?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Purpose
To determine the prevalence of presbyopia, and near vision spectacle coverage in a rural population of Northwestern Nigeria.
Study design
Cross sectional prevalence study.
Subjects and methods
Six hundred and fifty people of at least 40 years of age, in 13 clusters (50 per cluster) were examined using a multi-stage random sampling with probability proportional to size. The survey was conducted from April 7 to 28, 2012 at Bungudu Local Government Area of Zamfara State, Nigeria. Presbyopia was defined as the inability to read N8 at 40 cm. Presbyopic Spectacle Correction Coverage (PSCC) was calculated, and information on barriers to using near vision spectacles identified.
Results
The crude prevalence of presbyopia was 30.4%, 95% CI: (26.8%–34.1%). The prevalence was significantly higher in females (P=0.0005) and individuals with at least secondary education (P=0.022). The age specific prevalence of presbyopia was three times (63.5%) more among those aged 70 years and above, as compared to those within 40–49 years age group (19.3%). The met need was 0.2%, the unmet need 30.2%, and a PSCC of 0.7%. The major barriers reported as reasons for not obtaining near vision spectacles were unawareness and lack of felt need.
Conclusion
The prevalence of presbyopia in Bungudu is relatively low compared to other reports with major risk factors being increasing age, female sex and attainment of higher education. The presbyopic spectacles correction coverage is very low with high unmet need thus there is a need to create awareness, and provide affordable and accessible optical services in the affected population.
Keywords:
Introduction
Presbyopia is an inability to focus at near distance as a result of loss of accommodation with age.Citation1
With age, presbyopia eventually affects everyone but is generally measured and diagnosed only when an individual becomes symptomatic and presents to an eye care provider with need for near-vision correction. In clinical practice, presbyopia is diagnosed by measurements of accommodative amplitude, near subjective refraction, and/or patient’s reported symptoms.Citation2
While new treatments are being developed for presbyopia, spectacles represent an effective, economic option for low- and middle-income countries.Citation3 Use of contact and accommodative intraocular lenses have the advantage of making presbyopes spectacle independent. Lenticular and corneal surgical manipulations have been reported to alleviate presbyopia; these include multifocal and monovision corneal refractive surgical procedures, or near-vision conductive keratoplasty, or a pinhole (PH) corneal inlay.Citation4 These devices and surgical procedures are however not accessible to our study population.
It is now increasingly recognized that presbyopia is an aspect of refractive error that needs to be addressed. Good vision is important, even among populations who use it for tasks other than reading and writing.Citation3
Holden et alCitation5 estimated in 2005 that 1.04 billion people worldwide were presbyopic with an expected increase to 1.4 billion and 1.8 billion by the years 2020 and 2050, respectively. They deduced the prevalence in North America, Europe, and Japan to be 83% among individuals 45 years and above. Population-based studies in East Africa reported prevalence of 61.7%–85.4%,Citation6,Citation7 with low spectacle coverage in individuals aged 40 years and older.
Few population-based studiesCitation8–Citation10 carried out in Nigeria reported presbyopia prevalence of 33%–53.5%; majority of reported studies being institution-based.Citation11–Citation14
Zamfara state located in Northwestern Nigeria has had a VISION 2020: the Right to Sight-compliant eye care program since 2009 that provides eye care services including optical services. Although implemented through the primary health care structure, optical services are largely restricted to major towns where skilled workers are available to provide the service. The purpose of this study was to provide data on presbyopia and spectacle correction coverage and barriers that could serve as baseline data for stakeholders of the Zamfara state eye care program and nearby states. The data could be used for advocacy, planning, and resource allocation to achieve a more efficient and effective optical service delivery.
Subjects and methods
Study design
This was a population-based survey of people 40 years and above conducted from April 7 to 28, 2012.
Ethical considerations
Human Research and Ethics Committee of the National Eye Centre in Nigeria granted ethical approval. Bungudu Local Government Area (LGA) and Zamfara State Ministry of Health also gave approval for conducting the study.
Sample size determination
A minimum sample size of 646 people was calculated using the formula:
(1) where n= required sample size, Z= standard normal deviation, p= expected prevalence, q= (1–p), d= degree of accuracy and multiplied by the design effect.
(2)
Study Population
Bungudu LGA is one of the 14 LGAs in Zamfara State with 2,356 km2 land mass. The local government headquarters is about 20 km from Gusau, the state capital. It is located at 12°16′00″N 6°33′24″E. It has a population of 257,917 with 20% aged 40 years and above who are mainly agrarian Hausas, Fulanis, and a few other minority ethnic groups of Nigeria. The LGA has eleven administrative wards with one general hospital and 57 primary health centers. There is no eye clinic in any of the health facilities in the LGA. The nearest eye care facility is located 20 km away in the state capital. In 2011, the State Eye Care Programme trained ten community health extension workers as integrated eye care workers who are spread across the health facilities.
Inclusion criteria
1) Individuals 40 years and above. 2) Resident who has spent at least 6 months in the community continuously.
Exclusion criteria
1) Person(s) whose presenting distance visual acuity (VA) is less than 6/60 of Snellen chart and did not improve with PH. 2) Individuals with mental or other incapacitating illnesses whose vision cannot be tested.
Sampling technique
Using a cluster size of 50 people, 13 (650/50) clusters were selected using a multi-stage random sampling with probability proportional to size. In each cluster, sample selection was by “spin-the-bottle method” at the center of the cluster that was followed by random walk to select households for inclusion into the study. All eligible people in a household were included in the survey until the required sample size in a cluster was obtained.
Survey team and training
The survey team comprised of an ophthalmologist (principal investigator [PI]), an ophthalmic nurse (ON) and a research assistant (interviewer). A pilot survey was conducted in a non-selected community in the LGA. The VA measurement achieved an inter-observer agreement of more than 90% between the ON and the PI. The purpose of the interview was masked to the research assistant (interviewer) to reduce bias and an agreement of more than 90% was obtained with the PI on how to administer the questionnaire. Areas of difficulty were re-discussed and further practiced to minimize errors in data collection. The International Center for Eye Health of the London School of Hygiene and Tropical Medicine validated the survey questionnaire as used in an earlier study in Nigeria.Citation9
Data collection procedures
The trained interviewer obtained enumeration and demographic information comprising of age, sex, occupation, and educational level after obtaining consent. Historical events were used to estimate age where necessary.
The ON assessed the distance VA of subjects using the Snellen tumbling E chart at six meters in ambient outdoor illumination under shade. PH VA was done on all subjects who had VA less than 6/18 in either eye. Refractive error was defined as improvement of vision to 6/18 or better with PH in either eye.
The ophthalmologist then carried out objective and subjective distance refraction for subjects presenting with VA less than 6/18 who had an improvement of at least one Snellen acuity line with a PH in either eye.
Near vision was tested at 40 cm (wearing distance correction where necessary) using logMAR (logarithm of the minimum angle of resolution) near E chart under ambient indoor illumination. Correct identification of three out of five characters constituted success in reading a line. The end point of near vision testing was N8 optotypes. Presbyopia (functional) was defined in a subject who could not read the N8 optotype at 40 cm with the distance correction in place, if required. Under-corrected presbyopia is said to be present in a subject presenting with near vision spectacles but who fails to read N8.
Spectacles for near correction were provided at no cost to the presbyopes (uncorrected or under-corrected), subject to availability of the required power and willingness of participants to accept. This was done after completion of data collection in an entire cluster without prior knowledge of the participants to avoid bias. Subjects whose near spectacle prescription was not available or had other ocular pathologies were referred to the eye clinic for appropriate management.
Participants with presbyopia who do not present with near vision spectacle correction were asked to state reason(s) for not having a presbyopic spectacle correction.
Data management
Collected data were entered into a software program designed in SPSS for windows version 16.0 (SPSS Inc., Chicago, IL, USA) and analyzed with support from a statistician. The prevalence, confidence intervals and P-values (significant at the P<0.05 level), percentages of met need, unmet need, and presbyopia spectacles correction coverage (PSCC) were calculated. Analysis of variance (ANOVA) was used to determine the association between age, sex, and literacy with near visual impairment. “Met need” was calculated as the number of presbyopic subjects who are able to read N8 with presenting near vision spectacles out of the total people examined. “Unmet need” was the number of presbyopic people without near vision spectacles or unable to read N8 with spectacles (where available) out of the total people examined. PSCC was calculated using the formula:
(3)
Results
General characteristics
Of the 650 subjects enumerated, 635 were examined constituting a response rate of 97.7%. The mean age of participants was 53.59 years (range 40–97 years). As shown in , there was no significant age differences among people examined and those not examined (refused and absent), (P=0.448). The baseline characteristics of subjects examined are depicted in .
Table 1 Baseline characteristics of sample population with age distribution of presbyopia
Table 2 Baseline characteristics of study subjects
The number of males and females and their proportions within the age groups was significantly different (P=0.000). Majority (42.4%) of the sample was 40–49 years of age. Majority of the participants had Qur’anic education and only 4.1% attained tertiary education ().
Table 3 Distribution of presbyopia by literacy level
Out of all the females examined only 3.2% (8/249) had formal education. Farming was the major occupation among the males (48.5%) while the majority of the females were housewives.
Prevalence of presbyopia
The crude prevalence of presbyopia was 30.4%, (95% confidence interval: 26.8%–34.1%). The mean dioptric add required to read N8 increased significantly with age (P=0.000).
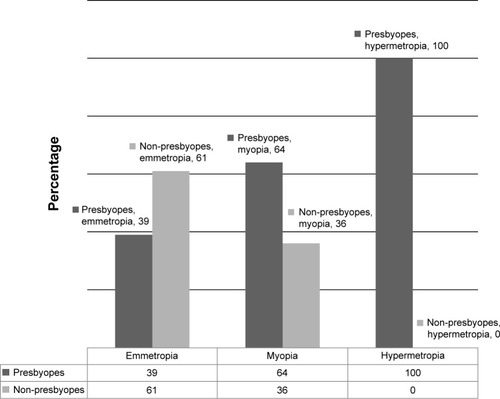
The prevalence of presbyopia was two times higher in females (P=0.000). The prevalence of presbyopia is higher among hyperopes (100%) than myopes (64%) and emmetropes (39%) (). There is a weak association of presbyopia with educational status as people with at least secondary education were more likely to be presbyopic (P=0.022).
PSCC, met, and unmet needs
Only six people with presbyopia presented with near vision correction spectacles, and five could not read N8 at 40 cm with their current spectacles. The met need was 0.2% (1/635×100), unmet need of 30.2% (192/635×100) and a PSCC of 0.7% (met need/met need + unmet need). There was no statistically significant difference among participants in terms of their age group, sex, literacy level, and occupation in use of near vision spectacle correction. The near vision spectacles were obtained by three participants from the roadside spectacle vendors while the rest were from an eye clinic.
Barriers to use of near vision spectacles
The major barriers to obtaining near vision spectacles were “not aware of problems”, “no felt need”, “not a priority”, and “lack of money” ().
Table 4 Barriers to use of near vision spectacles
Women significantly reported lack of awareness as a barrier to obtaining near vision spectacles compared with men (P=0.002). Other demographic characteristics such as age group, literacy level, and occupation of the participants did not show any statistically significant difference in the barriers reported. Of the six participants who have had near vision spectacles, four bought it for less than N2000.00 (US$12) while two bought theirs for between N2,000.00 (US$12) and N3,999.00 (US$24). All of them said they could pay a maximum of the same amount for replacement.
Discussion
This study had a good response rate that was achieved through adequate community mobilization. The results of this study could be a reflection of presbyopia in the district and possibly nearby population. The results obtained in this study will help in the ongoing implementation of Zamfara State Eye Care Programme which hitherto had no baseline data on presbyopia in the state.
The mean age of participants in this study is similar to a study conducted in Abuja, Nigeria.Citation9 Out of the 15 people who were absent during examination or refused, 13 (86%) were females. The refusal rate was higher in women because their male spouses did not give consent for examination. The literacy level of participants was low which is at variance with the Abuja and Southeastern Nigeria studies.Citation8,Citation9 Only 12% of the people examined had at least secondary education which was far lower than the average of 41.4%Citation16 for the Zamfara state central senatorial district to which LGA study belongs.
The prevalence of 30.4% obtained in this study translates to a magnitude of between 13,824 and 17,590 people 40 years and above with presbyopia in Bungudu LGA. This is similar to that reported from studies in Southeast Nigeria (33%)Citation8 and Timor-Leste (32.3%).Citation15 The Timor-Leste study was similar to ours as they were both conducted in people 40 years and above unlike the Nigerian study that included younger people. Studies in NigeriaCitation8 and other African countriesCitation6,Citation7 reported prevalence higher than 50%. The variation may be due to significantly lower number of female participants who are known to have higher prevalence of presbyopia.Citation6,Citation7,Citation9 A male female ratio of 1:1.7 was obtained in this study suggesting the need to give priority to females in eye care services aimed at improving near vision. The low literacy level might have contributed to low prevalence, as higher prevalence has been associated with high literacy level.Citation7,Citation9 Majority of the people who attained secondary education in this study are presbyopic which may be related with higher visual demand for near tasks such as reading.
The mean dioptric power required to read N8 at 40 cm increases with age among participants in this study, which corroborates results from several other studies.Citation6,Citation7,Citation15 This is due to decline in amplitude of accommodation with increasing age.Citation1,Citation17 All participants with hypermetropia were presbyopic compared to those with myopia and emmetropia. Hypermetropia is known to be associated with early onset presbyopia. However, residual hypermetropia not fully corrected may induce pseudo-presbyopia.
PSCC, met, and unmet needs
The PSCC, met and unmet needs obtained in this study are very low compared to results from similar studies in NigeriaCitation9 and other developing countries.Citation6,Citation15 The NigerianCitation9 study reported a PSCC, met need and unmet need of 21%, 11.2%, and 42.1%, respectively. The low literacy level in this study population may have contributed to the low PSCC of 0.7%. A global survey showed that educated individuals are more likely to have eye examinations in their lifetime.Citation18 An Indian study reported that the odds of seeking ophthalmic treatment were significantly higher among literate individuals.Citation19 Only one (16.7%) out of six participants who presented with near vision spectacles read N8 at 40 cm, thus giving 83% under-corrected presbyopia. The absence of an eye clinic in the LGA and unfelt need for near vision spectacles might have accounted for this. Sex, literacy level, and occupation did not influence ownership of near vision spectacles in our study. There have been reports of high PSCC among malesCitation15 and people with higher education.Citation8 Majority of the participants in this study read the Holy Qur’an, usually written in large Arabic script. This may delay the need for reading spectacles. Health education training and integration of nurses and community health extension workers as refractionists, primary eye care workers, and redeploying them to rural areas will increase access to optical services thereby raising the PSCC. Incorporation of refraction services into the cataract outreach program may also enhance presbyopic spectacle correction uptake especially among women and the elderly who have high prevalence of presbyopia.
The major reasons given by participants for not owning near vision spectacles were “lack of awareness” and, “unfelt need”, lack of priority which compares with findings in studies from resource poor nations.Citation7,Citation8,Citation20 This similarity may be due to common prevailing socio-economic conditions in the developing countries. None of the six participants with presbyopia who presented with spectacles interviewed in this study was willing to pay more than N4,000.00 (US$24) for near vision spectacles. Provision of affordable and accessible optical services may enhance spectacle utilization in Bungudu LGA.
Of the six people who use spectacles in this study, three purchased it from roadside vendors. Ayanniyi et alCitation21 reported that 16 (7%) out of 214 spectacle wearers interviewed in six health centers in Ilorin and Ekiti states obtained them from roadside vendors. This attitude should be discouraged through health education, because incorrectly prescribed glasses may act as a barrier to continuous use of spectacles if discomfort and poor vision persist. There is the need for provision of an affordable and accessible optical service to optimize spectacle correction uptake and improve quality of life. However, the fact that lack of felt need was the commonest barrier reported in this study means unless the people are health educated on the benefit of using near spectacles, utilization of the latter may remain low.
The onset of presbyopia influences near work habits of individuals and as such no uniform method can accurately detect it among different people. In this study the inability to read N8 at 40 cm with logMAR near chart may have under-diagnosed participants with presbyopia whose habitual near work distance is less than 40 cm. There is therefore a need for the stakeholders to develop short- and long-term plans to provide optical services to the population. The short-term strategy should create demand using radio and television jingles and also utilize available ONs in the state capital as refractionists diagnosing and dispensing spectacles for simple refractive errors including presbyopia using outreach service delivery strategy; and a long-term plan should be the establishment of an eye clinic in the local government area providing regular comprehensive eye care services including optical services.
Conclusion
The PSCC is very low in the study district and impliedly in Zamfara state, Nigeria with high unmet need.
Acknowledgments
We thank the management of National Eye Centre, Kaduna, Nigeria for partial funding, members of the survey team for the sacrifices during the conduct of the survey, and Prof CO Bekibele for his immense contribution and support during the conduct of this work that was submitted to the National Postgraduate Medical College of Nigeria as dissertation for the award of the Fellowship of the College.
Disclosure
The authors have no conflicts of interest to disclose.
References
- GlasserAKaufmanPLAccommodation and presbyopiaKaufmanPLAlmAAdler’s physiology of the Eye, clinical application10th edPhiladelphiaMosby2003197233
- HickenbothamARoordaASteinmausCGlasserAMeta-Analysis of Sex Differences in PresbyopiaInvest Ophthalmol Vis Sci20125363215322022531698
- PatelIWestSKPresbyopia: prevalence, impact and interventionsCommunity Eye Health20072063404117971909
- BaikoffGSurgical treatment of presbyopia: scleral, corneal, and lenticularCurr Opin Ophthalmol200415436536915232478
- HoldenBAFrickeTRHoSMGlobal Vision Impairment due to Uncorrected PresbyopiaArch Ophthalmol2008126121731173919064856
- SherwinJCKeeffeJEKuperHIslamFMMullerAMathengeWFunctional presbyopia in a rural Kenyan population: the unmet presbyopic needClin Experiment Ophthalmol200836324525118412593
- BurkeAGPatelIBeatrizMPopulation-based study of presbyopia in rural TanzaniaOphthalmology2006113572372716650664
- NwosuSNOcular problems of young adults in rural NigeriaInt Ophthalmol199822525926310826540
- ChiromaMRPrevalence of presbyopia and the impact of uncorrected presbyopia on the quality of life in rural Gwagwalada, Abuja, Nigeria dissertationInternational Center for Eye Health (ICEH): London School of Hygiene and Tropical Medicine (LSHTM)2008
- KioFEOstia-EminaMPattern of refractive anomalies in Warri metropolis, Delta State of NigeriaJournal of the Nigerian Optometric Association2003103038
- AshayeAOAsuzuMCOcular findings seen among the staff of an institution in Lagos NigeriaWest Afr J Med2005242969916092306
- BagaiyaTPamVRefractive error in Kaduna, NigeriaThe Nigerian Journal of Surgical Research200353–4106109
- AmadiANNwankwoBOIbeAICommon ocular problems in Aba metropolis of Abia State, Eastern NigeriaPakistan Journal of Social Sciences2009613233
- EkwenchiEEEzegwuiIUmehRPattern of Eye disorders among inmates of a Nigerian PrisonOrient Journal of Medicine2009214 Available from: www.ajol.info.journalhome
- RamkeJToitRDPalagyiABrianGNaduvilathTCorrection of refractive error and presbyopia in Timor-LesteBr J Ophthalmol200791786086617576709
- National Bureau of Statistics Nigeria [homepage on the Internet]Report of the National Literacy Survey 2010 Available from: nigerianstat.gov.ng/pages/download/4Accessed March 10, 2013
- ElkingtonARFrankHJGreaneyMJPresbyopiaElkingtonARFrankHJGreaneyMJClinical Optics3rd edLondonWiley-Blackwell1999141151
- VelaCSamsonEZunzuneguiMVHaddadSAubinMJFreemaEEEye care utilization by older adults in low, middle, and high income countriesBMC Ophthalmol201212522471351
- KovaiVKrishnaiahSShamannaBRThomasRRaoGNBarriers to accessing eye care services among visually impaired populations in rural Andhra Pradesh, South IndiaIndian J Ophthalmol200755536537117699946
- LaviersHThe prevalence of presbyopia and feasibility of community distribution of near spectacles in adults in Zanzibar, East AfricaJ Community Eye Health2007206473
- AyanniyiAAFadamiroCOAdeyemiFolorunsoFNUzukwuSCCommon refractive errors among the Ekitis of southwesternJournal of Medicine and Medical Sciences201019401416