Abstract
Purpose
Evaluating the clinical results of trans-epithelial collagen cross-linking (CXL) and standard CXL in patients with progressive keratoconus.
Methods
This prospective study comprised 20 eyes of 20 patients with progressive keratoconus. Ten eyes were treated by standard CXL and ten by trans-epithelial cross-linking (TE-CXL, epithelium on) with 1 year of follow-up. All patients underwent complete ophthalmologic testing that included pre- and postoperative uncorrected visual acuity, corrected visual acuity, spherical error, spherical equivalent, corneal astigmatism, simulated maximum, minimum, and average keratometry, coma and spherical aberration, optical pachymetry, and endothelial cell density. Intra-and postoperative complications were recorded. The solution used for standard CXL comprised riboflavin 0.1% and dextran 20.0% (Ricrolin), while the solution for TE-CXL (Ricrolin, TE) comprised riboflavin 0.1%, dextran 15.0%, trometamol (Tris), and ethylenediaminetetraacetic acid. Ultraviolet-A treatment was performed with UV-X System at 3 mW/cm2.
Results
In both the standard CXL group (ten patients, ten eyes; mean age, 30.4±7.3 years) and the TE-CXL group (ten patients, ten eyes; mean age, 28±3.8 years), uncorrected visual acuity and corrected visual acuity improved significantly after treatment. Furthermore, a significant improvement in topographic outcomes, spherical error, and spherical equivalent was observed in both groups at month 12 posttreatment. No significant variations were recorded in other parameters. No complications were noted.
Conclusion
A 1-year follow-up showed stability of clinical and refractive outcomes after standard CXL and TE-CXL.
Introduction
Keratoconus is a degenerative, bilateral, asymmetrical, non-inflammatory disease, which induces biomechanical corneal weakening.Citation1,Citation2 Two different variants of the same surgical technique are adopted for treatment of this disease. Both methods, standard cross-linking (CXL, epi-off CXL) and trans-epithelial cross-linking (epi-on CXL), use ultraviolet-A (UVA) light and riboflavin (photosensitizer, vitamin B2). The photochemical reaction between the latter leads to the development of chemical bonds between collagen fibrils within the corneal stroma thereby strengthening the cornea and slowing or stopping the progression of keratoconus and other corneal ectasia (ie, post-laser in situ keratomileusis and pellucid marginal degeneration).Citation3–Citation7 Epi-off CXL involves epithelium debridement. Long-term clinical studies have shown that this method slows and in most cases blocks keratoconus progressionCitation8–Citation11 and in some cases, it also improves refractive and topographic features.Citation7,Citation12 Epi-on CXL is a technique more recently introduced and is performed without epithelial debridement. This technique aims to reduce postoperative pain and risk of infection, eliminates the need of an operating room, and ensures disease stability.Citation13 In terms of efficacy of both techniques, epi-on CXL and epi-off CXL, opinions seem to be controversial in this regard.Citation14 Literature reports studies that confirm the safety of both techniques.Citation15–Citation18 These works found the procedures to be safe to the endothelium, confirming in vivo the sparing of corneal nerve fibers seen in vitro.Citation19,Citation20 However, further studies showed that the apoptotic effect of epi-on irradiationCitation18,Citation21 was concentrated at a very superficial level, being limited to the anterior stroma and that riboflavin penetration was not homogeneous with the epithelium in situ using the same UVA power, as for standard treatment (3 mW/cm2).Citation21,Citation22
In most previous works, the epi-on technique was performed on patients with central corneal thickness (CCT) greater than 400 μm and homogeneous topographic and anatomical parameters (in a defined range of thickness and keratometry).Citation13,Citation23,Citation24 The aim of our study was to evaluate the efficacy of the two treatments in two homogeneous groups (for age, anatomical and topographic parameters) of patients with progressive keratoconus, in order to better define the validity of both techniques.
Methods
Patients with progressive keratoconus were recruited at the Eye Clinic of the Second University of Naples, Italy, from May 2012 to July 2012. Twenty eyes from 20 affected patients were included in the study. Patients were randomly assigned to one of the two treatment groups (ten eyes were treated with epi-off CXL, and the other ten eyes were treated with epi-on CXL). The study adhered to the tenets of the Declaration of Helsinki and was approved by a departmental Institutional Review Board at the University Hospital Second University of Naples. Moreover, each patient gave written informed consent for his or her involvement. All patients included in the treatment protocol were of age greater than 18 years and presented progressive keratoconus with a documented clinical and instrumental (topographic, pachymetric, or aberrometric) worsening in the previous 6 months of observation. The parameters defined to establish keratoconus progression and inclusion criteria were worsening of uncorrected distance visual acuity (UDVA) and/or corrected distance visual acuity (CDVA) of more than one Snellen line, an increase in central corneal astigmatism of at least 1.00 D, an increase in the maximum cone apex curvature of at least 1.00 D, a reduction of at least 10 μm or more in the thinnest point and the thinnest point being no lower than 400 m, a clear cornea on slit lamp, and the absence of Vogt striae. Exclusion criteria were any coexisting ocular disease or corneal opacities possibly affecting visual acuity, previous intraocular surgery, history of herpetic keratitis, severe dry eye, and concomitant autoimmune diseases.
Clinical pre- and postoperative testing included UDVA, CDVA, slit-lamp exam, spherical error, spherical equivalent (SE), corneal astigmatism, simulated maximum, minimum, and average keratometry (K), coma and spherical aberration, CCT, and endothelial cell density (ECD). All intra- and postoperative adverse events were recorded, and complete testing was repeated at three and 12 posttreatment time points, except spherical aberration, coma aberration, and root mean sphere.
UDVA and CDVA were recorded using a LogMAR Early Treatment Diabetic Retinopathy Study chart at 4 m. Pentacam topography (Oculus, Wetzlar, Germany) was used to evaluate pre- and postoperative corneal topography and pachymetry. Corneal endothelium was photographed using a noncontact specular microscope NonconRobo Sp-8000 (Konan), and ECD was calculated after marking at least 40 cells. Coma and spherical aberration and root mean squares were calculated using Eye Top (Costruzione Strumenti Oftalmici, Florence, Italy). Contact lens wearers were instructed to discontinue use of spherical soft lenses for a minimum of 4 weeks and soft toric, rigid gas-permeable and hard lenses for a minimum of 12 weeks before the preoperative eye examination. Epi-off CXL technique was performed under topical anesthesia instilling 4% lidocaine and 1.0% pilocarpine. Mechanical corneal epithelium removal over 9.0 mm was performed. Riboflavin (0.1% in 20% dextran solution; Ricrolin; Sooft, Montegiorgio, Italy) was administered topically every 2 minutes for 30 minutes and was continued every 2 minutes during UVA exposure. The cornea was exposed to UVA 370 nm light (UV-X System; Peschke Meditrade GmbH, Hünenberg, Switzerland) for 30 minutes at an irradiance of 3.0 mW/cm2. Ofloxacin and cyclopentolate drops were administered, and therapeutic contact lens (LAC ACUVUE-etafilcon A) were applied for 3 days after surgery. Patients were discharged with topical tobramycin to apply four times a day for 1 week, dexamethasone phosphate 0.1% four times a day for 2 weeks, then tapering to zero, and lubricating eye drops to use for the following 3 months. The epi-on CXL group was treated using following technique: corneal epithelial removal was not performed, and corneal imbibition was obtained with 0.1% riboflavin–15% dextran solution supplemented with Tris-hydroxymethylaminomethane and sodium ethylenediaminetetraacetic acid (Ricrolin TE; Sooft) by instillation of two drops every 5 minutes for 30 minutes at 3.0 mW/cm2. One drop of 1% pilocarpine was administered 30 minutes before treatment. Twenty minutes before UV radiation, the cornea was anesthetized with single-dose anesthetic eye drops (4% lidocaine). Postoperative corticosteroid drops were not instilled. All patients were operated by same surgeon.
A sample size of ten eyes was required to detect a difference of 0.75 D between the Kmax 12 months after treatment and at baseline, at a significance level of 0.05 and a power of 80%, assuming a standard deviation of 0.75 D. Data are expressed as mean ± standard deviation. Statistical analysis was performed by using MATLAB r2014a (MathWorks, Natick, MA, USA). In order to deal with non-normality of some data, differences between the two groups (at baseline and in treatment effect) were assessed using Wilcoxon rank sum test, while differences over the follow-up time points were evaluated by using Wilcoxon signed rank test with Bonferroni correction for multiple comparisons. A P-value <0.05 was considered statistically significant.
Results
The study sample consisted of 20 eyes of 20 patients. Ten eyes were treated with epi-off CXL (group A), and the other ten eyes were treated with epi-on CXL (group B) (). No significant differences in age and pachymetric and keratometric parameters between the two groups were assessed at baseline, while UDVA and CDVA were higher in the epi-off CXL group.
Table 1 Outcomes before and after epithelium-off CXL and TE-CXL
In group A, mean age was 30.4±7.3 years (range: 22–42 years). Mean baseline UDVA was 0.65 LogMAR (SD ±0.15 LogMAR). UDVA improvement (mean 0.64 LogMAR; SD ±0.09 LogMAR) observed at the 3-month postoperative time point became statistically significant (P<0.05) at the 12-month time point with median UDVA =0.49 LogMAR (SD ±0.03 LogMAR). Mean baseline CDVA was 0.22 LogMAR (SD ±0.04 LogMAR), and this value started to increase significantly from the 3-month postoperative time point (0.17 LogMAR; SD ±0.04 LogMAR; P<0.05). All topographic parameters (Kmin, Kmax, and mean K) showed a statistically significant improvement at 12 months post-surgery. The improvement in Kmin and Kmax over the follow-up is shown in and , respectively.
Figure 1 The simulated minimum keratometry (K) after epithelium-off CXL (A) and after epithelium-on CXL (B).
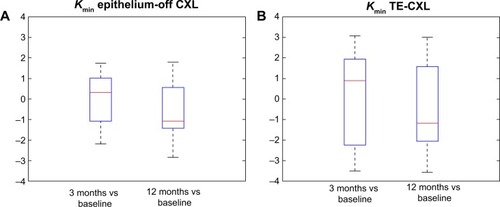
Figure 2 The simulated maximum keratometry (K) after epithelium-off CXL (A) and after epithelium-on CXL (B).
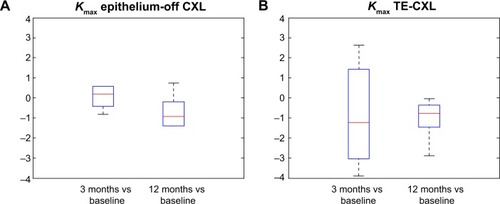
In group B, mean age was 28±3.8 years (range: 24–34 years). Median baseline UDVA was 0.88 LogMAR (SD ±0.19 LogMAR). UDVA improvement (median 0.87 LogMAR; SD ±0.18 LogMAR) recorded at 3 months became statistically significant (P<0.05) at 12 months post-surgery, when median UDVA was 0.75 LogMAR (SD ±0.19 LogMAR). Median baseline CDVA was 0.36 LogMAR (SD ±0.13 LogMAR) and increased significantly 12 months post-surgery (0.21 LogMAR; SD ±0.11 LogMAR; P<0.05). At the same time point, a statistically significant improvement was also recorded in topographic parameters (Kmin, Kmax, and mean K) ( and ), spherical error, SE, topographic astigmatism, apex keratometry, inferior–superior symmetry index, root mean sphere. CCT, ECD, coma aberration, and spherical aberration remained stable up to 12 months after treatment (P>0.05).
The treatment effect on the main clinical features between the two groups is compared in . No significant differences were observed between the groups A and B, with only exception of a higher improvement in CDVA in group B.
Table 2 Comparison of treatment effects between the two groups (epithelium-off CXL and TE-CXL)
No patients were lost at follow-up. During follow-up, no ocular or systemic adverse events were observed. No corneal edema, no haze, and no re-epithelialization delay were noticed.
Discussion
In this study, we analyzed refractive and functional outcomes after epi-off CXL and epi-on CXL in two groups of patients with progressive keratoconus. In order to assess the effectiveness of the two treatments, we removed all the confounding factors related to the patients, using the two techniques in two groups of patients with homogeneous characteristics at baseline. In fact, all eyes showed a CCT greater than 400 μm and homogeneous topographic and anatomical parameters (in a defined range of thickness and keratometry).Citation13,Citation23,Citation24 The aim of our study was to evaluate the efficacy of the two treatments in two homogeneous groups. Patients were randomly assigned to one of the two treatment groups. At 12 months posttreatment, our results showed that both procedures proved to be useful and effective in halting the progression of keratoconus, in accordance with previous reports.Citation13,Citation21,Citation24–Citation26 Furthermore, the results obtained using both procedures showed reduced mean SE and spherical error, improvement in UDVA and CDVA, and reduced topographic power after 12 months. Apex keratometry improvement highlighted the flattening of the corneal cone, as in other studies.Citation7,Citation10,Citation25 No significant variations were recorded in spherical aberration and coma aberration, and CCT remained constant in both groups at 12 months post-surgery. Vinciguerra et al pointed out a significant decrease in corneal pachymetry at 12 months, but this prospective study treated patients with advanced keratoconus.Citation27 The two most recent studies that analyze the effectiveness of epi-on CXL and epi-off CXL were performed by Caporossi et alCitation24 and Magli et al.Citation11 Caporossi et alCitation24 reported a study of 26 eyes treated by epi-on CXL, and they observed an initial, although not statistically significant, increase in UDVA and CDVA in the first 3 months. However, between the third and sixth postoperative months, their patients showed a gradual return to preoperative functional values associated with a progressive reduction in corneal thickness and the need for re-treatment with epi-off CXL in 50% of pediatric patients.Citation24 These study results therefore suggest that the epi-on technique should not be used in patients under 18 years of age. Magli et al reported the results of a study performed on two groups of patients using both techniques; all patients presented a corneal thickness greater than 400 μm and homogeneous topographic and anatomical parameters, but the patients treated were younger than the patients in our study (<18 years).Citation11 Both studies deal with the epi-on CXL technique in pediatric patients with discordant results. In our study, no patients needed re-treatment, and in both groups, a significant improvement in visual acuity and topographic parameter was observed. In fact, after treatment (12-month observation time point), 80% of our patients had a visual acuity greater than 0.2 LogMAR, highlighting the effectiveness of the technique epi-on CXL in adult patients.
No complications were recorded in either group. In the literature, several complications have been reported especially after epi-off CXL, such as corneal haze, melting, endothelial damage, and sterile infiltrate infections.Citation28–Citation31 In addition, we observed a significantly greater mean postoperative pain in the epi-off CXL group compared to the epi-on CXL group perhaps due to the exposure of corneal nerves and the release of inflammatory mediators, especially prostaglandins and neuropeptides after epithelium removal.
An overall analysis of the clinical outcomes after epi-off and epi-on CXL showed that keratoconus was relatively stable after 12 months, and no differences were observed comparing the two procedures. Despite the different penetration stroma demonstrated in other studies, we observed no clinical differences comparing the two groups. In addition, the risk of infection and pain in the group treated with epi-on CXL was much lower than in the epi-off CXL group. We believe that the lack of a unanimous agreement on the effectiveness of the CXL treatment is due to the presence of intrinsic confounding factors strictly related to the patients. In fact, as evidenced by some authors, effectiveness of CXL varies according to age and keratometry.Citation8,Citation32
Conclusion
The current study is the first that describes and compares the results of two CXL techniques performed on two groups of patients with homogeneous clinical and topographical characteristics, highlighting the effectiveness of the epi-on CXL technique in adult patients and proposing it as an alternative to the epi-off CXL. However, our work presents some limitations: the small number of treated eyes and a short follow-up length (12 months). For this reason, our results are not sufficient to assess the differences in efficacy and long-term stability between the two procedures, in particular, epi-on CXL. Further studies with a larger number of eyes and a longer follow-up length are needed to answer these questions.
Acknowledgments
The authors thank Dr Carmela Acerra (English native speaker) for linguistic revision of the manuscript and Dr Paolo Melillo for statistical analysis.
Disclosure
The authors report no conflicts of interest in this work.
References
- RabinowitzYSKeratoconusSurv Ophthalmol1998422973199493273
- AndreassenTTSimonsenAHOxlundHBiomechanical properties of keratoconus and normal corneasExp Eye Res1980314354417449878
- WollensakGWilschMSpoerlESeilerTCollagen fiber diameter in the rabbit cornea after collagen crosslinking by riboflavin/UVACornea20042350350715220736
- WollensakGIomdinaEBiomechanical and histological changes after corneal crosslinking with and without epithelial debridementJ Cataract Refract Surg20093554054619251149
- MencucciRMariniMGheriGLectin binding in normal, keratoconus and cross-linked human corneasActa Histochem201111330831620053427
- SpoerlEWollensakGSeilerTIncreased resistance of crosslinked cornea against enzymatic digestionCurr Eye Res200429354015370365
- VinciguerraPAlbèETrazzaSRefractive, topographic, tomographic, and aberrometric analysis of keratoconic eyes undergoing corneal cross-linkingOphthalmology200911636937819167087
- VinciguerraRRomanoMRCamesascaFICorneal cross-linking as a treatment for keratoconus: four-year morphologic and clinical outcomes with respect to patient ageOphthalmology201312090891623290750
- O’BrartDPKwongTQPatelPMcDonaldRJO’BrartNALong-term follow-up of riboflavin/ultraviolet A (370 nm) corneal collagen cross-linking to halt the progression of keratoconusBr J Ophthalmol20139743343723385632
- CaporossiAMazzottaCBaiocchiSCaporossiTLong-term results of riboflavin ultraviolet a corneal collagen cross-linking for keratoconus in Italy: the Siena eye cross studyAm J Ophthalmol201014958559320138607
- MagliAForteRTortoriACapassoLMarsicoGPiozziEEpithelium-off corneal collagen cross-linking versus transepithelial cross-linking for pediatric keratoconusCornea20133259760123132450
- GrewalDSBrarGSJainRSoodVSinglaMGrewalSPCorneal collagen crosslinking using riboflavin and ultraviolet-A light for keratoconus: one-year analysis using Scheimpflug imagingJ Cataract Refract Surg20093542545619251133
- FilippelloMStagniEO’BrartDTransepithelial corneal collagen crosslinking: bilateral studyJ Cataract Refract Surg20123828329122104644
- Raiskup-WolfFHoyerASpoerlEPillunatLECollagen crosslinking with riboflavin and ultraviolet-A light in keratoconus: long-term resultsJ Cataract Refract Surg20083479680118471635
- MazzottaCBalestrazziATraversiCTreatment of progressive keratoconus by riboflavin-UVA-induced cross-linking of corneal collagen: ultrastructural analysis by Heidelberg Retinal Tomograph II in vivo confocal microscopy in humansCornea20072639039717457184
- MazzottaCTraversiCBaiocchiSCorneal healing after riboflavin ultraviolet-A collagen cross-linking determined by confocal laser scanning microscopy in vivo: early and late modificationsAm J Ophthalmol200814652753318672225
- MazzottaCTraversiCBaiocchiSSergioPCaporossiTCaporossiAConservative treatment of keratoconus by riboflavin-UVA-induced cross-linking of corneal collagen: qualitative investigationEur J Ophthalmol20061653053516952090
- CaporossiAMazzottaCBaiocchiSCaporossiTParadisoALTransepithelial corneal collagen crosslinking for keratoconus: qualitative investigation by in vivo HRT II confocal analysisEur J Ophthalmol201222suppl 7S81S883022344471
- Al-AqabaMCaliennoRFaresUThe effect of standard and transepithelial ultraviolet collagen cross-linking on human corneal nerves: an ex vivo studyAm J Ophthalmol201215325826621930257
- XiaYChaiXZhouCRenQCorneal nerve morphology and sensitivity changes after ultraviolet A/riboflavin treatmentExp Eye Res20119354154721763309
- LeccisottiAIslamTTransepithelial corneal collagen crosslinking in keratoconusJ Refract Surg20102694294820166621
- BaiocchiSMazzottaCCerretaniDCaporossiTCaporossiACorneal crosslinking: riboflavin concentration in corneal stroma exposed with and without epitheliumJ Cataract Refract Surg20093589389919393890
- SpadeaLMencucciRTransepithelial corneal collagen cross-linking in ultrathin keratoconic corneasClin Ophthalmol201261785179223152657
- CaporossiAMazzottaCParadisoALBaiocchiSMariglianiDCaporossiTTransepithelial corneal collagen crosslinking for progressive keratoconus: 24-month clinical resultsJ Cataract Refract Surg2013391157116323790530
- WollensakGSpoerlESeilerTRiboflavin/ultraviolet-a-induced collagen crosslinking for the treatment of keratoconusAm J Ophthalmol200313562062712719068
- VinciguerraPAlbeETrazzaSSeilerTEpsteinDIntraoperative and postoperative effects of corneal collagen cross-linking on progressive keratoconusArch Ophthalmol20091271258126519822840
- SharmaANottageJMMirchiaKSharmaRMohanKNirankariVSPersistent corneal edema after collagen cross-linking for keratoconusAm J Ophthalmol2012154922–926e122959362
- RamaPDi MatteoFMatuskaSPaganoniGSpinelliAAcanthamoeba keratitis with perforation after corneal crosslinking and bandage contact lens useJ Cataract Refract Surg20093578879119304108
- RamaPDi MatteoFMatuskaSInsaccoCPaganoniGSevere keratitis following corneal cross-linking for keratoconusActa Ophthalmol201189e658e65921106042
- DhawanSRaoKNatrajanSComplications of corneal collagen cross-linkingJ Ophthalmol2011201186901522254130
- GreensteinSAHershPSCharacteristics influencing outcomes of corneal collagen crosslinking for keratoconus and ectasia: implications for patient selectionJ Cataract Refract Surg2013391133114023889865
- WollensakGSpoerlEWilschMSeilerTKeratocyte apoptosis after corneal collagen cross-linking using riboflavin/UVA treatmentCornea200423434914701957
