Abstract
Purpose
To compare the final changes in corneal wavefront aberration by limbal relaxing incisions (LRIs) after cataract surgery.
Methods
This prospective cumulative interventional nonrandomized case study included cataract and astigmatic patients undergoing LRIs and phaco with intraocular lens implantation. LRIs were planned using Donnenfeld nomogram. The root mean square of corneal wave aberration for total Z(n,i)(1≤n≤8), astigmatism Z(2,±1), coma Z(3–5–7,±1), trefoil Z(3–5–7,±2), spherical Z(4–6–8,0), and higher-order aberration (HOA) Z(3≤n≤8) was examined before and 3 years after surgery (optical path difference-Scan II [OPD-Scan II)]. Uncorrected distance visual acuity and best-corrected distance visual acuity (CDVA) for distance, keratometric cylinder, and variations in average corneal power were also analyzed.
Results
Sixty-four eyes of 48 patients were included in the study. Age ranged from 42 to 92 years (70.6±8.4 years). After LRIs, uncorrected distance visual acuity and best-corrected distance visual acuity improved statistically (P<0.01). The keratometric cylinder value decreased by 40.1%, but analysis of KP90 and KP135 polar values did not show any decrease that could be statistically confirmed (P=0.22 and P=0.24). No significant changes were detected in root mean square of total (P=0.61) and HOAs (P=0.13) aberrations. LRIs did not induce alteration in central corneal power confirming a 1:1 coupling ratio.
Conclusion
LRIs determined a nonsignificant alteration of corneal HOA. Therefore, LRIs can be still considered a qualitatively viable mean in those cases where toric intraocular lenses are contraindicated or not available. Yet, the authors raise the question of nonpersonalized nomograms, as in the present study, LRIs did not reach the preset target cylinder.
Introduction
At the time of cataract surgery, astigmatism can be corrected combining incisional techniques, such as limbal relaxing incisions (LRIs) with conventional intraocular lenses (IOLs), or directly implanting a toric IOL. Both methods present strengths and weaknesses. LRIs are a relatively safe and inexpensive procedure inducing low amount of irregularity on corneal topographies, as well as minor glare and patient discomfort.Citation1–Citation4 However, we know that LRIs are surgeon-dependent and result in some degree of variability and unpredictability, which causes an increase in higher-order aberrations (HOAs) and,Citation5 occasionally, in dry eye and healing problems.Citation6 On the other hand, toric IOLs are precise, predictable, and reliable, while requiring specialized surgical skills.Citation7–Citation9 Indeed, toric IOL effective correction of astigmatism relies on performing accurate keratometry and on the mastery of a perfect insertion technique, thus avoiding any postoperative (postop) rotation, even though rotations may be independently induced by postop capsular bag shrinkage.Citation10
Although several studies report that toric IOLs have advantages in comparison to LRIs in terms of astigmatism correction,Citation11–Citation24 we wanted to assess the final changes in corneal wavefront aberration caused by an LRI after cataract surgery through direct comparison before and after surgery on a single patient. The main objective of this study was to determine whether conventional LRIs using a diamond knife have an impact on corneal HOA and therefore on visual optical quality.
Materials and methods
Patients
This prospective, cumulative, interventional, nonrandomized, case study included astigmatic patients undergoing cataract surgery with IOL implantation between October 2011 and February 2012. An informed consent form in accordance with the Helsinki Declaration was obtained from each patient. The institutional review board and the ethics committee of Ospedale Fatebenefratelli e Oftalmico, Milan, Italy, approved the study. Inclusion criteria were patients with cataract and Lens Opacity Classification System III severity of NO1, C1, P1, or more;Citation25 keratometric (K) astigmatism greater than 0.5 diopters (D); and no other ocular comorbidity that might influence visual outcome. Exclusion criteria were patients with active ocular diseases, significant level of corneal HOA exceeding 0.350 µm, using the Zernike polynomials from the topography map (OPD-Scan II; Nidek Co., Ltd., Gamagori, Japan), and a high irregular astigmatism index (>0.54). Irregular astigmatism index is the result of average sum of interring area-corrected dioptric variations along every semimeridian for the whole analyzed surface and normalized by average corneal power (ACP) and the number of all measured points. It describes the short-range semimeridional fluctuation of power distribution and increases along with local irregular corneal astigmatism.
Limbal relaxing incisions calculation
Length and number of LRIs were calculated on a web site (http://www.lricalculator.com, last accessed February 25, 2012) in order to obtain the minimum value of residual astigmatism. This calculator employs Donnenfeld nomogram (DONO) and automatically takes into account the vector from the phaco incisions. The DONO is rated effective between 0.5 and 3 D of astigmatism. The suggested length for an LRI is 90° (3 clock hours). Each 90° LRI provides approximately 1.5 D of correction. The phaco incision and the LRI should not overlap. K readings, surgically induced astigmatism (SIA), and tunnel location were required. K readings were simulated keratometry (SIM Ks) provided by corneal navigator, a function integrated into OPD-Scan II. SIM Ks values include curvature radii along the steepest and the flattest meridians crossing each other at right angles and corneal refractive powers based in a 3 mm zone centrally on an axial map. A SIA value of 0.20 D and a temporal tunnel location was also introduced (180° for right eyes and 0° for left eyes). In case of a SIA cylinder of 0–0.5 D, the LRI calculator software suggests a 30° phaco incision. The paracentesis is considered astigmatically neutral. In case of astigmatism lower than 0.5 D (including SIA), the software automatically displays a message to avoid LRIs at all.
Surgical technique
All procedures were performed by the same surgeon (AS), under topical anesthesia. Preoperatively and before pupil dilatation, slit-lamp-marking technique was performed with patient sitting in upright position and staring at a distant target at head height using the contralateral eye. The finest slit allowed by the slit-lamp was centered on the corneal apex and rotated to the central axis of the planned incisions, using the slit rotation index. The tip of a 30 gauge needle was used to mark limbus at both ends. The length of LRIs was then marked by a fine-tipped marking pen at the beginning of surgery, using a Mendez ring (Martel Inc., Dover, DE, USA). Based on the procedure described by Langerman,Citation26 after proceeding to the operating room and under the operating microscope, a vertical limbal relaxing wound was created with a guarded micrometer diamond blade (Meyco, Biel-Bienne, Switzerland) by making a 0.5 mm groove inside limbus in clear cornea. The incision depth was standardized at 600 µm. After making a single or paired incision as indicated by the nomogram, a 2.2 mm sutureless temporal clear corneal tunnel was created, avoiding overlapping with LRIs. Coaxial phacoemulsification was subsequently performed with AcrySof IQ SN60WF (Alcon Laboratories, Inc., Fort Worth, TX, USA) implantation. In all cases, the goal was emmetropia. As LRIs approximately have a 1:1 coupling ratio, no change in IOL power was needed. The coupling ratio describes the amount of flattening induced in the incised meridian referring to the steepening occurring 90° away. In case of LRIs, negligible change in sphero-equivalent occurs, thus avoiding any adjusting of IOL power.Citation13
Preoperative (preop) and postop examinations
All patients underwent full ophthalmologic examination preoperatively and postoperatively (after 3 years), including refractive status, uncorrected distance visual acuity (UDVA) and best-corrected distance visual acuities (CDVAs) for distance, slit-lamp examination, tonometry, and funduscopy. Visual data were obtained using logMAR units. Additionally, corneal topography and aberrometry (OPD-Scan II), endothelial cell count (Non-Con Robo SP 6000, Konan Medical Inc., Irvine, CA, USA), corneal thickness (Pentacam® HR, OCULUS, Inc., Lynnwood, WA, USA), biometry (Lenstar LS900®, Haag-Streit AG, Koeniz, Switzerland), and macular optical coherence tomography (HRA2, Heidelberg Engineering GmbH, Heidelberg, Germany) were performed (when preoperatively feasible).
Wavefront and topographic assessments were performed using OPD-Scan II, which converts dynamic skiascopy data points (up to 1,440) into wavefront values, using Zernike polynomials up to eighth order. The OPD-Scan II measures the whole eye wavefront aberration and, through the placido-based corneal topography adoption, directly calculates corneal wavefront aberration. OPD-Scan II has demonstrated similar reproducibility but lower interobserver variability when compared to other wavefront aberrometers.Citation27,Citation28
All tests were performed by an independent observer (GM). Data analysis was performed by one of the authors (GM), upon completion of the data collection.
Outcome measures
On a 3-year follow-up visit, the following changes in corneal parameters were considered: 1) root mean square (RMS) of wave aberration for total Z(n,i)(1≤n≤8), astigmatism Z(2,±1), coma Z(3–5–7,±1), trefoil Z(3–5–7,±2), spherical Z(4–6–8,0), and HOA Z(3≤n≤8) with a 4.0 mm aperture diameter; 2) SIM Ks; 3) keratometric cylinder (CYL); 4) difference between pre-calculated (expected) and postop (obtained) CYL; 5) ACP (ACP is an area-corrected average of corneal power ahead of the entrance pupil and generally equal to K spherical equivalent, except for decentered refractive surgical procedures); 6) surface regularity index (SRI is correlated to potential visual acuity and measures local fluctuations in central corneal power); and 7) standard deviation of corneal power (SDP is calculated from distribution of all corneal powers in a videokeratograph; it is often elevated in all situations involving a wide range of powers occurring in measured topography). Postop UDVA and CDVA were also reported. Since preop and postop CYL presents different axes, comparison between preop versus postop, and expected versus obtained values was carried out using polar value analysis.Citation29
Statistical analysis
Statistical analysis was performed using SPSS Windows software (version 15.0, SPSS Inc., Chicago, IL, USA). A sample size was determined from the data collected by the authors in previous studies. Based on such information, a 95% confidence level, a ±20% precision and a P<0.05 variability, the number of eyes necessary to detect the difference between preop and postop values was 64. Normality of all data samples was assessed using Kolmogorov–Smirnov test. For parametric analysis, a Student’s t-test for paired data was performed for comparisons between preop and postop examinations or expected versus obtained data. Whenever parametric analysis was not feasible, Wilcoxon rank-sum test was performed to assess the significance of difference between preop and postop conditions, or expected versus obtained data. The same level of significance was used for all statistical test (P<0.05).
Results
Out of 55 patients recruited, seven were excluded on account of: central retinal vein occlusion (one patient), concomitant cardiovascular diseases (three patients), no-show on follow-up visits (three patients). Sixty-four eyes of 48 patients (27 female and 21 male) were included in this study. Age ranged from 42 to 92 years (70.6±8.4 years). No perioperative and postop complications occurred.
shows the evolution of corneal aberrations after surgery. At 3 years, no statistical difference was found in terms of RMS of total aberrations Z(n,i)(1≤n≤8) (P=0.61) which decreased mainly due to reduction in astigmatism Z(2,±1) (P=0.10). No significant changes were found in the RMS value of HOA Z(3≤n≤8) (P=0.13) except for the trefoil Z(3,±2), which showed a significant increase (P=0.004).
Table 1 Corneal wavefront aberrations with a 4.0 mm aperture diameter over time. Corresponding two-tailed P-values for the comparison between the visits are shown for each parameter
In , the visual and refractive data are reported. UDVA and CDVA improved statistically (P<0.01). CYL value decreased by 40.1%. Analysis of KP90 and KP135 polar values did not show a statistical decrease (P=0.22 and P=0.24, Wilcoxon rank-sum test). The target CYL was not reached, as confirmed by the analysis of the difference between expected and obtained CYL (P<0.01, Wilcoxon rank-sum test).
Table 2 Change in visual and refractive data over time. Corresponding two-tailed P-values for the comparison between the visits are shown for each parameter
LRIs did not induce alteration and fluctuations in central corneal power (ACP, SDP, and SRI).
Discussion
At the time of cataract surgery, astigmatism can be corrected using incisional techniques, such as LRIs. Yet, little is known about the outcomes of corneal aberrations after surgery.
The aim of this study was to assess long-term changes induced by LRIs on HOA and corneal optical quality.
Three years after procedure, as shown in , no significant differences were found in terms of the RMS value of HOA between preop and postcorneal aberrations (). Such a result contrasts sharply with the conclusions of a previous report by Montés-Micó et al where the authors found that astigmatic keratotomy (AK) increased HOA, both coma-like and spherical-like, in a population of patients treated for high myopic astigmatism.Citation5 This could confirm that LRIs are more conservative than astigmatic keratotomy in terms of aberrations, however, probably less effective. Indeed, in our study, only one value showed a significant increase: the trefoil. This figure could relate to the findings of Denoyer et al showing how corneal trefoil increases along with size of incision during cataract surgery.Citation30 Finally, it can be assumed that if an incisional procedure, such as LRIs, is added during phacoemulsification surgery, third-order aberrations in cornea are only partially affected. If the unaltered indices of corneal irregularities – such as SRI and SDP – are taken into account, it may be assumed that LRIs can be considered safe, thus not causing significant irregularities in corneal morphology.
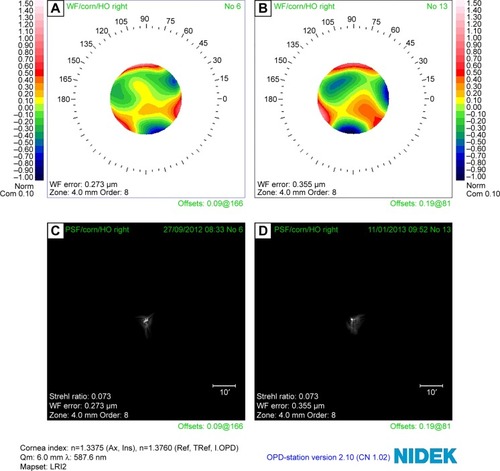
Figure 1 Trend of higher-order aberrations over time.
Abbreviations: corn, cornea; HO, higher-order; WF, wavefront.
Total wavefront aberrations decreased mainly due to reduced astigmatism (). The result has been confirmed by refractive data, as shown in . CYL value decreased to a mean value of 40.1%, comparable to the one reported in literature by several authors. Budak et al reported an absolute decrease in mean astigmatism by 44%,Citation31 Bayramlar et al 52%,Citation32 Kaufmann et al 25%,Citation33 Carvalho et al 50%,Citation34 and Kim et al 32%.Citation35 However, analysis of KP90 and KP135 polar values did not show, in our study, a significant reduction. Target postop CYL was not reached, as confirmed by the analysis of the difference between expected and obtained CYL. Only Sharma et al reported positive results using DONO.Citation36 We think that the nomograms proposed in the literature, including the one we used, are not able to thoroughly account for and correct all the tissue factors influencing the results. Personalized nomograms probably are not a viable solution because they are not exact and are far too dependent on the surgeon’s specific medical expertise, thus proving counterproductive. These limitations should be improved by femtosecond laser, even if recent reports disagree, probably because the technique involves the same biologic aspects.Citation37,Citation38
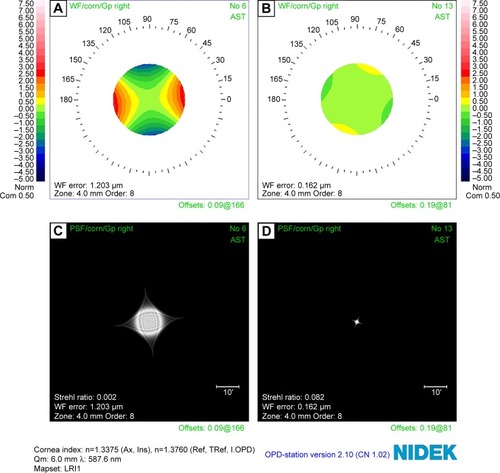
Figure 2 Trend of astigmatism aberration over time.
Abbreviations: corn, cornea; WF, wavefront.
Average central corneal power was not significantly modified by LRIs, thus confirming the value of the coupling ratio of approximately 1:1 previously published. To our knowledge, this is the first report using ACP to confirm such a coupling ratio. Previously, Lindstrom found a 1:1 coupling ratio when a straight 3 mm keratotomy or a 45°–90° arcuate keratotomy incision is performed, thus showing that coupling ratio depends on the length, location, and depth of incision.Citation13 Thornton stated that a true 1:1 coupling ratio can only occur when corneal incisions act as an added tissue but at the same time, corneal circumference is not changed; the latter result is achieved only in case of short, concentric, and arcuate incisions.Citation39
The authors are aware that the present study is limited by data resulting from a 3-year assessment. This means that they cannot rule out the possibility that part of the LRI effect could be due to surgical regression. Yet, the aim of this study was to assess the final outcome, not the evolution in time.
Conclusion
Our study demonstrated that LRIs during cataract surgery do not induce significant changes in corneal HOA. For this reason, though the variability of refractive correction is still a major drawback, LRIs can still be considered a safe and viable means to correct astigmatism in those cases where toric IOLs are contraindicated or not available.
Disclosure
The authors report no conflicts of interest in this work.
References
- NichaminLDAstigmatism controlOphthalmol Clin North Am200619448549317067903
- GillsJPVan Der KarrMCherchioMCombined toric intraocular lens implantation and relaxing incisions to reduce high pre-existing astigmatismJ Cataract Refract Surg2002281585158812231316
- BudakKFriedmanNJKochDDLimbal relaxing incisions with cataract surgeryJ Cataract Refract Surg1998245035089584246
- Müller-JensenKFischerPSiepeULimbal relaxing incisions to correct astigmatism in clear corneal cataract surgeryJ Refract Surg19991558658910504084
- Montés-MicóRMunozGAlbarran-DiegoCRodriguez-GalieteroAAliòJLCorneal aberrations after astigmatic keratotomy combined with laser in situ keratomileusisJ Cataract Refract Surg2004301418142415210217
- NichaminLDChanging approach to astigmatism management during phacoemulsification: Peripheral arcuate astigmatic relaxing incisionsPresented at: The Annual Meeting of the American Society of Cataract and Refractive Surgery2000Boston, MA
- MiyakeTKamiyaKAmanoRIidaYTsunehiroSShimizuKLong-term clinical outcomes of toric intraocular lens implantation in cataract cases with preexisting astigmatismJ Cataract Refract Surg2014401654166025149554
- ScialdoneARaimondiGMonacoGIn vivo assessment of higher-order aberrations after Acrysof toric intraocular lens implantation: a comparative studyEur J Ophthalmol201222453154022139617
- HayashiKkondoHYoshidaMManabeSHirataAHigher-order aberrations and visual function in pseudophakic eyes with a toric intraocular lensJ Cataract Refract Surg2012381156116522608030
- GrabowHBEarly results with foldable toric IOL implantationEur J Implant Refract Surg19946177178
- KohnenTKochDDMethods to control astigmatism in cataract surgeryCurr Opin Ophthalmol199671758010160441
- BuzardKHaightDTroutmanRRuiz procedure for postkeratoplasty astigmatismJ Refract Surg198734045
- LindstromRLThe surgical correction of astigmatism: a clinician’s perspectiveRefract Corneal Surg1990664414542076422
- TadrosAHabibMTejwaniDVon LanyHThomasPOpposite clear corneal incisions on the steep meridian in phacoemulsification: early effects on the corneaJ Cataract Refract Surg20043041441715030833
- GillsJPGaytonJLCataract Surgery: The State of the ArtThorofare, NJSlack Inc19985366
- KershnerRMSurgical Treatment of AstigmatismThorofare, NJSlack Inc1994143155
- GrabowHBRefractive Keratotomy for Cataract Surgery and the Correction of AstigmatismThorofare, NJSlack Inc199479115
- KershnerRMToric lenses for correcting astigmatism in 130 eyesOphthalmology20001071776178210964844
- MaloneyWFSandersDRPearcyDEAstigmatic keratotomy to correct preexisting astigmatism in cataract patientsJ Cataract Refract Surg1990162973042355314
- OsherRHContemporary Refractive Surgery Ophthalmology Clinics of North AmericaPhiladelphia, PAW.B. Saunders1992717725
- BuzardKALaranjeiraEFundingslandBRClinical results of arcuate incisions to correct astigmatismJ Cataract Refract Surg1996224364408733846
- GillsJPFenzlREAnalysis of astigmatic keratotomy with a 5.0-mm optical clear zoneAm J Ophthalmol19961217317328644827
- NichaminLDWallaceRBRefractive Cataract Surgery and Multifocal IOLsThorofare, NJSlack Inc2001167172
- ShepherdJRCorrection of preexisting astigmatism at the time of small incision cataract surgeryJ Cataract Refract Surg19891555572921734
- ChylackLTJrWolfeJKSingerDMThe lens opacities classification system III. The longitudinal study of Cataract Study GroupArch Ophthalmol199311168318368512486
- LangermanDWArchitectural design of a self-sealing corneal tunnel, single-hinge incisionJ Cataract Refract Surg19942084888133489
- BartschDUBesshoKGomezLFreemanWRComparison of laser ray-tracing and skiascopic ocular wavefront-sensing devicesEye200822111384139017571088
- VisserNBerendschotTTVerbakelFTanANde BrabanderJNuijtsRMEvaluation of the comparability and repeatability of four wavefront aberrometersInvest Ophthalmol Vis Sci20115231302131121051697
- NaeserKHjortdalJOMultivariate analysis of refractive data: mathematics and statistic of spherocylindersJ Cataract Refract Surg20012712914211165863
- DenoyerARicaudXVan WentCLabbéABaudouinCInfluence of corneal biomechanical properties on surgically induced astigmatism in cataract surgeryJ Cataract Refract Surg20133981204121023756347
- BudakKYılmazGAslanBSDumanSLimbal relaxing incisions in congenital astigmatism: 6 month follow-upJ Cataract Refract Surg20012771571911377902
- BayramlarHHDağlioğluMCBorazanMLimbal relaxing incisions for primary mixed astigmatism and mixed astigmatism after cataract surgeryJ Cataract Refract Surg20032972372812686239
- KaufmannCPeterJOoiKPhippsSCooperPGogginMLimbal relaxing incisions versus on-axis incisions to reduce corneal astigmatism at the time of cataract surgeryJ Cataract Refract Surg2005312261226516473215
- CarvalhoMJSuzukiSHFreitasLLBrancoBCSchorPLimaALLimbal relaxing incisions to correct corneal astigmatism during phacoemulsificationJ Refract Surg20072349950417523513
- KimDHWeeWRLeeJHKimMKThe short term effects of a single limbal relaxing incision combined with clear corneal incisionKorean J Ophthalmol2010242788220379456
- SharmaBRKumarAPreliminary experiences with limbal relaxing incision for treatment of astigmatism during phacoemulslficationNepal J Ophthalmol200912909421140999
- VenterJBlumenfeldRSchallhornSPelouskovaMNon-penetrating femtosecond laser astigmatic keratotomy in patients with mixed astigmatism after previous refractive surgeryJ Refract Surg201329318018623446014
- ChanTCChengGPWangZThamCCWooVCJhanjiVVector analysis of cornea astigmatism after combined femtosecond-assisted phacoemulsification and arcuate keratotomyAm J Ophthalmol2015160225025525982969
- ThorntonSPSutureless Cataract SurgeryThorofare, NJSlack Inc1992123143
