Abstract
An 84-year-old female with a history of hypertension and dyslipidemia was referred for a retinal artery macroaneurysm with exudation that had extended into the macula. She underwent a total of six injections of bevacizumab, with some improvement in visual acuity and retinal thickness. Due to persistent macular edema, focal laser photocoagulation was performed around the macroaneurysm. The vision remained at 20/30 during 20 months of follow up. Although anti-vascular endothelial growth factor therapy may improve vision and decrease retinal thickness in retinal artery macroaneurysm, recalcitrant cases may be treated with laser photocoagulation to seal the leaking vessel.
Introduction
Retinal artery macroaneurysms (RAMs) are rare, acquired dilatations of the retinal arterial vasculature, usually within the first three branches of the arteriolar tree.Citation1 The incidence is estimated to be approximately 1 in 4,500 people over the age of 40.Citation2 Hypertension and older age lead to hyaline degeneration of the vascular walls, loss of autoregulatory tone and elastic recoil, and arterial dilatation.Citation3
Approximately 8%–25% of RAMs will undergo spontaneous involution. Even with submacular hemorrhage, up to 37% of patients will have better than 20/40 visual acuity without treatment.Citation4 However one third of patients will develop vascular leakage and retinal edema and may need treatment.Citation5
Case report
An 84-year-old female with a past medical history of hypertension and dyslipidemia was referred for progressively decreasing visual acuity in the left eye. She had no history of diabetes. On initial examination, her visual acuity was 20/30 in both eyes. Dilated fundus examination and fluorescein angiography of the left eye revealed a superotemporal retinal arterial macroaneurysm, with surrounding circinate exudates involving the fovea ( and ). The right eye was normal.
Figure 1 Fluorescein angiography and fundus photographs.
Abbreviations: RAM, retinal artery macroaneurysm; VEGF, vascular endothelial growth factor.
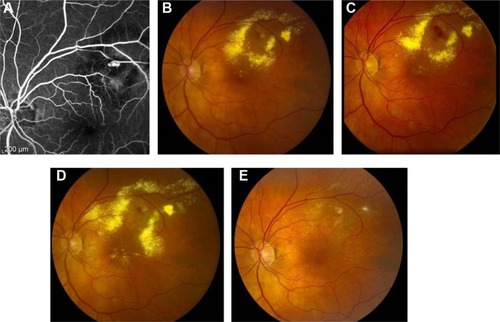
Figure 2 Progression on OCT.
Abbreviations: CFT, central foveal thickness; OCT, optical coherence tomography; ILM, Internal limiting membrane; RPE, retinal pigment epithelium; S, superior; I, inferior; N, nasal; T, temporal.
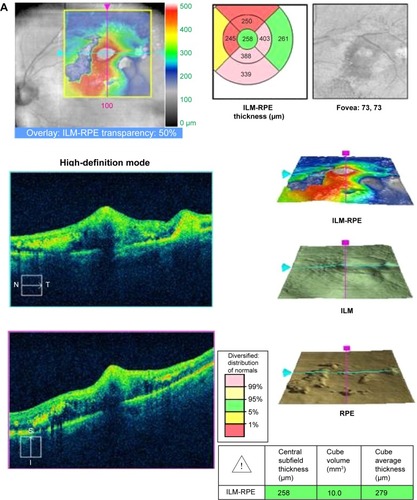
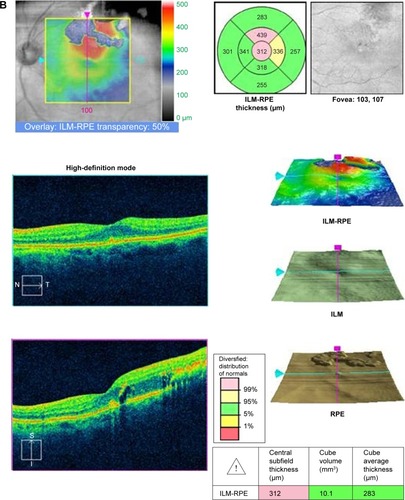
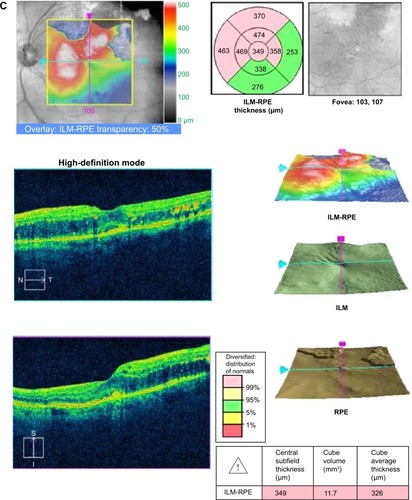
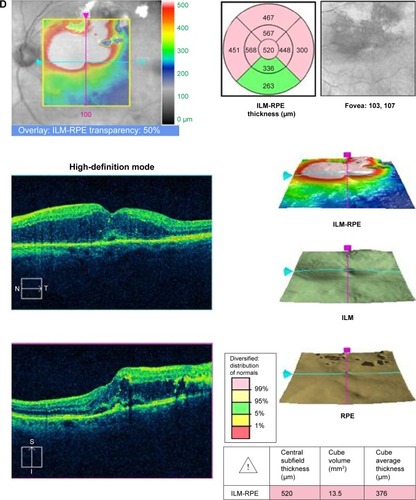
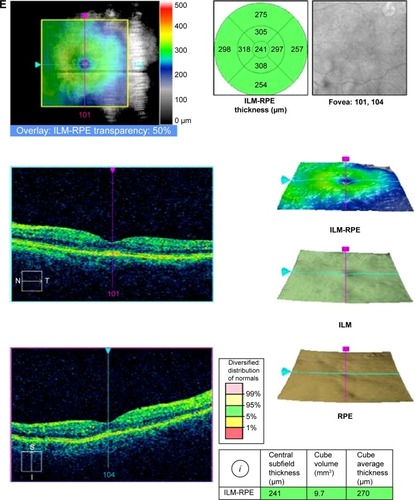
The patient was observed initially, but the edema increased and her vision deteriorated to 20/60. An intravitreal injection of 1.25 mg of bevacizumab improved the vision to 20/30. The patient was observed for 3 months, but the vision worsened again to 20/60, with increased edema and exudates on optical coherence tomography. She was observed for 3 months, but due to recurrent leakage, she ultimately received a total of six injections of intravitreal bevacizumab every 1 month to 3 months. Her vision gradually improved back to 20/30.
Fourteen months after initial presentation, her vision deteriorated again to 20/60. The decision was made to perform laser photocoagulation around the macroaneurysm. Argon laser at a setting of 400 mW and 200 μm spot size was applied around the RAM. The RAM occluded, and on follow-up examination 6 months later, the patient’s vision has remained at 20/30.
Discussion
The first report of laser photocoagulation to treat exudative retinal artery macroaneurysm was published in 1976 by Dr Donald Gass and colleagues.Citation6 In a study of 27 patients with symptomatic RAM, half of the patients underwent argon laser therapy and the remaining half was observed. The vision in both groups improved, but the laser group experienced a greater gain.Citation7 Approximately 16%–27% of RAMs occlude with lasers, but there is a risk of vascular occlusion, early increase in exudates from selective reabsorption of fluid, arteriovenous shunts, macular pucker, and scotomas.Citation7,Citation8 Other treatment options for RAMs include yellow dye laser and indocyanine green dye-enhanced photocoagulation.Citation9,Citation10
Anti-vascular endothelial growth factor (VEGF) therapy has recently been reported in the treatment of patients with exudative or hemorrhagic RAMs. Chanana and AzadCitation11 published the first case report in 2009, and subsequent case reports have shown encouraging results ().Citation12–Citation19 Cho et alCitation18 described 23 patients with RAMs who were either observed or received intravitreal bevacizumab. Both groups experienced statistically significant improvements in visual acuity and central macular thickness, but the bevacizumab group regained vision faster. A larger, prospective study of 38 eyes with hemorrhagic and exudative RAMs underwent three monthly injections of bevacizumab, with the vision and retinal thickness improving in both groups.Citation19
Table 1 Literature review of anti-VEGF use in the treatment of retinal artery macroaneurysms
The role of VEGF and the mechanism of action of anti-VEGF therapy in RAMs are not fully understood. In a study that compared the VEGF levels in 500 μL vitreous samples from patients with vitreous hemorrhage from nondiabetic etiologies (including four patients with RAM) with those from patients with proliferative diabetic retinopathy, the VEGF levels were significantly lower in the former than in the latter groups (2.75 pg/mL vs 821 pg/mL, respectively).Citation20 However, these were small vitreous samples obtained up to 3 weeks after the initial hemorrhage and may not have been representative of the vitreous and microenvironment around the RAM.
The role of VEGF in intracranial aneurysms and other biological systems has been more clearly elucidated. In intracranial aneurysms, VEGF levels were found to be significantly higher than the levels in controls.Citation20 In particular, patients with intracranial aneurysms had higher expressions of VEGF receptor 2 (VEGFR2) and lower levels of VEGF receptor 1 (VEGFR1). VEGFR1 is associated with angiogenesis, while VEGFR2 is associated with thrombosis.Citation21 Bevacizumab has been shown to decrease VEGFR1 levels and to increase VEGFR2 levels to normal levels in cancer cells.Citation22 In the circulatory system, platelets produce VEGF, which stimulates nitrous oxide production, resulting in vasodilation.Citation21 Inhibition of VEGF may decrease leakage of fluid and exudates through the endothelium. In mice studies, bevacizumab decreases bleeding time and increases coagulation.Citation23 Thus, VEGF inhibition may block angiogenesis, decrease binding of the prothrombotic VEGFR2, and decrease vascular permeability.
In conclusion, the majority of RAMs can be observed, but intervention may be necessary in cases of persistent or recurrent macular edema from exudative or hemorrhagic RAMs. Our patient’s RAM was initially observed, but continued leakage prompted further therapy.
Anti-VEGF injections have shown promise in improving visual acuity and hastening resolution of macular edema in RAM;Citation5 however, most of the previously published cases had relatively short follow-up. Our case has one of the longest follow-ups with the most number of anti-VEGF treatments, but the patient continued to have leakage into the macula. The potential benefits of anti-VEGF treatment must be carefully weighed against the potential risk of infection from serial injections. Laser photocoagulation remains a viable treatment option in cases of macular edema secondary to RAM.
Disclosure
The authors report no conflicts of interest in this work.
References
- LavinMJMarshRJPeartSRehmanARetinal arterial macroaneurysms: a retrospective study of 40 patientsBr J Ophthalmol198771118178253689733
- XuLWangYJonasJBFrequency of retinal macroaneurysms in adult Chinese: the Beijing eye studyBr J Ophthalmol200791684084117510482
- FichteCStreetenBWFriedmanAHA histopathologic study of retinal arterial aneurysmsAm J Ophthalmol1978854509518655232
- McCabeCMFlynnHWJrMcLeanWCNonsurgical management of macular hemorrhage secondary to retinal artery macroaneurysmsArch Ophthaolmol20001186780785
- RabbMFGalianoDATskeMPRetinal arterial macroaneurysmsSurv Ophthalmol198833273963055391
- LewisRANortonEWGassJDAcquired arterial macroaneurysms of the retinaBr J Ophthalmol197660121301268157
- MeyerJCAhmadBUBlinderKJShahGKLaser therapy versus observation for symptomatic retinal artery macroaneurysmsGraefes Arch Clin Exp Ophthalmol Epub 2014713
- BrownDMSobolWMFolkJCWeingeistTARetinal arterial macroaneurysm: long term visual outcomeBr J Ophthalmol1994785345387918263
- RussellSRFolkJCBranch retinal artery occlusion after dye yellow photocoagulation of an arterial macroaneurysmAm J Ophthalmol198710421861873618718
- SteigerwaltRDJrPascarellaAArricoLIdiopathic juxtafoveal retinal telangiectasis and retinal macroaneurysm treated with indocyanine green dye-enhanced photocoagulationPanminerva Med2012541 suppl 4939623241941
- ChananaBAzadRVIntravitreal bevacizumab for macular edema secondary to retinal arterial macroaneurysmEye (Lond)200923249349418388958
- JonasJBSchmidbauerMIntravitreal bevacizumab for retinal macroaneurysmActa Ophthalmol2010887e28420977692
- JaveyGMoshfeghiANMoshfeghiAAManagement of ruptured retinal arterial macroaneurysm with intravitreal bevacizumabOphthalmic Surg Lasers Imaging20104141521728252
- WenksternARPetersenHIntravitreal ranibizumab in retinal macroaneurysmGraefes Arch Clin Exp Ophthalmol2010248111667167020508944
- GolanSGolderbergDGoldsteinMLong-term follow-up of intravitreal bevacizumab in retinal arterial macroaneurysm: a case reportCase Rep Ophthalmol20112338739122220164
- TsakpinisDNasrMBTranosPThe use of bevacizumab in a multilevel retinal hemorrhage secondary to retinal macroaneurysm: a 39-month follow-up case reportClin Ophthalmol201151475147722069349
- ZweifelSATonzMSPfenningerLBeckerMMichelsSIntravitreal anti-VEGF therapy for retinal macroaneurysmKlin Monbl Augenheilkd2013230439239523629789
- ChoHJRheeTKKimHSIntravitreal bevacizumab for symptomatic retinal arterial macroaneurysmAm J Ophthalmol2013155589890423385203
- PichiFMoraraMTorrazzaCIntravitreal bevacizumab for macular complications from retinal arterial macroaneurysmsAm J Ophthalmol20131552287.e 294.e23111179
- ShirasawaMArimuraNOtsukaHSonodaSHashiguchiTSakamotoTIntravitreous VEGF-A in eyes with massive vitreous hemorrhageGraefes Arch Clin Exp Ophthalmol2011249121805181021853228
- MadernaECorsiniEFranziniAExpression of vascular endothelial growth factor receptor-1/-2 and nitric oxide in unruptured intracranial aneurysmsNeurol Sci201031561762320635108
- ZhangZNeivaKGLingenMWEllisLMNorJEVEGF-dependent tumor angiogenesis requires inverse and reciprocal regulation of VEGFR1 and VEGFR2Cell Death Differ201017349951219834490
- LiuXHaoLZhangSGenetic repression of mouse VEGF expression regulates coagulation cascadeIUBMB Life2010621181982421086498
