Abstract
Purpose
To evaluate the lens edge interaction with the ocular surface with different edge designs using optical coherence tomography and to examine the effect of lens power on the lens edge interactions.
Methods
Four types of silicone hydrogel lenses with different edge designs (round-, semi-round-, chisel-, and knife-edged) at six different powers (+5.0, +3.0, +1.0, −1.0, −3.0, and −5.0 diopters) were fitted to both eyes of 20 healthy volunteers. Optical coherence tomography images were taken at the corneal center and at the limbus within 15–30 minutes after insertion. The images were evaluated with respect to two parameters: conjunctival indentation exerted by the lens edge; and the tear film gaps between the posterior surface of the lens and the ocular surface. The amount of conjunctival indentation was measured with the distortion angle of the conjunctiva at the lens edge.
Results
The degree of conjunctival indentation was highest with the chisel-edged design followed by the semi-round design (P<0.0001). Knife- and round-edged lenses exerted similar levels of conjunctival indentation that was significantly lower compared to chisel-edged lens (P<0.001). For each one of the tested lens edge designs, no significant difference was observed in the conjunctival indentation with respect to lens power. The chisel-edged lens produced the highest amount of conjunctival indentation for each one of the six lens powers (P<0.0001). Post-lens tear film gaps at the limbus were observed at most in the round-edge design (P=0.001).
Conclusion
The fitting properties of contact lenses may be influenced by their edge design but not by their lens power.
Introduction
A comprehensive evaluation which includes patient-related factors (palpebral aperture, lid position, iris diameter, and corneal topography) and contact lens-related factors (fitting profile, lens movement after blink, and lens modulus) is the essential step in the contact lens fitting process. This will minimize the risk of future failures or problems because of poor lens fitting. Discontinuation of contact lens wear is a major problem in contact lens practice. Inappropriate lens fit is responsible for 7% of contact lens discontinuations.Citation1 The primary reasons for discontinuation of contact lens wear over time have been reported to be discomfort, dryness, and red eyes.Citation2,Citation3 Comfort may be the most important factor in determining success versus failure of a contact lens wearer. Ocular discomfort, primarily caused by mechanical irritation linked to modulus, edge thickness, lens design, and inappropriate lens fit is the most important reason for discontinuation of contact lens wear.Citation1,Citation4,Citation5 Modulus values represent lens stiffness and resistance to shape change. Higher modulus can be related to mechanical complications, including contact lens papillary conjunctivitis, superior epithelial arcuate lesions, limbal epithelial hypertrophy, contact lens-induced conjunctival staining (CLICS), and conjunctival epithelial flaps (CEFs).Citation6–Citation9
Slit-lamp examination is often used for evaluation of contact lens fit but it is not always sufficient to give information to evaluate the lens fitting relationship between a contact lens and the ocular surface, and it is often difficult to objectively quantify soft contact lens fitting. Successful lens fitting is affected by many factors, such as corneal shape,Citation10 an adequate distribution of the contact lens weight over all the corneal surface, post-lens tear film,Citation11,Citation12 enough movement to provide an optimal tear turn-over, blink rate,Citation13 and lens material and design,Citation14 all of which provide minimal mechanical effect between the ocular surface and the contact lens.
Edge design is an extremely important and often underestimated parameter that can primarily affect comfort, lens positioning, lens motion, and overall fit. Both center thickness and edge thickness change with different lens powers.
Soft contact lenses cover the surface of the cornea and extend over the limbus onto the sclera by approximately 1 mm, hence topographical features of the corneoscleral junction as well as the central and the peripheral cornea are important to evaluate this appropriate fitting relationship. Recent studies have shown that there is a smooth, gradual transition in topography between the cornea and the sclera having a tangential profile in the majority of cases, and have suggested that the interaction between the lens edge and the ocular surface at the periphery has an equal or more important role for lens fitting.Citation15,Citation16 Hence, determination of the topography of the peripheral cornea, corneoscleral junction, and the anterior sclera provides crucial information for proper lens fitting.Citation15,Citation17 Optical coherence tomography (OCT) may be suitable for this task. Anterior segment OCT can image the entire ocular surface and the contact lens on the eye, obtain quantitative topography of the ocular surface, and generate thickness maps of the soft contact lenses.Citation18 OCT device is a noninvasive technique that can be used to visualize tears around contact lenses and to image the interactions between the ocular surface and the contact lens edge.Citation17,Citation19,Citation20 The indentation in the previous study was only subjectively graded in different lens edge design.Citation17 However, to the best of our knowledge, measuring the angle of conjunctival indentation for determination of quantitative assessment of lens edge–ocular surface interaction and the effect of lens power on these fitting characteristics using OCT has not been studied previously.
The purpose of this study was to evaluate the edge fitting and the interaction with the ocular surface of four silicone hydrogel lenses (SiHy) with different edge designs and materials using OCT, and also to examine the effect of lens power on these fitting characteristics.
Methods
A prospective, randomized (random integer generator; www.random.org/integers), and clinical comparative study was approved by the Marmara University Ethical Committee. The study followed the tenets of the Declaration of Helsinki. Informed consent was obtained from all subjects.
Both eyes of 20 healthy volunteers were fitted with SiHy. Slit-lamp examination was performed by the same examiner (SAT) to confirm the proper lens fitting, defined as having a good centration and enough movement (the post-blink movement within 0.2 to 0.4 mm). Each subject was enrolled in the study if they were aged between 18 and 40 years, and were successfully fit with the study lenses. There was no evidence or history of ocular surgery, dry eye, use of any ophthalmic medication, or ocular inflammation. None of the subjects wore contact lenses before or between study visits. Participants underwent a full ocular assessment. The order of the lens and diopter insertion was randomized for each eye of the subjects. Four types of SiHy contact lenses with different edge designs (round-, semi-round-, chisel-, and knife-edged) at six different powers (+5.0, +3.0, +1.0, −1.0, −3.0, and −5.0 diopters) were fitted. The study consisted of four visits for each subject. Each lens type was worn on a different visit, separated by at least 1 day. shows the characteristic features of SiHy contact lenses used in this study.
Table 1 Characteristics of the contact lenses used in the study
Imaging and measurements were performed by the RTVue OCT system (Optuvue, Inc., Fremont, CA, USA), which uses Fourier domain OCT technology. An 8 mm-wide scan was made on the horizontal meridian. Within 15–30 minutes after insertion, OCT images for the center, nasal, and temporal sides of the lens were obtained for each eye after a blink.Citation17 Images taken from the temporal side of the lens were evaluated with respect to two parameters: conjunctival indentation by the lens edge; and the tear film gaps between the posterior surface of the lens and the ocular surface. All OCT images were taken in a consulting room with controlled temperature (15°C–25°C) and humidity (30%–50%). All subjects were scheduled after 10 am to avoid the edematous cornea and the alteration of the tear film induced by sleep.Citation17,Citation21,Citation22
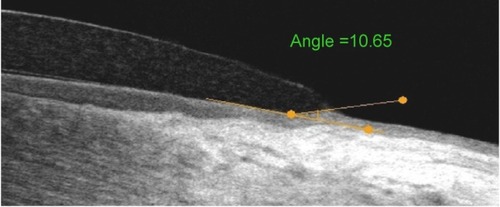
The amount of conjunctival indentation was measured with the distortion angle of the conjunctiva at the lens edge. An imaginary straight line was drawn along the contour of the conjunctival surface at the limbus. Another line was drawn passing along the axis of the indented conjunctiva at the lens edge. Then the angle at the intersection of these two lines was measured by the angle measurement tool on the OCT instrument. The larger the angle, the greater the degree of conjunctival indentation ().
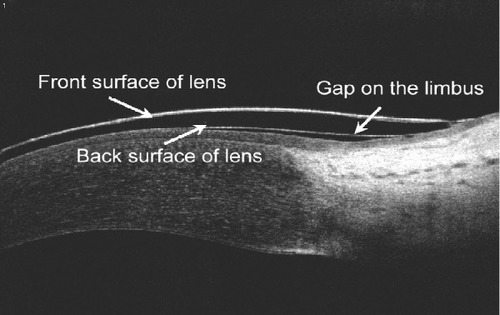
Tear film gaps at the limbus were also evaluated, as previously described.Citation17 The presence of these gaps was recorded for each study lens ().
Statistical analysis
Data analysis was performed by means of SPSS for Windows, version 17.0 (SPSS Inc., Chicago, IL, USA). The nonparametric analysis of variance (Kruskal–Wallis) and Dunn’s post hoc tests were used to determine significant differences of the measured conjunctival indentation among lens types and lens powers. The differences of occurrence frequency of tear film gaps among lenses were compared with chi-square test. Differences were considered to be statistically significant when the P-value was <0.05.
Results
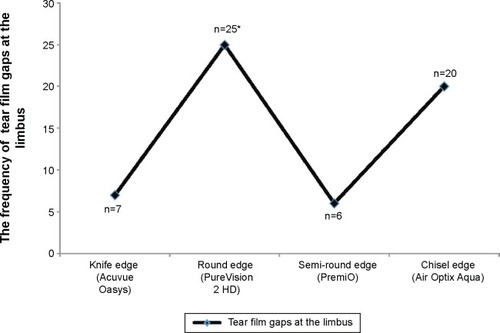
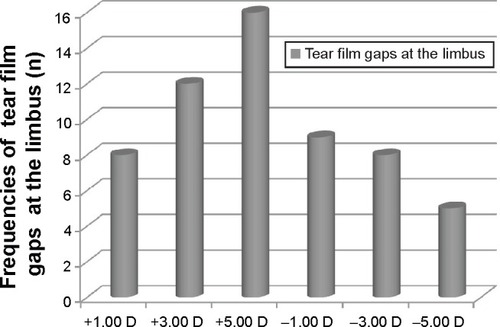
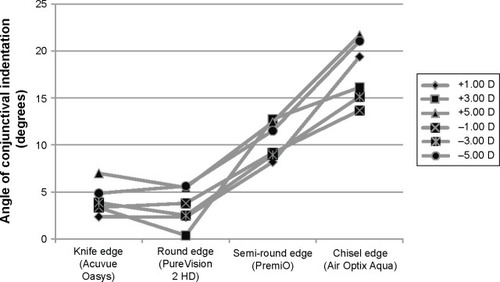
Forty eyes of 20 participants (ten women, ten men) with a mean age (± standard deviation) of 25.1±3.8 (range, 18–38) years were enrolled in this study. The average of keratometric values for right and left eyes were 43.73±1.69 and 43.43±1.53 diopters, respectively. Conjunctival indentation exerted by the lens edge for different edge designs are presented in . When all data (n=480) were examined regardless of lens power, conjunctival indentation was highest with the chisel-edge design followed by the semi-round-edge design (P<0.0001) (). There were no significant differences in the conjunctival indentation between the knife-edge and the round-edge designs (P>0.05). The distribution of conjunctival indentation according to lens power is shown in . The chisel-edged lens produced the highest amount of conjunctival indentation for each of the six lens powers (P<0.0001). For each of the tested lens edge designs, no significant difference was observed in the conjunctival indentation with respect to lens power (P>0.05). Post-lens tear film gaps at the limbus were present in 12% of all eyes. Post-lens tear film gaps at the limbus were observed at most with the round-edge design followed by the chisel-edge design (). Post-lens tear film gaps at the limbus were observed mostly with plus-power lenses (P=0.017) ().
Figure 3 Angle of conjunctival indentation was measured by optical coherence tomography for different edge designs.
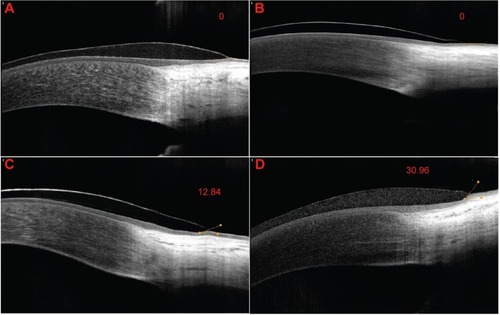
Figure 4 Comparison of conjunctival pressure exerted by the lens edge for different edge designs, regardless of the lens power.
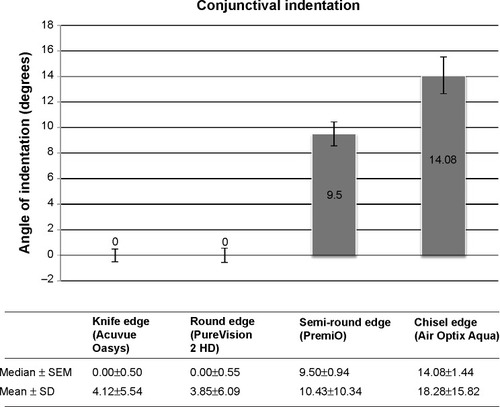
Figure 5 Distribution of conjunctival indentation according to lens power and edge design.
Discussion
Slit-lamp examination is the gold standard method in the evaluation of appropriate lens fit. Although this simple method provides proper assessment in the majority of patients, it gives limited information about the interaction between the ocular surface and the posterior surface of the contact lens. The posterior lens surface interacts with the cornea, limbus, and the bulbar conjunctiva, and the anterior surface has close relationship with the palpebral conjunctiva and upper/lower lid margins. So, a better understanding of this interaction will provide more valuable information to prevent complications associated with contact lens wear.
SiHy lens materials have a higher modulus than conventional hydrogel lenses and are more prone to induce mechanical complications.Citation5 Two recently described clinical conditions related with mechanical interaction between the conjunctival tissue and the contact lens are CEFs and CLICS.Citation5,Citation8,Citation23,Citation24 CEFs are mostly located at the superior and inferior quadrants of the bulbar conjunctiva adjacent to the lens edge and they are believed to occur due to repeated interaction of the lens periphery with the ocular surface causing delamination of the superficial layers of the conjunctival epithelium. Although CEF is an asymptomatic condition, its long-term risk for any inflammatory response is not yet clear. The occurrence of CEFs has been linked to modulus of rigidity of the lens material, edge design, and wearing modality.Citation5 Previous clinical studies have suggested that chisel-edge-design SiHy lenses induce a higher incidence of CEFs than the round-edge-design ones,Citation5,Citation23 and continuous wear modality is more likely to exacerbate this mechanical effect compared to daily wear.Citation5 This implies that the management of CEFs may involve modifying the wearing modality and changing to a round-edge lens design. The other mechanical complication is CLICS, which is more common with certain lens edge configurations than others. Direct contact between the lens periphery and the ocular surface irritating the conjunctival epithelium causes staining at the limbal area. Maissa et alCitation25 investigated the conjunctival staining produced in the circumlimbal region by SiHy lenses with different edge designs, and also the relationship between circumlimbal staining and comfort. They reported that round-edge design produced the lowest staining while knife-edge design, being in close apposition with the ocular surface, produced the highest. Balafilcon A and lotrafilcon B lenses have a similar material rigidity, but circumlimbal staining produced by a balafilcon A lens was lower than that produced by a lotrafilcon B lens. This finding suggested that the lens edge design is the primary factor in controlling circumlimbal staining.Citation25 When the multifactorial comfort analysis was evaluated, the lens edge design was the primary influential factor that affected lens comfort: the knife-edge design had the best comfort; the round-edge design had the worst comfort. There was an inverse relationship between circumlimbal staining and lens comfort, and the authors concluded that CLICS was not a significant factor associated with decreased comfort.Citation25 In our study, we observed the highest amount of conjunctival indentation with the chisel-edge design lens followed by the semi-round-edge design lens. Knife and round-edge designs induced the lowest amount of conjunctival indentation. In a recent study, Shen et alCitation17 used an analog scale (0%, 25%, 50%, 75%, 100%) for indicating the degree of conjunctival buildup around the lens edge and compared four different types of soft contact lenses (two SiHy and two hydrogel contact lenses) with two different edge designs (rounded and angled). Similar to our results, they found no significant difference in the conjunctival buildup between the two SiHy lenses with rounded (PureVision; Bausch & Lomb Incorporated, Bridgewater, NJ, USA) and angled-edge designs (Acuvue Advance; Vistakon, Johnson&Johnson Vision Care, Inc., Jacksonville, FL, USA). However, there was a significant difference among lower modulus hydrogel lenses in that the knife-edged lens (Acuvue 2; Vistakon) favored less conjunctival indentation than the round-edged one (Biomedics 55; CooperVision, CooperVision Inc., Fairport, NY). Wolffsohn et alCitation26 investigated four experimental lens designs with the same material (senofilcon A) to evaluate the interaction of mid-peripheral lens shape profile (8.4 mm base curve and 8.8 mm base curve) and lens edge design (knife-edge design and chisel-edge design) with the ocular surface using OCT. They reported that epithelial indentation did not change with mid-peripheral lens shape profile or with edge design after optical distortion was corrected, unlike the findings of Shen et alCitation17 and our study.
The present study was the first attempt to demonstrate the effect of lens power on lens fitting characteristics using OCT. In contrast to our presumption that high-minus-power lenses with thicker lens edges would indent conjunctiva more, lens power, regardless of lens edge design, was observed to have no significant influence on the conjunctival indentation exerted by the lens edge.
The dynamic interaction between the contact lens and the tear film influences several aspects of ocular physiology as well as vision and comfort. Tear exchange is of key interest in providing essential supplies to the tissues under the contact lens and in the removal of deposits, and the tear film layer is also important to reduce the friction between the ocular surface and the lens. The edge design may play an important role in the circulation of the tear fluid under the lens, and in the movement of the lens over the conjunctiva and the cornea. A higher level of the conjunctival buildup at the lens edge has a negative effect on tear exchange beneath the lens that causes tear film gaps between the contact lens and the ocular surface.Citation17 The presence of gaps between the lens and the cornea may also be an indicator of how the contact lens conforms to the surface of the cornea. In our study, greater frequencies of tear film gaps at the limbus occurred with the round-edge followed by the chisel-edge-design lenses, with both having a higher modulus than the other two edge designs. This finding is in agreement with data previously reported by Shen et alCitation17 who stated that the round-edged lenses (Biomedics 55 and PureVision) produced a higher percentage of tear film gaps on the cornea than the angle-edged lenses (Acuvue 2 and Acuvue Advance), and round-edged lenses (PureVision) had the highest percentage of tear film gaps at the limbus. This shows that the occurrence of tear film gaps between the lens and the cornea is associated not only with the edge configuration but also with the modulus of the material. SiHy lenses with a higher modulus may not conform to the shape of the eye compared to SiHy lenses with a lower modulus. As a consequence, the “stiffer” material does not drape over the cornea easily.Citation27
Tear exchange under the contact lens is likely to be impacted by lens power besides the modulus of the material and the edge configuration as both center thickness and edge thickness change with different lens powers. In this study, limbal tear film gaps were mostly observed with plus-power lenses. The lens edge thickness in plus-power lenses is thinner than the apex. According to a recent study, touch points between the lens and the ocular surface were observed at the corneal apex, at the mid-periphery of the cornea and the limbus.Citation17 Hence, these touch points and thickness differences between lens powers may have an impact on the circulation of the tear film, resulting in entrapment of tears in the form of tear film gaps. The dynamics of lens movement may also influence the tear exchange.Citation28 Confirmation of these hypotheses needs to be elucidated in further studies.
In summary, this was the first study to demonstrate the quantitative assessment of the conjunctival indentation and to determine the effect of lens power on the lens fitting and tear exchange using OCT. Our results suggest that the fitting properties of contact lenses may be influenced by their edge design but not by lens power. Anterior segment OCT is a useful method to evaluate the fitting characteristics of contact lenses and can be used to show lens edge and ocular surface interaction. OCT findings of lens fit can be evaluated in further studies with respect to subjective comfort scores, clinical findings, and the lens movements.
Acknowledgments
This work has previously been presented at 41st ECLSO Congress, Istanbul, Turkey on 9–11 September 2011. Best oral presentation award was attributed to this paper.
Disclosure
The authors report no conflicts of interest in this work.
References
- YoungGWhy one million contact lens wearers dropped outCont Lens Anterior Eye2004272838516303533
- YoungGVeysJPritchardNColemanSA multi-centre study of lapsed contact lens wearersOphthalmic Physiol Opt200222651652712477016
- PritchardNFonnDBrazeauDDiscontinuation of contact lens wear: a surveyInt Contact Lens Clin199926615716211384832
- BegleyCGCafferyBNicholsKKChalmersRResponses of contact lens wearers to a dry eye surveyOptom Vis Sci2000771404610654857
- Santodomingo-RubidoJWolffsohnJGilmartinBConjunctival epithelial flaps with 18 months of silicone hydrogel contact lens wearEye Contact Lens2008341353818180681
- SkotnitskyCCNaduvilathTJSweeneyDFSankaridurgPRTwo presentations of contact lens-induced papillary conjunctivitis (CLPC) in hydrogel lens wear: local and generalOptom Vis Sci2006831273616432470
- DumbletonKAdverse events with silicone hydrogel continuous wearCont Lens Anterior Eye200225313714616303486
- GrahamADTruongTNLinMCConjunctival epithelial flap in continuous contact lens wearOptom Vis Sci2009864e324e33119225431
- SynderCModulus and its effect on contact lens fitContact Lens Spectrum2007222
- YoungGSchniderCHuntCEfronSCorneal topography and soft contact lens fitOptom Vis Sci201087535836620386354
- LittleSABruceASHydrogel (Acuvue) lens movement is influenced by the postlens tear filmOptom Vis Sci19947163643708090438
- LittleSABruceASPostlens tear film morphology, lens movement and symptoms in hydrogel lens wearersOphthalmic Physiol Opt199414165698152823
- GoldingTRBruceASGaterellLLLittleSAMacnamaraJSoft lens movement: effect of blink rate on lens settlingActa Ophthalmol Scand19957365065119019373
- TranoudisIEfronNIn-eye performance of soft contact lenses made from different materialsCont Lens Anterior Eye200427313314816303536
- HallLAYoungGWolffsohnJSRileyCThe influence of corneoscleral topography on soft contact lens fitInvest Ophthalmol Vis Sci20115296801680621685339
- MeierDDas corneo-skleral-profile-ein kriterium individueller kontactlinsenanpassung [The corneo-scleral profile – a criterion of individual contact lens fitting]Die Kontaklinse1992264411 German
- ShenMCuiLRileyCWangMRWangJCharacterization of soft contact lens edge fitting using ultra-high resolution and ultra-long scan depth optical coherence tomographyInvest Ophthalmol Vis Sci20115274091409721372023
- ShenMWangMRWangJYuanYChenFEntire contact lens imaged in vivo and in vitro with spectral domain optical coherence tomographyEye Contact Lens2010362737620093938
- WangJJiaoSRuggeriMShoushaMAChenQIn situ visualization of tears on contact lens using ultra high resolution optical coherence tomographyEye Contact Lens2009352444919265323
- KaluznyBJKaluznyJJSzkulmowskaASpectral optical coherence tomography: a new imaging technique in contact lens practiceOphthalmic Physiol Opt200626212713216460312
- PatelSBevanRFarrellJCDiurnal variation in precorneal tear film stabilityAm J Optom Physiol Opt19886531511543364523
- ShenMWangJQuJDiurnal variation of ocular hysteresis, corneal thickness, and intraocular pressureOptom Vis Sci200885121185119219050473
- LøfstrømTKAA conjunctival response to silicone lens wear: a new finding reveals how silicone hydrogel lenses may affect the conjuctival epitheliumContact Lens Spectrum20052094244
- LinMCYehTNMechanical complications induced by silicone hydrogel contact lensesEye Contact Lens201339111512423271473
- MaissaCGuillonMGarofaloRJContact lens-induced circumlimbal staining in silicone hydrogel contact lenses worn on a daily wear basisEye Contact Lens2012381162622146704
- WolffsohnJSDrewTDhalluSSheppardAHofmannGJPrinceMImpact of soft contact lens edge design and midperipheral lens shape on the epithelium and its indentation with lens mobilityInvest Ophthalmol Vis Sci20135496190619723942975
- DumbletonKAChalmersRLMcNallyJBayerSFonnDEffect of lens base curve on subjective comfort and assessment of fit with silicone hydrogel continuous wear contact lensesOptom Vis Sci2002791063363712395917
- CuiLShenMWangMRWangJMicrometer-scale contact lens movements imaged by ultrahigh-resolution optical coherence tomographyAm J Ophthalmol20121532275283.e27121920493