Abstract
Purpose
Opacification of hydrophilic acrylic intraocular lenses (IOLs) is an emerging complication following Descemet stripping automated endothelial keratoplasty (DSAEK). We report six cases and review the current literature.
Methods
In this retrospective, noncomparative, observational case series, patients with IOL opacification after previous DSAEK surgery were identified from corneal clinic records. Case notes were reviewed for demographic details, indication for DSAEK, IOL model, incidence of rebubbling, and postoperative course.
Results
Six patients developed IOL opacification after DSAEK. All patients had Fuchs’ endothelial dystrophy and had previously received hydrophilic acrylic IOL models. Central anterior IOL opacification was noted in all six cases. Five cases (83%) had required rebubbling due to dislocated graft tissue, and one had an early postoperative intraocular pressure (IOP) rise. Five cases (83%) were managed conservatively, and one case with a failed graft underwent redo DSAEK and IOL exchange.
Conclusion
Repeated exposure to intracameral air, raised IOP, and other patient influences may be major etiological factors for IOL opacification after DSAEK. We advise avoiding hydrophilic acrylic IOL models in patients who may require future endothelial keratoplasty.
Introduction
The surgical treatment of corneal endothelial pathology has changed significantly with the evolution of posterior lamellar keratoplasty techniques and Descemet stripping automated endothelial keratoplasty (DSAEK) is now widely performed as the procedure of choice for corneal decompensation secondary to endothelial dysfunction.Citation1 DSAEK is associated with excellent visual outcomes, with less corneal astigmatism and a more rapid visual recovery compared to traditional penetrating keratoplasty (PKP).Citation1,Citation2
Complications of DSAEK are well-described, although the most common adverse events do not appear to be detrimental to the ultimate visual outcome.Citation3 Reported complications include graft dislocation, graft rejection, primary graft failure, graft– host interface opacification, pupillary block, cystoid macular edema, and epithelial ingrowth.Citation2,Citation3 It has only recently become apparent that intraocular lens (IOL) complications may occur in pseudophakic patients undergoing DSAEK, with a number of recent reports describing late IOL opacification.Citation4–Citation10 We report a series of six cases of late-onset IOL opacification in pseudophakic patients after DSAEK surgery, and review the current literature on this emerging complication.
Methods
This study was a retrospective, noncomparative, observational case series. The institutional review board of the Research & Development Department, Heart Of England NHS Foundation Trust, Birmingham, UK, ruled that approval was not required for this report. We reviewed clinic records from patients attending the corneal service at Solihull Hospital, Heart of England NHS Foundation Trust, Birmingham, UK. Pseudophakic patients who had undergone DSAEK and later diagnosed with IOL opacification between January 2010 and April 2014, inclusive, were identified from clinic records. Charts were reviewed for demographic data, diagnosis/indication for DSAEK, ocular comorbidity, date of prior cataract surgery, details of IOL implant, date and perioperative details of DSAEK surgery, and postoperative management. For patients who had undergone surgery at another institution before transfer of their case to our clinic, all surgical and perioperative records for both cataract and corneal procedures were obtained for these patients from the referring center.
Results
A total of six patients were identified with IOL opacification following DSAEK: three (50%) were male and the mean age was 75.6 years (range 71–81 years). Five of the patients had undergone DSAEK elsewhere, and had subsequently transferred to our unit for ongoing management. We are therefore unable to accurately calculate the incidence from our series. Indication for DSAEK was corneal decompensation secondary to Fuchs’ endothelial dystrophy (FED) in all cases, and all had previously undergone cataract surgery and implantation of hydrophilic acrylic IOL models. Five cases (83%) had required intracameral air injection (‘rebubbling’) for donor graft dislocation in the early postoperative (1–5 days) period. One patient who did not require rebubbling had a postoperative intraocular pressure (IOP) spike on day 2 post-DSAEK, which was managed with oral and topical antihypertensive medical therapy. This patient subsequently developed a corticosteroid-induced rise in IOP 3 months post-operatively, which settled after a switch to a less potent corticosteroid preparation. The standard postoperative medication regime after DSAEK included topical preservative-free 0.1% dexamethasone six times daily and 0.5% chloramphenicol four times daily for 4 weeks, and subsequently 0.1% dexamethasone four times daily for 3 months, tapered over 3 months, and maintained on long-term 0.1% fluorometholone (FML). In all cases, IOL opacification was a central, crystalline opacity within the pupillary margin, diagnosed on average 32 months (range 5–80 months) after DSAEK. Five (83%) patients have been managed conservatively, and one patient with a subsequently failed corneal graft has recently undergone IOL exchange and redo DSAEK. Demographic, clinical, and relevant postoperative details are summarized in . Clinical images of two patients are illustrated in and , respectively.
Figure 1 IOL opacification after DSAEK (Case 4).
Abbreviations: DSAEK, Descemet stripping automated endothelial keratoplasty; IOL, intraocular lens.
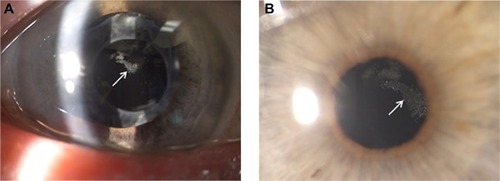
Figure 2 IOL opacification after DSAEK (Case 5).
Abbreviations: DSAEK, Descemet stripping automated endothelial keratoplasty; IOL, intraocular lens.
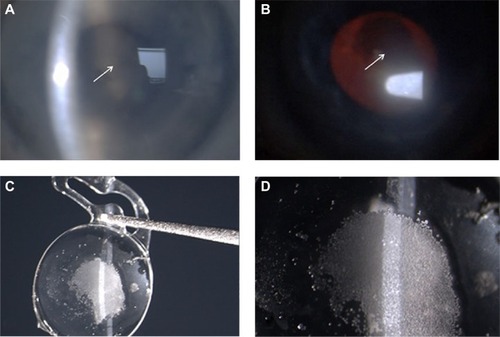
Table 1 Summary of six cases of IOL opacification after DSAEK
Discussion
Opacification of IOLs is well-described and associated with many factors, including IOL production processes, surgical techniques, and metabolic conditions.Citation11,Citation12 There are recent reports of hydrophilic acrylic IOL opacification as an emerging late complication of DSAEK ().Citation4–Citation10 We identified six cases of central IOL opacification in pseudophakic patients after undergoing DSAEK for corneal decompensation secondary to FED. Whilst the pathophysiology is incompletely understood, several features are evident that may enable greater comprehension of this phenomenon and result in changes to practice.
Table 2 Summary of published reports of post-DSAEK IOL opacification
Anterior central IOL opacification after DSAEK was first described in three cases presenting between 7 and 18 months postoperatively.Citation5 A further case presenting approximately 18 months after a combined redo DSAEK and phacoemulsification with hydrophilic IOL underwent IOL explantation,Citation9 and analysis confirmed granular calcification in the central zone of the anterior IOL optic. Calcification has been a common feature of all the explanted IOLs analyzed and confirmed by X-ray spectroscopy and calcium-specific staining methods such as alizarin red.Citation4,Citation7–Citation10 Histological examination of the explanted IOL from our Case 5 confirmed the presence of dystrophic calcification ().
Our six patients had all been implanted with hydrophilic acrylic IOL models prior to undergoing DSAEK (), and published cases have also been exclusively associated with hydrophilic acrylic IOLs (). These IOLs all have a similar water content of 25.5%–26%, although different acrylic polymer compositions, suggesting that the class of IOL is important for the development of opacification, rather than the IOL model per se. Despite macroscopically similar clinical appearances of IOL calcification reported after intraocular gas, there are some differences in the microscopic appearance of the crystalline deposits between different IOL models, possibly reflecting the individual IOL polymer ultrastructure.Citation6–Citation11
The use of intracameral air is an integral part of DSAEK surgery and rebubbling of an incompletely adherent graft in the early postoperative period is reported in the majority of cases that have developed IOL opacification (), suggesting that repeated exposure of the hydrophilic IOL to intracameral air is responsible. Consistently, five cases in our series (83%) required repeat intracameral air injection within the first postoperative week. The largest series to date of IOL opacification after keratoplasty reported ten cases, including seven after DSAEK, one after deep anterior lamellar keratoplasty (DALK), and two after PKP.Citation7 Six of the DSAEK cases (86%) underwent at least one rebubbling and the DALK case reported was also exposed to repeated intracameral air injections. A recent report described early postoperative rebubbling in all four cases of opacification of Rayner hydrophilic acrylic IOL models after DSAEK, accounting for 40% of cases rebubbled in this series.Citation10 Repeated exposure of hydrophilic IOLs to intracameral air or gas is therefore likely to be a major contributory factor to the development of calcification, and has also been described in other cases of IOL opacification, such as after SF6 and C3F8 gas fill for treatment of Descemet membrane detachment after cataract surgery.Citation13 Anterior central opacification with sparing of the posterior and peripheral IOL optic is a common feature and the pattern of opacification in our cases is comparable ( and ). The distribution of calcification has been attributed to the presence of intracameral gas/air in contact with the anterior IOL surface and relative protection of the peripheral IOL by the iris.Citation6 Interestingly, one case reportedly had a small area of opacification outside the pupillary region, corresponding to an area of preexisting iris atrophy, further supporting the notion of an etiological factor within the anterior chamber.Citation6 The repeated presence of gas or air in the anterior chamber may induce ultrastructural changes on the IOL optic surface within the pupil margin, leading to increased IOL permeability to anterior chamber factors that combine with the IOL material to act as a focus for calcification.Citation6,Citation8 As newer surgical modifications and instruments are being developed, Descemet membrane endothelial keratoplasty (DMEK) has been gaining popularity, although it is associated with high graft detachment rates of up to 63% in the early surgical learning curve.Citation14 Whilst this rate tends to improve with experience,Citation15 IOL opacification may be a potentially greater problem for surgeons performing DMEK or converting from DSAEK, which is associated with a lower incidence of graft dislocations.Citation3,Citation15
Factors other than the repeated presence of intracameral air may also contribute to the development of IOL opacification, as not all reported cases of post-DSAEK IOL calcification have been rebubbled in the postoperative period.Citation5,Citation7,Citation9 IOL opacification is not an inevitable sequel to rebubbling. For example, a series examining 29 DSAEK cases requiring rebubbling did not mention IOL opacity,Citation16 and several smaller series of donor graft dislocations being managed with rebubbling have similarly failed to describe IOL changes.Citation17,Citation18 Use of hydrophobic acrylic or other IOL materials in these cohorts, underreporting of IOL complications, or other factors may account for the lack of IOL opacification described.
Prolonged breakdown of the blood–aqueous barrier (BAB) has been suggested as a contributory factor in IOL opacification, with air or postoperative inflammation inducing a metabolic change in the anterior chamber, leading to an increase in aqueous protein, cells, and calcium content.Citation5,Citation7 Repeated air/gas tamponade may then drive calcium-rich aqueous into hydrophilic IOL substance with subsequent crystallization.Citation6,Citation8 One of the cases in our cohort (Case 5) developed IOL opacification in an eye in which the endothelial graft had failed several years previously, and it is therefore possible that prolonged low-grade intraocular inflammation was unidentified behind a cloudy cornea. Of note, this patient developed significant band keratopathy which required laser phototherapeutic keratectomy (PTK) in the 2 years after DSAEK. He had a past medical history of inflammatory bowel disease, requiring surgical colectomy, and had also previously been prescribed antipsychotic medication, and these factors may have influenced his metabolic status and propensity to calcification, although systemic calcium levels were not raised.
The postoperative course of published cases has been variable. Of the three cases reported by Patryn et alCitation5 only one had been rebubbled, and the other two had very minimal and short-lived intraocular inflammation. The seven DSAEK case series all had complicated postoperative courses with rebubbling and intraocular inflammation, and even the one case that was not rebubbled had a prolonged anterior chamber inflammatory reaction and posterior synechiae.Citation7 Schmidinger et al reported the presence of posterior synechiae in their case, which did not undergo rebubbling.Citation9 Our single case (Case 4) who did not require rebubbling had a spike in IOP in the immediate postoperative period and a later corticosteroid-induced IOP rise. Whilst the influence of raised IOP has not been widely considered, it is possible that IOP raised above a certain threshold may be an initiating event for anterior chamber factors to induce IOL calcification. We cannot rule out the possibility that IOP or antiglaucoma medications may be contributing factors. Thus, prolonged intraocular inflammation, raised IOP, or other patient metabolic factors may increase the risk of developing IOL opacification after DSAEK.
Whilst there are many indications for endothelial transplantation, all the patients we identified had a diagnosis of FED. Furthermore, over 90% of reported cases have occurred in FED patients (),Citation4–Citation10 although IOL opacification after DSAEK has also been described in patients with pseudophakic bullous keratopathy and Axenfeld–Rieger’s anterior segment dysgenesis.Citation8,Citation19 It is possible that the underlying ocular condition itself may play a role in the pathogenesis of IOL opacification after DSAEK. FED is not considered to be an inflammatory disease, but it is conceivable that differences in aqueous humor proteome in FED patients could predispose to IOL calcification.Citation20 Furthermore, differential expression of genes related to ion transport, pump function, and stress response has been reported in the corneal endothelium of FED patients compared to normal controls.Citation21 Altered expression of aquaporins and solute transporters has also been reported in FED and PBK patients and further understanding of the genetic basis of corneal endothelial conditions may reveal other potential patient-related factors.Citation22,Citation23
Management of IOL opacification after DSAEK depends on the nature of the patient’s symptoms. Where intervention is indicated, neodymium-doped yttrium aluminum garnet (Nd:YAG) laser has failed to disperse the calcification opacity ().Citation4–Citation9 However, it should be considered that Nd:YAG laser treatment of the posterior capsule may compromise a safe IOL exchange if subsequently required.Citation7 Attempts to surgically remove the opacity have also failed (),Citation5–Citation9 reflecting the fact that the opacity is not merely a surface membrane but calcification within the IOL substance. IOL exchange is the only intervention that has enabled visual improvement (),Citation4–Citation10 and may require iris-fixated or sutured/glued IOL in cases where capsular integrity is insufficient for in-the-bag or sulcus implantation.Citation8,Citation24
In summary, we report six cases of IOL opacification after DSAEK, of which the majority required rebubbling of the dislocated donor endothelial graft in the early postoperative period. Repeated exposure to intracameral air is likely to be a significant etiological factor, although excessive postoperative inflammation, raised IOP, or other local or systemic factors may also contribute. Steps should be taken to minimize IOP spikes and inflammation. We suggest that hydrophilic IOL models should be avoided in patients undergoing cataract surgery who are at risk of postoperative corneal decompensation. Furthermore, as lamellar keratoplasty is now the treatment of choice for endothelial dysfunction, it is important that clinicians are alert to the emergence of this newly reported late complication in pseudophakic patients with hydrophilic IOLs.
Acknowledgments
This manuscript is derived from a poster abstract submitted to the American Academy of Ophthalmology, Chicago, IL, USA, October 18–21, 2014.
Disclosure
The authors report no conflicts of interest in this work.
References
- PriceMOPriceFWDescemet’s stripping endothelial keratoplastyCurr Opin Ophthalmol200718429029417568204
- National Institute for Health and Care ExcellenceCorneal endothelial transplantation [IPG304]2009110 Available from: https://www.nice.org.uk/guidance/ipg304Accessed January 6, 2015
- LeeBLJacobsDSMuschDCKaufmanSCReinhartWJShteinRMDescemet’s stripping endothelial keratoplasty: safety and outcomes: a report by the American Academy of OphthalmologyOphthalmology200911691818183019643492
- WernerLWilbanksGOllertonAMichelsonJLocalized calcification of hydrophilic acrylic intraocular lenses in association with intracameral injection of gasJ Cataract Refract Surg201238472072122305709
- PatrynEvan der MeulenIJLapid-GortzakRMouritsMNieuwendaalCPIntraocular lens opacifications in Descemet stripping endothelial keratoplasty patientsCornea201231101189119222236784
- DhittalASpaltonDJGoyalSWernerLCalcification in hydrophilic intraocular lenses associated with injection of intraocular gasAm J Ophthalmol2012153611541160 e122325304
- NeuhannIMNeuhannTFRohrbachJMIntraocular lens calcification after keratoplastyCornea2013324e6e1023010776
- FellmanMAWernerLLiuETCalcification of a hydrophilic acrylic intraocular lens after Descemet-stripping endothelial keratoplasty: case report and laboratory analysesJ Cataract Refract Surg201339579980323541897
- SchmidingerGPempBWernerLOpacification of an intraocular lens: calcification of hydrophilic intraocular lenses after gas tamponade of the anterior chamberOphthalmologe20131101110661068 German23552856
- De CockRFajgenbaumMACalcification of Rayner hydrophilic acrylic intra-ocular lenses after Descemet’s stripping automated endothelial keratoplastyEye (Lond)201428111383138425081295
- WernerLCauses of intraocular lens opacification or discolorationJ Cataract Refract Surg200733471372617397749
- WernerLCalcification of hydrophilic acrylic intraocular lensesAm J Ophthalmol2008146334134318724977
- SaeedMUSinghAJMorrellAJSequential Descemet’s membrane detachments and intraocular lens haze secondary to SF6 or C3F8Eur J Ophthalmol200616575876017061232
- PriceMOGiebelAWFairchildKMPriceFWJrDescemet’s membrane endothelial keratoplasty: prospective multicenter study of visual and refractive outcomes and endothelial survivalOphthalmology2009116122361236819875170
- DirisamerMHamLDapenaIEfficacy of descemet membrance endothelial keratoplasty; clinical outcome of 200 consecutive cases after a learning curve of 25 casesArch Ophthalmol2011129111435144321746971
- ClementsJLBouchardCSLeeWBRetrospective review of graft dislocation rate associated with descemet stripping automated endothelial keratoplasty after primary failed penetrating keratoplastyCornea201130441441821099405
- TerryMAHoarKLWallJOusleyPHistology of dislocations in endothelial keratoplasty (DSEK and DLEK): a laboratory-based, surgical solution to dislocation in 100 consecutive DSEK casesCornea200625892693217102669
- BaharIKaisermanIMcAllumPSlomovicARootmanDComparison of posterior lamellar keratoplasty techniques to penetrating keratoplastyOphthalmology200811591525153318440638
- ParkJHabibNOpacification of IOL implants following endothelial keratoplastyPaper presented at: Congress of the ESCRSOctober 2013Amsterdam, Netherlands
- RichardsonMRSeguZMPriceMOAlterations in the aqueous humor proteome in patients with Fuchs endothelial dystrophyMol Vis2010162376238321139973
- GottschJDBowersALMarguliesEHSerial analysis of gene expression in the corneal endothelium of Fuchs’ dystrophyInvest Ophthalmol Vis Sci200344259459912556388
- KenneyMCAtilanoSRZorapapelNHolguinBGasterRNLjubimovAVAltered expression of aquaporins in bullous keratopathy and Fuchs’ dystrophy corneasJ Histochem Cytochem200452101341135015385580
- VithanaENMorganPERamprasadVSLC4A11 mutations in Fuchs endothelial corneal dystrophyHum Mol Genet200817565666618024964
- KumarDAAgarwalAGlued intraocular lens: a major review on surgical technique and resultsCurr Opin Ophthalmol2013241212923080013
