Abstract
Rhino–orbital–cerebral mucormycosis (ROCM) is an uncommon but fatal fungal infection. We report a rare case of unilateral ROCM with ipsilateral central retinal artery occlusion and contralateral choroiditis, which later progressed to endogenous fungal endophthalmitis. The patient was successfully treated with sinuses debridement, systemic liposomal amphotericin B, and intravitreal amphotericin B. The endophthalmitis completely resolved with good vision, but the ROCM eye remained blind due to central retinal artery occlusion.
Introduction
Mucormycosis is a rare opportunistic infection caused by filamentous fungi of the family Mucoraceae. These fungi are commonly found in soil, decaying vegetation, animal feces, and old bread.Citation1 There are six major clinical forms of mucormycosis – namely, rhino–orbital–cerebral mucormycosis (ROCM), pulmonary mucormycosis, cutaneous mucormycosis, gastrointestinal mucormycosis, disseminated mucormycosis, and uncommon forms such as endocarditis, osteomyelitis, peritonitis, and pyelonephritis.Citation2 ROCM is the most common form of mucormycosis in diabetic patients, and it is the presenting manifestation in one-fourth of diabetic patients who present with ROCM.Citation3,Citation4 The prevalence of ROCM in diabetic patients is 0.15%.Citation4 ROCM usually occurs in debilitated hosts and is frequently fatal. We report a case of unilateral ROCM with ipsilateral central retinal artery occlusion (CRAO), cavernous sinus thrombosis, and contralateral endogenous fungal endophthalmitis in a diabetic patient.
Case report
A 63-year-old woman with no background medical history presented with a 1-day history of sudden drooping of the right eyelid and loss of right eye vision upon waking from sleep. It was associated with intermittent fever and headache for 10 days. She had a history of right upper premolar tooth extraction 2 weeks before the onset of symptoms.
She was conscious, oriented, and afebrile. There were no signs of meningeal irritation. Her oral hygiene was good and there was no foul-smelling nasal discharge. Ophthalmic examination revealed periorbital cellulitis, complete ptosis, and total ophthalmoplegia of the right eye. No proptosis was observed. She had right infraorbital hypoesthesia.
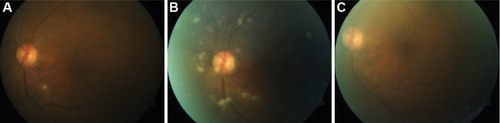
The visual acuity in the right eye included no perception of light, with the presence of relative afferent pupillary defect in the affected eye. Anterior segment examination was unremarkable in both eyes. Fundoscopy revealed a slightly pale optic disc, a generalized pale retina, and the presence of a cherry red spot at the posterior pole, suggestive of CRAO of the right eye ().
Figure 1 Fundus photo of the right eye showed a slightly pale optic disc, a generalized pale retina, and the presence of a cherry red spot at the posterior pole.

The visual acuity in the fellow eye was 6/24 correctable to 6/18 with a pinhole. The extraocular movement was full in the left eye. Fundoscopy of the left eye showed a white creamy subretinal nodule at the inferior arcade close to the optic disc, suggesting choroiditis; however, no vitritis was observed ().
Figure 2 Fundus photo of the left eye.
Abbreviations: D-AMB, amphotericin B deoxycholate; AMB, amphotericin B; L-AMB, liposomal amphotericin B.
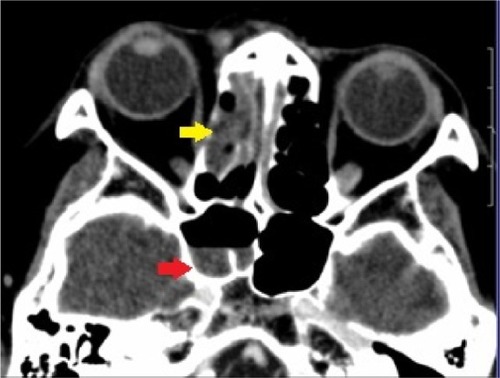
Her random blood sugar level was 23.0 mmol/L, her urine glucose was 4+ (110 mmol/L), but her urine ketone was negative. Hemogram revealed leukocytosis (17.24×10−3/μL); blood culture was negative. Computed tomography scan of the brain, orbit, and paranasal sinuses showed mucosal thickening and fluid in the right ethmoidal and sphenoidal sinuses compatible with sinusitis (). Nasal and sinus endoscopy by the otorhinolaryngology team showed black eschar in the right sinuses (). A biopsy was taken from the necrotic tissue for microbiological examination. Further cranial imaging with magnetic resonance imaging, magnetic resonance arteriogram, and venogram showed evidence of right cavernous sinus thrombosis.
Figure 3 Contrast-enhanced computed tomography of the brain, orbit, and paranasal sinuses.
Based on the clinical and radiological findings, she was diagnosed with right ROCM with ipsilateral CRAO and cavernous sinus thrombosis, as well as choroiditis in the left eye. She was also diagnosed with diabetes mellitus. She was started on intravenous amphotericin B deoxycholate (D-AMB), 50 mg daily, and her blood sugar was controlled with subcutaneous insulin. She underwent emergency functional endoscopic sinus surgery with debridement of the sinuses. Culture of the biopsy specimen from the sinuses grew Rhizopus spp.
At 3 weeks of treatment, the choroiditis in the left eye progressed to endogenous fungal endophthalmitis with multifocal chorioretinitis and overlying minimal vitritis (). Vitreous tap and single-administration intravitreal amphotericin B (AMB), 0.005 mg, diluted with sterile water to 0.1 mL was injected into the left eye. At the same time, she developed nephropathy secondary to intravenous D-AMB treatment. Her treatment was then changed to liposomal amphotericin B (L-AMB), 250 mg daily.
She was discharged well after 10 weeks of hospitalization and had completed intravenous L-AMB for a total duration of 7 weeks. Subsequent follow-up revealed that her right eye remained blind, with complete ptosis and total ophthalmoplegia. There was complete resolution of chorioretinitis and vitritis in the left eye (), with a final best-corrected visual acuity of 6/9.
Discussion
CRAO and endophthalmitis are rare complications of ROCM with few published reports.Citation4,Citation5 Ipsilateral endophthalmitis to the ROCM eye has been reported in the literature.Citation4,Citation5 Contralateral endophthalmitis following ROCM has not been reported before based on our PubMed search. Our patient presented with right ROCM, ipsilateral CRAO, and contralateral choroiditis, which later progressed to endogenous fungal endophthalmitis.
ROCM following tooth extraction has been reported in the literature.Citation6,Citation7 Following tooth extraction, the extraction socket acts as a port for the spread of mucormycosis from the oral cavity into the palate and sinuses.Citation6 This pathogenesis contradicts the usual route of infection, which begins in the nose and paranasal sinuses from the inhalation of fungal spores.Citation8 Thereafter, orbital involvement is due to contiguous spread from the sinuses or via the nasolacrimal duct. Further intracerebral spread extends from the orbit via the orbital apex, orbital vessels, or cribriform plate.
Talmi et alCitation9 reported that the most common clinical feature of ROCM is black nasal eschar in a review of 19 cases. Other clinical features are malaise, periorbital cellulitis, ptosis, ophthalmoplegia, infraorbital hypoesthesia, visual loss, fever, and headache.Citation9 Our patient presented with all of these aforementioned features. Other clinical features include conjunctival chemosis, nasal discharge, proptosis, deterioration of mental status, palatal involvement, facial palsy, hemiplegia, and seizure.Citation9
CRAO is a rare complication of ROCM with an incidence of 16%–20%.Citation4,Citation5 The pathogenesis of CRAO in ROCM is due to the contiguous spread of angioinvasive fungal infection from the orbit, which infiltrates the central retinal artery, causing necrotizing vasculitis and thrombosis. In contrast, the incidence of endophthalmitis complicating ROCM has been reported as 1%–6%.Citation4,Citation5 Contralateral endophthalmitis may be due to hematogenous dissemination of the fungal infection forming focal infected deposits in the choroid. The choroiditis under microscopic examination consists of granulomatous inflammation with causative organisms in the center and surrounding suppuration.Citation10 Further local spread of the lesion extends into the retina causing retinitis. Vitritis occurs when the infection breaks through the retina, seeding into the vitreous. The definition of endophthalmitis is reserved only for eyes with vitreous seeding.Citation11 In choroiditis alone, treatment is made with a systemic antifungal.Citation11 If it progresses to endophthalmitis, as in this case, an intravitreal antifungal is indicated.Citation11
In the treatment of fungal choroiditis and endophthalmitis, oral fluconazole was proposed as an alternative to systemic AMB because it has better intraocular penetration and fewer side effects.Citation11 Although oral fluconazole had been reported to be effective in clearing endophthalmitis where intravitreal AMB has failed, the causative organism in these reported cases was Candida.Citation12 Furthermore, systemic AMB remained the mainstay treatment for ROCM. In this patient, the subsequent resolution of endophthalmitis may be attributed to the higher intravitreal concentration of antifungal due to the intravitreal injection, as well as to the change from D-AMB to L-AMB, which was shown to have better intraocular penetration.Citation13 Only five in 19 cases of ROCM had positive blood culture.Citation9 In endogenous fungal endophthalmitis, blood culture is rarely positive, with only 11% of patients presenting with documented systemic fungal infection.Citation14 The vitreous culture was negative, possibly because the patient had been treated with a systemic antifungal prior to vitreous tap, and because there was only very minimal vitreous seeding.
Our patient was treated aggressively for both complications of ROCM. She survived this fatal condition with preservation of visual acuity in her left eye. The right eye remained blind following the CRAO. The infection was controlled with an appropriate systemic and intravitreal antifungal. She was very fortunate that her left visual acuity remained good, as the fovea was spared from the lesions and responded well to the treatment.
Conclusion
In conclusion, the early diagnosis and prompt treatment of ROCM is essential to improving the survival rate of the patient. A high index of suspicion in diabetic patients with imaging and nasal endoscopic evaluation is the key to an early diagnosis of ROCM. Both ipsilateral CRAO and contralateral endogenous endophthalmitis are rare and blinding complications of ROCM. In a case of unilateral ROCM, it is important to examine the contralateral eye for signs of endogenous spread, while monitoring it closely for progression.
Acknowledgments
This case report received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Disclosure
The authors report no conflicts of interest in this work.
References
- BrownSRShahIAGrinsteadMRhinocerebral mucormycosis caused by Apophysomyces elegansAmerican Journal of Rhinology19981242892929740925
- PetrikkosGDrogari-ApiranthitouMZygomycosis in immunocompromised non-haematological patientsMediterr J Hematol Infect Dis201131e201101221625316
- RodenMMZaoutisTEBuchananWLEpidemiology and outcome of zygomycosis: a review of 929 reported casesClin Infect Dis200541563465316080086
- BhansaliABhadadaSSharmaAPresentation and outcome of rhino-orbital-cerebral mucormycosis in patients with diabetesPostgrad Med J20048094967067415537854
- YohaiRABullockJDAzizAAMarkertRJSurvival factors in rhino-orbital-cerebral mucormycosisSurv Ophthalmol19943913227974189
- BakathirAAMucormycosis of the jaw after dental extractions: two case reportsSultan Qaboos Univ Med J200662778221748139
- KimJFortsonJKCookHEA fatal outcome from rhinocerebral mucormycosis after dental extractions: a case reportJ Oral Maxillofac Surg200159669369711381399
- VermaASinghVJindalNYadavSNecrosis of maxilla, nasal, and frontal bone secondary to extensive rhino-cerebral mucormycosisNatl J Maxillofac Surg20134224925124665188
- TalmiYPGoldschmied-ReouvenABakonMRhino-orbital and rhino-orbito-cerebral mucormycosisOtolaryngol Head Neck Surg20021271223112161726
- BrodRDFlynnHWJrClarksonJGPflugfelderSCCulbertsonWWMillerDEndogenous Candida endophthalmitis. Management without intravenous amphotericin BOphthalmology1990975666672 disc: 672–6742188195
- SmiddyWETreatment outcomes of endogenous fungal endophthalmitisCurr Opin Ophthalmol199893667010182104
- BorneMJElliottJHO’DayDMOcular fluconazole treatment of Candida parapsilosis endophthalmitis after failed intravitreal amphotericin BArch Ophthalmol199311110132613278216010
- BhansaliASharmaAKashyapAGuptaADashRJMucor endophthalmitisActa Ophthalmol Scand2001791889011167298
- EssmanTFFlynnHWJrSmiddyWETreatment outcomes in a 10-year study of endogenous fungal endophthalmitisOphthalmic Surg Lasers19972831851949076791

