Abstract
Aim
This study aimed to assess the diagnostic ramifications of vascular occlusion of the ocular vein and artery as a first thrombotic event associated with factor V Leiden (FVL) and/or prothrombin gene (PTG) heterozygosity.
Methods
Patients with ocular vein (n=191) and artery (n=74) occlusion, free of cardioembolic etiologies, were sequentially referred from vitreoretinal specialists for measurement of thrombophilia-hypofibrinolysis and compared to 110 healthy normal controls.
Results
Of the 265 patients, 29 (11%; 17 women, 12 men) of all referred ocular vascular occlusion (OVO) cases were found to be heterozygous for FVL and/or PTG, including 16 with FVL, 12 with PTG, and 1 with both. Of the 29 cases, 16 had central retinal vein occlusion (CRVO), 2 branch retinal vein occlusion (BRVO), 5 nonarteritic anterior ischemic optic neuropathy (NA-AION), 3 retinal artery occlusion (RAO), 2 amaurosis fugax (AF), and 1 had both CRVO and RAO. Of the 16 FVL cases, 15 (94%) had OVO as a first thrombotic event without prior deep venous thrombosis (DVT) or pulmonary embolism (PE); 6 (38%) also had other thrombotic events, including recurrent miscarriage, osteonecrosis, ischemic stroke, and/or ischemic colitis; and 5 (31%) had immediate family members with previous venous thromboembolism (VTE). Of the 12 PTG cases, 9 (75%) had OVO as a first thrombotic event, 5 (42%) experienced VTE other than DVT or PE, and 6 (50%) had immediate family members with VTE. In one patient with both FVL and PTG, DVT occurred before BRVO. Of the 17 women with FVL and/or PTG mutations, 7 (41%) experienced ≥1 miscarriage, 6 (35%) were on estrogen therapy, and 1 (6%) was on clomiphene.
Conclusion
Of the 265 patients with OVO, 29 (11%) had FVL and/or PTG, and 83% of these 29 cases presented with OVO as their first thrombotic event. By diagnosing thrombophilia as an etiology for OVO, the ophthalmologist opens a window to family screening and preventive therapy.
Introduction
Retinal vein occlusions (RVOs), retinal artery occlusions (RAOs), and ciliary artery occlusions causing optic nerve infarction or anterior ischemic optic neuropathy (AION) are well-recognized vascular ischemic events that affect the posterior segment of the eye. RVO is widely prevalent,Citation1–Citation4 with 5.20 cases per 1,000 people (95% confidence interval [CI]: 4.40–5.99) in the USA, Europe, Asia, and Australia as in 2010, suggesting that roughly 16 million people may have this disorder.Citation4 AION is less common, with a median age of 62 and a mean annual incidence rate of 2.3 per 100,000 people for nonarteritic AION (NA-AION) and 0.36 per 100,000 people for arteritic AION (A-AION).Citation5 Central retinal artery occlusion (CRAO), which causes retinal infarction, is slightly rarer, estimated to be 1 in 100,000 people and roughly 1 in 10,000 outpatient visits, but it may result in severe vision loss in up to 80% of patients.Citation6
The presentation of ocular vascular occlusion (OVO), including RAO, RVO or AION, is widely variable and may range from an incidental finding in asymptomatic patients to partial visual field loss, diminished or absent central vision, or diminished or complete loss of vision resulting from either one or a combination of the following: optic nerve infarction, retinal infarction, macular edema, macular ischemia, and/or neovascular glaucoma.Citation7,Citation8 Because OVO has the potential for such devastating complications, including permanent vision loss, it is important to identify the etiology of the patient’s OVO to implement the appropriate treatment and to provide available prophylactic measures to prevent subsequent contralateral ocular and/or systemic thrombotic events.
Recognized risk factors for OVO are categorized as systemic or local. Systemic factors include hyperviscosity, myeloproliferative disorders, retro-orbital mass effect, and vasculitis such as Behcet’s disease.Citation7,Citation9 A common local finding predisposing to OVO is open-angle glaucoma. Glaucoma decreases venous outflow through increased intraocular pressure, thus creating vascular stasis and increased risk of occlusion, in accordance with Virchow’s triad.Citation10–Citation13 When commonly recognized etiologies are ruled out, other risk factors for OVO must be assessed, including cardiovascularCitation13–Citation23 and hypercoagulable stateCitation9,Citation24,Citation25 risk factors.
The most recognized, but neither sensitive nor specific, cardiovascular risk factors for OVO include age, history of smoking, hypertension, hyperlipidemia, diabetes mellitus, and atherosclerosis.Citation13–Citation23 More recently, however, there has been increased focus on the pathoetiologic role of thrombophilia in OVO. In the absence of a cardioembolic etiology for OVO, thrombophilia is a common, major cause of ocular thrombotic events.Citation9,Citation24 In particular, thrombophilia should be carefully assessed in younger patients, <65 years old, or in patients with a personal or family history of thrombosis.Citation25
Thrombophilia can be heritable – such as in hyperhomocysteinemia, factor V Leiden (FVL) mutation, prothrombin (PTG) G20210A mutation, antithrombin III deficiency, protein C deficiency, or protein S deficiency – or acquired, particularly the lupus anticoagulant found in antiphospholipid syndrome. Of the thrombophilias that are risk factors for OVO,Citation7,Citation16,Citation20,Citation21,Citation24,Citation26–Citation37 hyperhomocysteinemia is the most likely to cause OVOCitation7,Citation20,Citation24,Citation32–Citation37 and is a recognized risk factor for systemic vascular thrombosis, including ischemic heart disease and deep venous thrombosis (DVT).Citation38,Citation39 In addition to hyperhomocysteinemia, FVL and PTG heterozygosity result in a systemic hypercoagulable state and are major risk factors for large-vein thrombosis, and thus their role in OVO deserves careful attention.Citation32,Citation40–Citation43
The FVL mutation involves a G-A substitution at nucleotide 1691 on the factor V gene, resulting in a procoagulant state caused by factor V’s resistance to inactivation by protein C.Citation28,Citation44 This is one of the commonest familial thrombophilias, witĥ ~5% of Caucasian populations being heterozygous for the mutation.Citation45 Multiple studies, including case–control studies and a meta-analysis,Citation21,Citation24,Citation26–Citation28 have shown a significant increase in the prevalence of FVL in patients with OVO.
The PTG mutation is a G-A transition at nucleotide 20210 of the factor II gene and is associated with increased plasma prothrombin, resulting in a procoagulant state.Citation42 Similar to FVL, the PTG mutation has a high-level carrier prevalence of 1%–4% and is more common among people of Caucasian descent.Citation46 In addition, the PTG mutation, similar to the FVL mutation, is associated with venous thromboembolism (VTE),Citation40,Citation47,Citation48 and recent literature has illustrated its significant role in mediating OVO.Citation28,Citation49
Thrombophilia and its role in OVO have received more attention in recent years, particularly in younger patients and in patients without an obvious cardiac, carotid, or embolic etiology. Particularly in Caucasian populations, the FVL and PTG mutations are some of the most frequent thrombophilic contributors to the development of VTE.Citation40,Citation47,Citation50,Citation51 Although the ophthalmologic literature has primarily focused on the pathophysiologic role that these thrombophilias play in ocular vascular thrombosis,Citation8,Citation16,Citation18,Citation21,Citation22,Citation25,Citation30,Citation36 it has not focused on the likelihood that the ocular thrombotic event is the patient’s first thrombotic event when associated with FVL and/or PTG, directing attention to familial thrombophilias in the kindred and prevention of subsequent thrombi in the proband and family. In the current study, our specific aim was to identify OVOs as first thrombotic events facilitated by FVL and/or PTG heterozygosity and to review the role that these heritable thrombophilias play in subsequent treatment, prophylaxis, and ramifications for patient and kindred.
Methods
The study was approved by the Jewish Hospital Institutional Review Board (ID 12-03). Informed consent was obtained from patients after the nature of the study was fully explained.
After NA-AION, branch or central retinal vein occlusion (BRVO, CRVO), RAO, or amaurosis fugax (AF) was diagnosed, 283 patients (172 with CRVO, 19 BRVO, 32 RAO, 41 AF, and 19 NA-AION) were sequentially referred from 1993 to 2015 by vitreoretinal specialists at the Cincinnati Eye Institute to our outpatient thrombosis research center. The diagnoses were established by complete ophthalmological evaluations during which the patients’ histories, visual deficits, and fundus abnormalities were ascertained and found to be typical of the ischemic events.
Patients with NA-AION exhibited segmental edema of the optic nerve head in eyes with little or no preexisting optic nerve cupping. Eyes with RVOs showed dilation of retinal veins (all veins if a CRVO was present and less than all veins if a BRVO was found) associated with intraretinal hemorrhages, retinal edema, and cotton wool spots limited in area by the drainage bed of the affected veins. Eyes with RAOs demonstrated retinal arterial narrowing, segmentation of the arterial blood column in some cases, and whitening of the retina due to opacification and thickening of the inner retina. In the case of a CRAO, a cherry red spot was seen in the macula. The fundus features of acute OVOs are stereotypical to the degree that confirmatory testing may not be necessary. Fluorescein angiography and optical coherence tomography were performed to corroborate the diagnosis depending on the preference of the referring ophthalmologist. In the cases of AION, measurements of erythrocyte sedimentation rates and C-reactive protein levels helped in the elimination of giant cell arteritis as the cause.
All 92 patients referred with ocular arterial disease (NA-AION, RAO, and AF) underwent carotid ultrasound and cardiac echocardiogram studies, and 18 were not entered into our analysis cohort because of documented arterial emboli. Excepting these 18 excluded arterial cases, the analysis cohort was prospectively evaluated in the sequence of their referral and included 265 cases (163 women and 102 men), 191 with ocular venous occlusion and 74 with ocular arterial occlusion.
The analysis cohort was divided into patients with venous (low-pressure, low-velocity) occlusion, including BRVO and CRVO, and those with arterial (high-pressure and high-velocity) occlusion, including NA-AION, RAO, and AF.
At the patients’ initial visit at our center, a detailed history was taken and physical examination was conducted. In particular, presence of hypertension, diabetes mellitus, and hyperlipidemia; reproductive history and pregnancy outcomes; and previous episodes of VTE, DVT, and/or pulmonary embolism (PE) were noted. In addition, the patients’ use of tobacco or hormonal therapy, as well as family history of thrombosis, was obtained. Lastly, the patients’ visual status was assessed at the time of the ocular event and at each subsequent visit with the retinal specialist.
At the initial visit, atherosclerotic risk factors were measured, serologic coagulation assays were done, and polymerase chain reaction (PCR) analyses for thrombophilia and hypofibrinolysis were performed. Atherosclerotic risk factors measured included age, body mass index, smoking history, blood pressure, hemoglobin A1c, glucose, homocysteine, and levels of triglycerides and cholesterol, including HDL and LDL cholesterol.Citation24
PCR measuresCitation52 were used to measure G1691A factor V Leiden, G20210A prothrombin, methylenetetrahydrofolate reductase (MTHFR) C677T and A1298C mutations, and the plasminogen activator inhibitor-1 4G/4G mutation. In addition, serologic measures of thrombophiliaCitation53 were used, including measurement of anticardiolipin antibodies immunoglobulin G (IgG) and IgM (ACLA IgM), antigenic protein C, total and free protein S, antithrombin III, lupus anticoagulant, factors VIII and XI, and homocysteine. All PCR and serologic measures were done as previously described.Citation24
Healthy normal controls (n=110) were hospital employees, documented by interview and physical examination to be free of acute and chronic disease, including any history or evidence of OVO.
Statistical methods
All statistical analyses were performed using SAS V9.4 (SAS institute Inc, Cary, NC, USA).
Cases were compared to controls by Fisher’s exact test.
Sample size was estimated based on observed data of this report. To detect the difference of 50% having at least one of the seven thrombophilias in cases versus 20% in controls, there should be at least 39 subjects in each group for significance level 0.05 with power 80%.
Results
Central and branch retinal vein occlusion
Of the 191 RVO cases, 172 (90%) had CRVO and 19 (10%) BRVO; there were 116 (61%) women and 75 (39%) men (mean age ± standard deviation [SD]: 57±15 years; median age: 57 years).
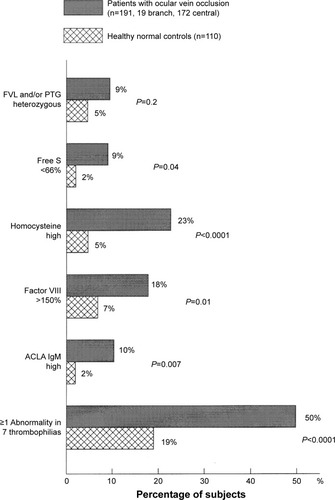
As displayed in , the 191 RVO cases differed from controls in terms of low free protein S (9% vs 2%, respectively; P=0.04), high homocysteine (23% vs 5%, respectively; P<0.0001), high factor VIII (18% vs 7%, respectively; P=0.01), and ACLA IgM (10% vs 2%, respectively; P=0.007). Assessing the number of abnormalities in the seven thrombophilias (FVL, PTG, free protein S, homocysteine, factor VIII, factor XI, and ACLA IgM), 50% of the 191 RVO cases had ≥1 thrombophilic abnormality vs 19% of normal controls (P<0.0001, ). The difference between patients with RVO vs controls in comparing ≥1 abnormality of FVL and PTG mutations was not statistically significant ().
Figure 1 Thrombophilia in 191 patients with ocular vein occlusion (19 branch, 172 central) compared to 110 healthy normal controls without ocular venous or arterial thrombi.
Abbreviations: FVL, factor V Leiden; PTG, prothrombin gene; free S, free protein S; ACLA IgM, anticardiolipin antibody immunoglobulin M.
Retinal artery occlusion
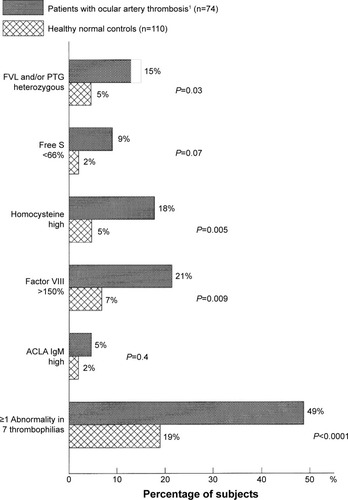
The 74 cases with RAO included 23 with CRAO, 32 AF, and 19 NA-AION, including 47 (64%) women and 27 (36%) men, with mean age ± SD of 54±16 (median: 55 years). As displayed in , the 74 RAO cases differed from controls for ≥1 abnormality of FVL and PTG mutations (15% vs 5%, respectively; P=0.03). They also differed in having high levels of homocysteine (18% vs 5%, respectively; P=0.005) and factor VIII (21% vs 7%, respectively; P=0.009), as well as being marginally different in the low levels of free protein S (9% vs 2%, respectively; P=0.07). Assessing the number of abnormalities in the seven thrombophilias (FVL, PTG, free protein S, homocysteine, factor VIII, factor XI, and ACLA IgM), 49% of the 74 RAO cases had ≥1 thrombophilic abnormality vs 19% of normal controls (P<0.0001).
Figure 2 Thrombophilia in 74 patients with ocular arterial occlusion (23 with central retinal artery occlusion, 32 with amaurosis fugax, and 19 with nonarteritic anterior ischemic optic neuropathy) compared to 110 healthy normal controls without ocular venous or arterial thrombi.
Abbreviations: FVL, factor V Leiden; PTG, prothrombin gene; free S, free protein S; ACLA IgM, anticardiolipin antibody immunoglobulin M.
Taken together, of the 265 patients with OVO (191 venous, 74 arterial), 29 (11%) had mutations of FVL, PTG, or both vs 5 (4.5%) of the 110 healthy normal controls (P=0.07).
FVL or PTG mutations
shows the 29 (11%) cases with heterozygosity of FVL, PTG, or both, among the total cohort of 265 OVO cases. Among these 29 patients with FVL, PTG, or both, the initial ocular vascular occlusive event occurred before the age of 60 years in 18 (62%) cases, before age 50 years in 10 cases (34%), and before age 40 years in 5 cases (17%). The median age at the time of OVO in these 29 cases was 56 years. Of the 16 cases with FVL heterozygosity, nine (56%) were female and seven (44%) were male (mean age ± SD: 51±13 years; median: 52 years).
Table 1 Characteristics of 29 patients with ocular vascular occlusion with FVL or PTG G20210A variant
Fifteen (94%) of the 16 cases with FVL had OVO as their first thrombotic event, defined by no previous DVT or PE, while 1 (6%) had a previous initial thrombotic event (DVT) (). Of the 16 FVL heterozygotes, 6 (38%) experienced other thrombotic events, defined as events likely resulting from a hypercoagulable state other than DVT or PE, including recurrent miscarriages, osteonecrosis, ischemic stroke, and/or ischemic colitis (). Five (31%) of the 16 FVL heterozygotes had an immediate family member with a history of thrombosis, including DVT and/or PE.
At last follow-up visit, 2 (13%) of the 16 cases with FVL had no remaining vision in the affected eye, 6 (38%) had residual vision loss, 5 (31%) returned to baseline vision, and 3 (19%) were lost to follow-up ().
Of the 12 heterozygous PTG cases, 7 (58%) were female and 5 (42%) were male (mean age ± SD: 59±20 years; median: 61 years). Nine (75%) of the 12 cases had OVO as an initial thrombotic event, while 3 (25%) had a known previous thrombotic event (2 DVT, 1 DVT-PE) (). Five (42%) of the 12 cases experienced other thrombotic events, and 6 (50%) had an immediate family member with a history of thrombosis. At their last follow-up visit, four (33%) of the 12 cases heterozygous for PTG had no remaining vision in the affected eye, 6 (50%) had residual vision loss, 1 (8%) returned to baseline vision, and 1 (9%) was lost to follow-up (). One of the 12 PTG heterozygotes (#10) had an additional ocular event (CRVO) in the second eye and returned to baseline vision in that eye at her last follow-up ().
One case was heterozygous for both FVL and PTG mutations. She had BRVO with previous DVT and recurrent miscarriages. She had residual vision loss at last follow-up ().
Of the 29 cases with OVO found to have FVL and/or PTG mutations, 24 (83%) had OVO as a first thrombotic event without prior DVT and/or PE, and 12 (41%) had other thrombotic events including miscarriage, osteonecrosis, ischemic stroke, and/or ischemic colitis. Of these 12 cases with prior thrombotic complications, 10 (83%) were female, 7 (70%) of whom had had previous miscarriages.
Seventeen (59%) of 29 OVO cases with FVL and/or PTG mutation were females (). Of these 17 cases, 7 (41%) had experienced at least one miscarriage for previously unknown reasons, 6 (35%) were on estrogen hormone therapy at the time of the ocular event, and 1 (6%) was on clomiphene. One male patient with PTG heterozygosity (#3, ) developed RVO 3 months after starting testosterone therapy.
Discussion
The ophthalmologist plays a critical role in the disposition and prognosis of patients who present with OVO, particularly when the OVO is the patient’s first thrombotic event. The most frequent pathoetiology for RAO and AF is largely embolic,Citation54,Citation55 which is frequently detectable in branch retinal artery occlusions but often cannot be detected via fundoscopy in ciliary artery occlusions, CRAOs, or AION. The 74 cases with RAO in the current study all had normal carotid and vertebral imaging and normal echocardiography, ruling out overt causes of thromboemboli. There is no easy way to rule out microscopic emboli as a cause of RAO, even when there is no detectable carotid or cardiac abnormality.
While cardioembolic investigation is warranted, there are numerous other contributing etiologies for OVO that must be considered. All patients should have a thorough assessment for cardiovascular and atherosclerotic risk factors, including screening for age, smoking history, hypertension, hyperlipidemia, and diabetes mellitus, all of which have been shown to have a significant, albeit nonspecific and nonsensitive, association with the development of OVO.Citation7,Citation9–Citation23,Citation54–Citation56
Several reports,Citation24,Citation35,Citation57 congruent with our current findings, have demonstrated the significant role of thrombophilia in the development of OVO and emphasize the importance of evaluating for thrombophilia in patients who present with OVO. In the current study, 49% of cases with arterial OVO and 50% with venous OVO had one or more of the seven major thrombophilias vs 19% of 110 healthy normal controls (P<0.0001). In cases of both venous and arterial occlusion, high levels of homocysteine and factor VIII were much more common than in healthy normal controls. Of the multiple thrombophilias, hyperhomocysteinemia has received the most attention as a risk factor for OVO,Citation53 and the relationship between elevated levels of homocysteine and both large-vein thrombosis and OVO is well recognized.Citation5,Citation20,Citation24,Citation32–Citation34,Citation36–Citation39 In addition to hyperhomocysteinemia, genetic mutations of FVL and PTG are major risk factors for large-vein thrombosis.Citation32,Citation40–Citation43 Recent studies have found a high prevalence of FVLCitation21,Citation24,Citation26–Citation28 and PTG mutationsCitation58,Citation59 in patients with OVO versus controls; however, some have not found the same.Citation16,Citation29,Citation30–Citation32
An ophthalmologist is in a unique position to diagnose familial and acquired thrombophilias in patients who present with a new OVO. This remains true even when the patient presents with no personal history of prior thrombosis. In the current study, 24 (83%) of 29 OVO patients found to have FVL and/or PTG mutations had no previous DVT, PE, and/or prior OVO. It is critical to diagnose these underlying, heritable thrombophilias in patients who present with OVO as a first thrombotic event to minimize local and systemic thrombotic morbidity and mortality, including significant vision loss. Approximately 7% of patients with RVO may have a contralateral OVO within 4 years,Citation17 and the risk of visual impairment with OVO is evident in the current study, in which 6 (21%) of 29 cases with FVL and/or PTG heterozygosity had no remaining vision in the affected eye, and 13 (45%) had residual vision loss.
In addition, thrombophilia often causes potentially preventable VTE, DVT, PE,Citation60 ischemic cerebral vascular accidents,Citation61 osteonecrosis,Citation62 and pregnancy loss.Citation63 In our study, 12 (41%) of 29 OVO cases with an underlying FVL and/or PTG mutation had some form of VTE other than DVT and/or PE, such as miscarriage, osteonecrosis, ischemic stroke, and/or ischemic colitis. The risk of systemic thrombosis and OVO is particularly high if the patient is exposed to additional known prothrombotic risk factors, including estrogen or testosterone hormone therapy, pregnancy, surgery, immobilization, or smoking.Citation27,Citation40
Of particular note, 7 (41%) of 17 female patients with FVL and/or PTG heterozygosity presenting with OVO shared a history of at least one unexplained miscarriage. Patients with increased exposure to estrogens, including hormone therapy or pregnancy, in combination with thrombophilia, are at a much higher risk of thrombosis. Six (35%) of 17 females in this study who developed OVO were on estrogen therapy, and 1 (6%) was on clomiphene. Case reports have suggested that clomiphene may predispose individuals to RVO, especially patients with underlying risk factors such as thrombophilia.Citation64 Other studies have shown the miscarriage rate in patients with RVO to be 24%–28%, significantly greater compared to the national figure of 15.7%.Citation24,Citation53,Citation65 These findings illustrate the importance of discovering a thrombophilic state for the patient and family to avoid unnecessary risk exposure, such as hormone therapy, and to allow for close monitoring during high-risk periods, including pregnancy.
Most thrombophilic mutations, including FVL and PTG mutations, are autosomal dominant and highly penetrant. Diagnosing an underlying thrombophilia has important implications, not only for the patient, but for the patient’s family as well. Of the 29 OVO cases in this study with the FVL and/or PTG mutation, 11 (38%) had immediate family members with a history of DVT and/or PE. OVOs serve as a gateway for physicians to discover an undiagnosed heritable thrombophilia, with significant implications for the patient and his or her family including the need for treatment, familial screening, and education regarding the avoidance of additional thrombotic risk factors.
In patients who are young, have an unexpected OVO, and/or have a personal or family history of thrombosis, the physician may discover a hypercoagulable state if appropriately evaluated.Citation20 One study found that up to 84% patients with OVO in which noncoagulation etiologies were ruled out were found to have thrombophilia.Citation9 This finding is of major importance for the patient and the patient’s family to ensure that appropriate medical and lifestyle measures are taken to minimize morbidity and mortality.
While elevated homocysteineCitation53 and antiphospholipid syndromeCitation66 have received the most attention regarding thrombophilias associated with OVO, our study demonstrates the importance of testing for the common and highly prothrombotic familial thrombophilias, FVL and PTG mutations, and illustrates how FVL and PTG heterozygosity may present with OVO as a first thrombotic event. It is important for the ophthalmologist to diagnose underlying coagulation disorders as both an etiology for OVO and as a window to family screening and preventive therapy for the family and the proband.
Acknowledgments
This work was supported in part by the Lipoprotein Research Fund of the Jewish Hospital of Cincinnati.
Disclosure
The authors report no conflicts of interest in this work.
References
- CugatiSWangJJRochtchinaEMitchellPTen-year incidence of retinal vein occlusion in an older population: the Blue Mountains Eye StudyArch Ophthalmol200612472673216682596
- DavidRZangwillLBadarnaMYassurYEpidemiology of retinal vein occlusion and its association with glaucoma and increased intraocular pressureOphthalmologica198819769743186211
- KleinRMossSEMeuerSMKleinBEThe 15-year cumulative incidence of retinal vein occlusion: the Beaver Dam Eye StudyArch Ophthalmol200812651351818413521
- RogersSMcIntoshRLCheungNInternational Eye Disease ConsortiumThe prevalence of retinal vein occlusion: pooled data from population studies from the United States, Europe, Asia, and AustraliaOphthalmology201011731331920022117
- JohnsonLNArnoldACIncidence of nonarteritic and arteritic ischemic optic neuropathy: population-based study in the state of Missouri and Los Angeles County, CaliforniaJ Neuroophthalmol19941438448032479
- VarmaDDCugatiSLeeAWChenCSA review of central retinal artery occlusion: clinical presentation and managementEye20132768869723470793
- KariaNRetinal vein occlusion: pathophysiology and treatment optionsClin Ophthalmol2010480981620689798
- RehakMWiedemannPRetinal vein thrombosis: pathogenesis and managementJ Thromb Haemost201081886189420492457
- BickRLAlfarHGoedeckeCThrombophilic causes of retinal vascular thrombosis: etiology and treatment outcomesClin Appl Thromb Hemost2002831531812516681
- BeaumontPEKangHKClinical characteristics of retinal venous occlusions occuring at different sitesBr J Ophthalmol20028657258011973257
- HitchingsRASpaethGLChronic retinal vein occlusion in glaucomaBr J Ophthalmol1976606946991009041
- DrydenRMCentral retinal vein occlusions and chronic simple glaucomaArch Ophthalmol19657365966314281983
- Group EDC-CSRisk factors for central retinal vein occlusionArch Ophthalmol19961145455548619763
- MohamedQMcIntoshRLSawSMWongTYInterventions for central retinal vein occlusion: an evidence-based systematic reviewOphthalmology200711450751917324695
- StemMSTalwarNComerGMSteinJDA longitudinal analysis of risk factors associated with central retinal vein occlusionOphthalmology201312036237023177364
- WegerMRennerWPinterORole of factor V Leiden and prothrombin 20210A in patients with retinal artery occlusionEye (Lond)20031773173412928685
- HayrehSSZimmermanBMcCarthyMJPodhajskyPSystemic diseases associated with various types of retinal vein occlusionAm J Ophthalmol2001131617711162981
- PriscoDMarcucciRBertiniLGoriAMCardiovascular and thrombophilic risk factors for central retinal vein occlusionEur J Intern Med20021316316912020623
- RecchiaFMBrownGCSystemic disorders associated with retinal vascular occlusionCurr Opin Ophthalmol20001146246711141642
- BackhouseOParapiaLMahomedILeeDFamilial thrombophilia and retinal vein occlusionEye (Lond)200014131710755093
- RehakMRehakJMüllerMThe prevalence of activated protein C (APC) resistance and factor V Leiden is significantly higher in patients with retinal vein occlusion without general risk factorsThromb Haemost20089992592918449423
- CheungNKleinRWangJJTraditional and novel cardiovascular risk factors for retinal vein occlusion: the multiethnic study of atherosclerosisInvest Ophthalmol Vis Sci2008494297430218539932
- O’MahoneyPWongTRayJRetinal vein occlusion and traditional risk factors for atherosclerosisArch Ophthalmol200812669269918474782
- GlueckCJWangPHutchinsRPetersenMRGolnikKOcular vascular thrombotic events: central retinal vein and central retinal artery occlusionsClin Appl Thromb Hemost20081428629418160589
- YauJWLeePWongTYBestJJenkinsARetinal vein occlusion: an approach to diagnosis, systemic risk factors and managementIntern Med J20083890491019120547
- WilliamsonTHRumleyALoweGDBlood viscosity, coagulation, and activated protein C resistance in central retinal vein occlusion: a population controlled studyBr J Ophthalmol1996802032088703856
- LarssonJOlafsdottirEBauerBActivated protein C resistance in young adults with central retinal vein occlusionBr J Ophthalmol1996802002028703855
- Ben-AmiRZeltserDLeibowitzIBerlinerSARetinal artery occlusion in a patient with factor V Leiden and prothrombin G20210A mutationsBlood Coagul Fibrinolysis200213575911994569
- ArasSYilmazGAlpasIBaltaciVTayançEAydinPRetinal vein occlusion and factor V Leiden and prothrombin 20210 G: A mutationsEur J Ophthalmol20011135135511820306
- DemirciFYGüneyDBAkarçayKPrevalence of factor V Leiden in patients with retinal vein occlusionActa Ophthalmol Scand19997763163310634553
- LarssonJHillarpAThe prothrombin gene G20210A mutation and the platelet glycopprotein IIIa polymorphism PIA2 in patients with central retinal vein occlusionThromb Res19999632332710593436
- JanssenMCHden HeijerMCruysbergJRMWollersheimHBredieSJHRetinal vein occlusion: a form of venous thrombosis or a complication of atherosclerosis?J Thromb Haemost20059310211026
- FeganCDCentral retinal vein occlusion and thrombophiliaEye (Lond)2002169810611913903
- TurelloMPascaSDaminatoRRetinal vein occlusion: evaluation of “classic” and “emerging” risk factors and treatmentJ Thromb Thrombolysis20102945946419669864
- SottilottaGOrianaVLatellaCRole of hyperhomocystinemia in retinal vascular occlusive diseaseClin Appl Thromb Hemost20071310410717164500
- CahillMTStinnettSSFekratSMeta-analysis of plasma homocysteine, serum folate, serum vitamin B(12), and thermolabile MTHFR genotype as risk factors for retinal vascular occlusive diseaseAm J Ophthalmol20031361136115014644226
- BiousseVNewmanNJSternbergPJRetinal vein occlusion and transient monocular visual loss associated with hyperhomocystinemiaAm J Ophthalmol19971242572609262559
- McCullyKSHomocysteine and vascular diseaseNat Med199623863898597939
- WaldDSLawMMorrisJKHomocysteine and cardiovascular disease: evidence on causality from a meta-analysisBMJ2002325120212446535
- SimsekEYesilyurtAPinarliFEyerciNUlusATCombined genetic mutations have remarkable effect on deep venous thrombosis and/or pulmonary embolism occurenceGene201353617117624334115
- SeligsohnULubetskyAGenetic susceptibility to venous thrombosisN Engl J Med20013441222123111309638
- PoortSRRosendaalFRReitsmaPHBertinaRMA common genetic variation in the 3′-untranslated region of the prothrombin gene is associated with elevated plasma prothrombin levels and an increase in venous thrombosisBlood199688369837038916933
- KosterTRosendaalFRde RondeHBriëtEVandenbrouckeJPBertinaRMVenous thrombosis due to poor anticoagulant response to activated protein C: Leiden Thrombophilia StudyLancet1993342150315067902898
- BertinaRMKoelemanBPKosterTMutation in blood coagulation factor V associated with resistance to activated protein CNature199436964678164741
- RidkerPMMiletichJPHennekensCHBuringJEEthnic distribution of factor V Leiden in 4047 men and women. Implications for venous thromboembolism screeningJAMA1997277130513079109469
- RosendaalFRDoggenCJZivelinAGeographic distribution of the 20210 G to A prothrombin variantThromb Haemost1998797067089569177
- ZhouXQianWLiJWho are at risk for thromboembolism after arthroplasty? A systematic review and meta-analysisThromb Res201313253153624074702
- TugEAydinHKaplanEDogruerDFrequency of genetic mutations associated with thromboembolism in the Western Black Sea RegionIntern Med201150172121212568
- GlueckCJWangPOcular vascular thrombotic events: a diagnostic window to familial thrombophilia (compound factor V Leiden and prothrombin gene heterozygosity) and thrombosisClin Appl Thromb Hemost200915121818796459
- WeingarzLSchwonbergJSchindewolfMPrevalence of thrombophilia according to age at the first manifestation of venous thromboembolism: results from the MAISTHRO registryBr J Haematol201316365566524219332
- de JongPGGoddijnMMiddeldorpSTesting for inherited thrombophilia in recurrent miscarriageSemin Reprod Med20112954054722161466
- GlueckCJFreibergRAWangPHeritable thrombophilia-hypofibrinolysis and osteonecrosis of the femoral headClin Orthop Relat Res20084661034104018350351
- GlueckCJHutchinsRKJuranteeJKhanZWangPThrombophilia and retinal vascular occlusionClin Ophthalmol201261377138422969282
- SharmaSNaqviASharmaSMCruessAFBrownGCTransthoracic echocardiographic findings in patients with acute retinal arterial obstruction. A retrospective review. Retinal Emboli of Cardiac Origin GroupArch Ophthalmol1996114118911928859076
- SharmaSThe systemic evaluation of acute retinal artery occlusionCurr Opin Ophthalmol199891510182093
- SalomonOHuna-BaronRMoisseievJThrombophilia as a cause for central and branch retinal artery occlusion in patients without an apparent embolic sourceEye (Lond)20011551151411767028
- GreinerKHafnerGDickBPeetzDPrellwitzWPfeifferNRetinal vascular occlusion and deficiencies in the protein C pathwayAm J Ophthalmol1999128697410482096
- KapurRKMillsLASpitzerSGHultinMBA prothrombin gene mutation is significantly associated with venous thrombosisArterioscler Thromb Vasc Biol199717287528799409269
- GurgeyAHaznedarogluICEgeselTTwo common genetic thrombotic risk factors: factor V Leiden and prothrombin G20210A in adult Turkish patients with thrombosisAm J Hematol20016710711111343382
- RodeghieroFTosettoAActivated protein C resistance and factor V Leiden mutation are independent risk factors for venous thromboembolismAnn Intern Med199913064365010215560
- GlueckCJFontaineRNWangPInteraction of heritable and estrogen-induced thrombophilia: possible etiologies for ischemic optic neuropathy and ischemic strokeThromb Haemost20018525625911246543
- GlueckCJFreibergRAFontaineRNSieve-SmithLWangPAnticoagulant therapy for osteonecrosis associated with heritable hypofibrinolysis and thrombophiliaExpert Opin Investig Drugs20011013091316
- GlueckCJPranikoffJAregawiDThe factor V Leiden mutation, high factor VIII, and high plasminogen activator inhibitor activity: etiologies for sporadic miscarriageMetabolism2005541345134916154434
- ViolaMIMeyerDKrugerTAssociation between clomiphene citrate and visual disturbances with special emphasis on central retinal vein occlusion: a reviewGynecol Obstet Invest201071737621160153
- VenturaSJMosherWDCurtinSCAbmaJCHenshawSTrends in pregnancies and pregnancy rates by outcome: estimates for the United States, 1976–1996Vital Health Stat 2120002114710740440
- YangPKruhJNFosterCSAntiphospholipid antibody syndromeCurr Opin Ophthalmol20122352853223042148
