWuSYYangFRTsaiYJOrbital blow-out fractures in children: characterization and surgical outcomeChang Gung Med J201033331332020584509
- GerbinoGRocciaFBianchiFAZavatteroESurgical management of orbital trapdoor fracture in a pediatric populationJ Oral Maxillofac Surg20106861310131620381939
- KwonJHMoonJHKwonMSChoJHThe differences of blowout fracture of the inferior orbital wall between children and adultsArch Otolaryngol Head Neck Surg2005131872372716103306
- YoonKCSeoMSParkYGOrbital trapdoor fracture in childrenJ Korean Med Sci200318688188514676448
- GrantJH3rdPatrinelyJRWeissAHKierneyPCGrussJSTrapdoor fracture of the orbit in a pediatric populationPlast Reconstr Surg20021092482489 discussion 490–49511818824
- BansagiZCMeyerDRInternal orbital fractures in the pediatric age group: characterization and managementOphthalmology2000107582983610811070
- CridenMREllisFJLinear nondisplaced orbital fractures with muscle entrapmentJ AAPOS200711214214717416323
- BleyTAWiebenOFrançoisCJBrittainJHReederSBFat and water magnetic resonance imagingJ Magn Reson Imaging201031141820027567
