Abstract
Purpose
To evaluate risk factors associated with posterior subcapsular cataract (PSC) development and the relationship between vitamin D deficiency and etiology of PSC.
Methods
Of 195 consecutive patients from a private ophthalmology practice, diagnosed with PSC, serum vitamin D3 (25-OH D) levels were obtained for 175, and associations among risk factors, comorbidities, and PSC were assessed.
Results
In all 175 PSC patients, mean 25-OH D levels were low (24 ng/mL ±11 SD) compared with age/sex-matched standards. Significant differences in 25-OH D levels were noted between PSC subjects taking/not taking calcium supplements, systemic steroids, osteoporosis medications, etc. Alone, smoking status and calcium channel blockers and/or topical steroids use made no significant difference in PSC subjects 25-OH D levels, but two or more of these factors were associated with lowered levels of 25-OH D (P<0.001). Low vitamin D was correlated with female sex, autoimmune disease, and non-skin cancer diagnosis, but not with age, or other comorbidities or medication use. In five early-stage PSC patients taking 5,000 IU of 25-OH D daily for vitamin D deficiency, there was resolution of their cataracts during the 2-year follow-up period.
Conclusion
Vitamin D levels for most PSC patients fell below the 30 ng/mL calcium homeostasis threshold. Some comorbidities and non-ophthalmic interventions are associated with the development of PSC at less depressed levels of 25-OH D. In this series, vitamin D deficiency was associated with PSC cataract, suggesting that raising the level of vitamin D intake may reduce PSC incidence.
Introduction
Posterior subcapsular cataract (PSC) is clinically common and known to be visually debilitating, having a high societal burden in terms of lost work and need for early surgical intervention. Prolonged corticosteroid use can lead to the development of PSC.Citation1–Citation3 Although other described risk factorsCitation4 include myopia,Citation5 various skin disorders,Citation6 diabetes,Citation7 intraocular inflammation or trauma,Citation8 retinitis pigmentosa,Citation9 and smoking,Citation10 the majority of PSCs have an unknown etiology.Citation11 PSC resembles the hypocalcemic cataract described in the endocrine and veterinary literature, and can be reproduced in vitro or in vivo by incubating clear excised lenses in hypocalcemic media or by feeding animals diets deficient in calcium or in severe vitamin D deficiency states.Citation12–Citation16 It was noted by one of the authors that within a large series of PSC cases, patients frequently presented with vitamin D insufficiency or deficiency. A retrospective examination of other risk factors was undertaken to establish any possible interactions with vitamin D deficiency as causative mechanisms of PSC formation, supporting the validity of the hypocalcemic animal model in humans.
Methods
This study comprised 195 of 1,585 consecutive cataract patients seen in a private practice ophthalmology clinic between June 1, 2008 and June 1, 2010, and diagnosed with PSC/anterior subcapsular cataract (ASC) alone or mixed cataract PSC/ASC combined with nuclear or cortical opaci-ties. Histories and risk factors were recorded by the senior author including steroid use, use of calcium supplements or osteoporosis medications, prior trauma, autoimmune or skin cancer disorders, diabetes, cancer diagnosis, or cardiopulmonary disease. The use of concomitant medications for their control was taken from the chart record (). Levels of 25-OH D were obtained or available for 175 of 195 PSC patients using either the DiaSorin LIAISON® Immunochemiluminometric assay or the QuestAssureD™ liquid chromatography, tandem mass spectrometry. Both methods, as performed by commercial laboratory testing services, had an analytical sensitivity of at least 4 ng/mL. Associations between risk factors and comorbidities and the presence of PSC were then assessed. A t-test for independent samples was used to determine whether the differences of 25-OH D levels in PSC subjects with and without risk factors and concomitant medications were statistically different from zero. In addition, a linear regression analysis was carried out to model the relationship between the level of 25-OH D and variables such as age, sex, autoimmune disease, hypertension, skin cancer, and antidepressant use. Access to anonymized clinical records by nonclinical personnel was approved by the Washington Regional Medical Center Institutional Review Board. All patients had received routine medical and surgical care. Patients whose cataracts interfered with daily vision function were scheduled for cataract surgery. Those whose cataracts were minimally symptomatic or asymptomatic were followed without surgery. Patients in this interval of care newly diagnosed with low levels of vitamin D were treated and referred to their primary care physician for follow up. This was a retrospective chart review study, and all patients received routine care with no experimental intervention.
Table 1 Patient demographics, cataract types, comorbidities, and risk factors
Results
All eyes were examined in the dilated state. Anterior and posterior subcapsular opacities were identified with the slit lamp set for retroillumination, spanning a range from axial retrodots to dense fibrotic plaques involving the capsule and immediately adjacent degenerating cortical lens fibers. In this study, all degrees of PSC and ASC were included. Lens Opacity Classification System IIICitation17 grades P1–P5 represented the majority of subcapsular cataracts. Additionally, some PSCs were greater than P5, involving the entire posterior capsule, and some patients had predominantly anterior subcapsular opacities identical to posterior subcapsular opacities, except for anterior location and more severe functional visual disturbance. Of 1,585 unique cataract patients seen during the study period, 12.3% had PSC (195/1,585), while 27.6% of patients who received cataract surgery had a PSC component (164/595). Vitamin D levels were evaluated for 175 (most bilateral; 62.3% female, 37.7% male; most were Caucasian) PSC patients (76% confirmed after diagnosis by serum testing, 24% as lab values were obtained from history/referral chart). Mean 25-OH D level of PSC cataract patients was on the low normal end of the spectrum (24 ng/mL ± 11SD) compared to age/sex-matched national standards for vitamin D levels.Citation18 This serum 25-OH D level has been defined by some authorities as vitamin D insufficiency.Citation19
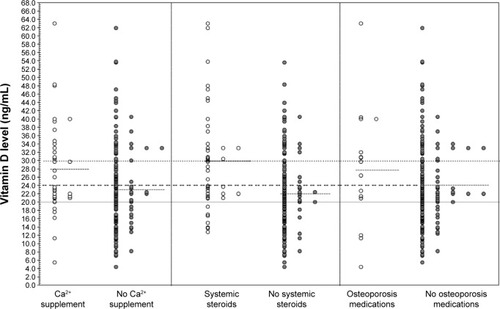
Significant differences in 25-OH D levels were noted between PSC subjects with and without certain risk factors and variables, including with or without calcium supplementation (28±11 vs 23±10 ng/mL; P=0.01), systemic steroids exposure (30±12 vs 22±9 ng/mL; P<0.001), or taking osteoporosis medications or not (28±14 vs 24±10 ng/mL; P=0.05) (). Smoking, use of calcium channel blockers, or topical steroid use alone showed no significant difference in 25-OH D levels between PSC patients with that variable or without it. However, marginally significant lower levels of vitamin D were noted when two or more variables were present compared with none of the variables (23±11 vs 25±11 ng/mL; P=0.06) (). Linear regression analysis showed that 25-OH D levels also correlated with female sex (P=0.042), autoimmune disease (P<0.001), (non-skin) cancer diagnosis (P=0.016), but not with age, hypertension, eye trauma or inflammation (not shown), cardiopulmonary disease (not shown), diabetes (not shown), or antidepressant use (). Five patients with early-stage multiple axial posterior or anterior subcapsular water cleft cysts and retro dots who began taking 5,000 IU of vitamin D3 (25-OH D) daily, completely resolved their early-stage cataracts.
Table 2 Significantly different 25-OH vitamin D levels in PSC subjects with and without risk factors and concomitant medications
Table 3 Similar 25-OH vitamin D levels in PSC subjects with and without other risk factors and concomitant medications
Table 4 Linear regression analysis of additional covariates associated with vitamin D levels in PSC subjects
Discussion
Low vitamin D status is extremely common worldwide when the cut point of <30–32 ng/mL is applied. In the USA, vitamin D levels have fallen over the last few decades due to fewer work and recreation-related outdoor activities, including more air conditioning in homes and offices, television viewing, computer use, and intentional sun avoidance (ie, sun screen use).Citation20 Milk fortification and dietary supplement have not closed the gap. The National Health and Nutrition Examination Surveys conducted between 1988 and 1994 compared with those conducted between 2001 and 2006 showed a mean decrease in age-specific 25-OH D levels of 5–10 ng/mL for Caucasian men and 2–6 ng/mL for Caucasian women. Other racial groups typically exhibited lower vitamin D levels even in the reference decades. Comorbidities on the rise due to lifestyle diseases or the aging demographic, including diabetic nephropathy and bone and mineral metabolism defects, may also be associated with vitamin D insufficiency or deficiency.Citation21,Citation22 Several agencies and guides now categorize serum 25-OH D levels <10.0 ng/mL as very deficient with impaired bone mineralization (rickets/osteomalacia), <20 ng/mL as deficiency, 20–29 ng/mL as insufficiency, and above 30 ng/mL vitamin D as normal serum levels. The Institute of Medicine recently revised the Recommended Dietary Allowances of vitamin D in order to maintain serum 25-OH D at or above 50 nM (20 ng/mL) to sustain bone density and calcium absorption and minimize the risk of osteomalacia and rickets.Citation23 But because vitamin D insufficiency seems to be associated with a number of adverse health effects, scientists and health professionals are advocating increasing vitamin D status to above 75 nM (30 ng/mL) 25-OH D.Citation24 Furthermore in a large cohort study, the association of serum 25-OH D levels with all-cause mortality was shown to be a nonlinear inverse association with risk increasing slightly at 25-OH D concentrations, <75 nM (30 ng/mL) and was most strongly increased in subjects with vitamin D deficiency.Citation25 In this series, the mean 25-OH D level for many more PSC patients was below this value ().
Figure 1 Individual PSC patient serum 25-OH D3 levels and associated concomitant medications.
Abbreviation: PSC, posterior subcapsular cataract.
Vitamin D is the chief regulator of systemic calcium as well as calcium levels in the serum and aqueous humor. Serum levels of vitamin D are negatively (P<0.01) correlated with parathyroid (PTH). There is a stable plateau for serum PTH levels as long as serum 25-OH D levels remain above 31 ng/mL, but increase when 25-OH D levels drop below 31 ng/mL.Citation26 Historic observations also suggest that PSC can be associated with PTH disorders.Citation27,Citation28 Disruption of calcium homeostasis in the lens has been shown experimentally to produce lens opacification via several mechanisms, including lens protein aggregation, enhanced migration of lens epithelial cells (LECs) onto the posterior capsule, abnormal differentiation of LECs into fibrocytes, lens fiber gap junction uncoupling, and loss of activity of calcium channels.Citation29,Citation30 Paradoxically, both hypocalcemia and hypercalcemia have been observed in association with experimental cataract models and in other forms of human cataract.Citation31 It is possible that causative factors for PSC cataracts fall into a bimodal distribution pattern for vitamin D levels, where one class of PSC cataracts develops in subjects with 25-OH D levels above 28–32 ng/mL and the other in subjects with lower levels. The group with levels below 28–32 ng/mL may have no other known risk factors for PCS except systemic hypocalcemia/low aqueous calcium. The group above ∼30 ng/mL may have known risk factors such as systemic steroid exposure, use of calcium supplements, or a need for osteoporosis medications.
PSC patients in the series reported here who were or had been using systemic steroids (but not topical steroids) showed a mean level of 25-OH D of 30 ng/mL, significantly higher than PSC subjects without systemic steroid exposure whose mean level was 22 ng/mL ( and ). Several studies have noted the association between the use of inhaled or oral corticosteroids and the long-term cataract risk.Citation32 Several cataractogenic mechanisms of action have been suggested for steroids, including modulation of LEC migrationCitation33 and downregulation of LEC fibroblast growth factor receptor and β-crystallin protein.Citation32 LECs exhibit a steroid-binding membrane protein whose activities are mediated in part by calcium.Citation34 Administration of a calcium-containing compound can reverse the cataract-inducing activity of steroids in an animal model.Citation35 The failure to find an association between vitamin D levels in individuals with PSC, and comorbidities such as asthma and chronic obstructive pulmonary disease where steroid use would be expected, may be a result of their use of other management medications, insufficient duration of steroid use, or just a sample size limitation. The involvement of calcium signaling in PSC formation appears complex, given that individuals taking calcium supplements and osteoporosis medications appeared to have higher 25-OH D levels despite PSC formation. In the instance of patients on Ca2+ supplements, usually for incipient osteopenia or a diagnosis of osteoporosis, these supplements often include vitamin D in the formulation contributing to their elevated 25-OH D level. It has been shown that as long as vitamin D levels are adequate, calcium intake need be no higher than 800 mg/dayCitation36 for osteoporosis. Those taking calcium channel blockers had similar levels of vitamin D to those not using these medications. Because Ca2+ channel blockers are prescribed for hypertension, also not strongly correlated with vitamin D deficiency, this may also not be unexpected.
In the early stage of ASC and PSC, vitamin D deficiency affects the calcium metabolism of the LEC, causing cell junctions to separate and creating cystic vacuoles that are visible as water cleft cysts. With time, the lens tissue becomes cloudy and distorted with calcium deposition; microscopically, the clear LECs turn into cloudy fibrocytes, eventually breaking down and depositing Ca2+ on the capsule forming white lens retrodots.Citation37 In five patients in this series with evidence of early axial subcapsular water cleft cysts,Citation38 their lenses unexpectedly normalized after taking 5,000 IU of vitamin D3 taken to treat their low vitamin D level.
Although 25-OH D is available in the human diet, it can also be synthesized from ultraviolet irradiation of 7-dehydroxycholesterol, a precursor present in mammalian skin. Following cutaneous production or intestinal absorption from nutritional sources, it is metabolized to 25-OH D3 in the liver by cytochrome P450 (CYP) 27A1. CYP27B1 in the kidney then converts this compound to the physiologically active hormone, 1α,25-dihydroxyvitamin D (calcitriol).Citation39 Calcitriol binds to the intracellular vitamin D receptor (VDR), which heterodimerizes with retinoic X receptor and binds DNA. The protein transcription thus initiated regulates calcium metabolism. The gene for VDR has variant polymorphisms in a fraction of American population with various diseases.Citation40 Patients with the E420A mutant form of VDR are known to have vitamin D-resistant rickets, requiring vitamin D supplementation at doses up to 100,000 IU daily to maintain adequate blood levels.Citation41 It is suspected that less severe forms of VDR impairment make it harder for some individuals to maintain adequate vitamin D3 levels without supplementation. It is hoped that with increasing and inexpensive gene testing methods, other haplotype VDR variations may be characterized to help identify patients who could benefit from additional vitamin D supplementation and thereby reduce their risk of PSC cataract formation and other allied disorders.
Acknowledgments
Craig J Brown, MD FACS and Faical Akachi, PhD would like to thank CCS Associates for assistance in preparing this manuscript.
Disclosure
The authors report no conflicts of interest in this work.
References
- JickSSVasilakis-ScaramozzaCMaierWCThe risk of cataract among users of inhaled steroidsEpidemiology200112222923411246585
- PraveenMRShahGDVasavadaARPosterior capsule opacification in eyes with steroid-induced cataracts: comparison of early resultsJ Cataract Refract Surg2011371889621183104
- UrbanRCJrCotlierECorticosteroid-induced cataractsSurv Ophthalmol19863121021103541262
- DelcourtCCristolJPTessierFRisk factors for cortical, nuclear, and posterior subcapsular cataracts: the POLA studyAm J Epidemiol2000151549750410707918
- BrownNAHillARCataract: the relation between myopia and cataract morphologyBr J Ophthalmol19877164054143620419
- SasakiKKojimaMNakaizumiHEarly lens changes seen in patients with atopic dermatitis applying image analysis processing of Scheimpflug and specular microscopic imagesOphthalmologica1998212288949486546
- BronAJSparrowJBrownNAThe lens in diabetesEye (Lond)1993722602757607346
- HooperPLRaoNASmithRECataract extraction in uveitis patientsSurv Ophthalmol19903521201442237757
- DilleyKJBronAJHabgoodJOAnterior polar and posterior subcapsular cataract in a patient with retinitis pigmentosa: a light-microscopic and ultrastructural studyExp Eye Res19762221551671269540
- HillerRSperdutoRDPodgorMJCigarette smoking and the risk of development of lens opacities. The Framingham studiesArch Ophthalmol19971159111311189298050
- VasavadaARMamidipudiPRSharmaPSMorphology of and visual performance with posterior subcapsular cataractJ Cataract Refract Surg200430102097210415474821
- PleskerRHetzelUSchmidtWCataracts in a laboratory colony of African green monkeys (Chlorocebus aethiops)J Med Primatol200534313914615860122
- RingvoldASagenEBjerveKSThe calcium and magnesium content of the human lens and aqueous humour. A study in patients with hypocalcemic and senile cataractActa Ophthalmol (Copenh)19886621531563389087
- SrivastavaVKSrivastavaSKVitamin D3 and calcitonin-induced regulation of calcium and phosphate in rat lens – its significance in cataract formationAnn Ophthalmol19892141491522543257
- SrivastavaVKSrivastavaSKGargMEndocrine regulation of calcium and phosphate in rat eye lens and its significance in cataract formationIndian J Exp Biol19902843653682161790
- TakahashiHCa(2+)-ATPase activity in the hypocalcemic cataractNihon Ganka Gakkai Zasshi19949821421498109458
- ChylackLTWolfeJKSingerDMThe Lens Opacities Classification System IIIArch Ophthalmol199311168318368512486
- LookerACJohnsonCLLacherDAPfeifferCMSchleicherRLSemposCTVitamin D status: United States, 2001–2006NCHSData Brief20115918
- GindeAALiuMCCamargoCAJrDemographic differences and trends of vitamin D insufficiency in the US population, 1988–2004Arch Intern Med2009169662663219307527
- LinosEKeiserEKanzlerMSun protective behaviors and vitamin D levels in the US population: NHANES 2003–2006Cancer Causes Control201223113314022045154
- DiazVAMainousAG3rdCarekPJThe association of vitamin D deficiency and insufficiency with diabetic nephropathy: implications for health disparitiesJ Am Board Fam Med200922552152719734398
- GutierrezOMFarwellWRKermahDRacial differences in the relationship between vitamin D, bone mineral density, and parathyroid hormone in the National Health and Nutrition Examination SurveyOsteoporos Int20112261745175320848081
- Institute of MedicineDietary Reference Intakes for Calcium and Vitamin DWashington, DCThe National Academies Press2011
- HeaneyRPHolickMFWhy the IOM recommendations for vitamin D are deficientJ Bone Miner Res201126345545721337617
- SchöttkerBHaugUSchomburgLStrong associations of 25-hydroxyvitamin D concentrations with all-cause, cardiovascular, cancer, and respiratory disease mortality in a large cohort studyAm J Clin Nutr201397478279323446902
- ChapuyMCPreziosiPMaamerMPrevalence of vitamin D insufficiency in an adult normal populationOsteoporos Int1997754394439425501
- GoswamiRBrownEMKochupillaiNPrevalence of calcium sensing receptor autoantibodies in patients with sporadic idiopathic hypoparathyroidismEur J Endocrinol2004150191814713274
- HavivYSSafadiRZamirEA rapidly progressive cataract in a patient with autoimmune hypoparathyroidism and acute liver and renal failureAm J Nephrol199919452352610460947
- GuptaPDJoharKVasavadaACausative and preventive action of calcium in cataracto-genesisActa Pharmacol Sin200425101250125615456524
- MaddalaRNagendranTde RidderGGL-type calcium channels play a critical role in maintaining lens transparency by regulating phosphorylation of aquaporin-0 and myosin light chain and expression of connexinsPLoS One201385e6467623734214
- JedziniakJANicoliDFYatesEMOn the calcium concentration of cataractous and normal human lenses and protein fractions of cataractous lensesExp Eye Res1976233325332976373
- WangJJRochtchinaETanAGUse of inhaled and oral corticosteroids and the long-term risk of cataractOphthalmology2009116465265719243828
- JamesERThe etiology of steroid cataractJ Ocul Pharmacol Ther200723540342017900234
- ZhuXLSextonPSCenedellaRJCharacterization of membrane steroid binding protein mRNA and protein in lens epithelial cellsExp Eye Res200173221321911446771
- VelpandianTNirmalJGuptaPEvaluation of calcium dobesilate for its anti-cataract potential in experimental animal modelsMethods Find Exp Clin Pharmacol201032317117920448859
- SteingrimsdottirLGunnarssonOIndridasonOSRelationship between serum parathyroid hormone levels, vitamin D sufficiency, and calcium intakeJAMA2005294182336234116278362
- VrensenGFde WolfACalcium distribution in the human eye lensOphthalmic Res199628Suppl 278858883093
- TanAGMitchellPRochtchinaELens retrodots and vacuoles and their associations with the prevalence and incidence of age-related cataractEye (Lond)201226456857522193877
- BikleDDVitamin D: newly discovered actions require reconsideration of physiologic requirementsTrends Endocrinol Metab201021637538420149679
- ZmudaJMCauleyJAFerrellREMolecular epidemiology of vitamin D receptor gene variantsEpidemiol Rev200022220321711218372
- MalloyPJZhouYWangJHereditary vitamin D-resistant rickets (HVDRR) owing to a heterozygous mutation in the vitamin D receptorJ Bone Miner Res201126112710271821812032
