Abstract
Orthokeratology (ortho-k) is a special rigid contact lens worn at night to achieve myopic reduction and control. This review provides an overview on prescribing ortho-k, including clinical consideration on patient aspect and lens design; its clinical outcomes; and clinical efficacy and safety. Patient satisfaction was summarized. In order to achieve long-term healthy ortho-k treatment, it requires both patient and practitioners’ care and rapport to maintain good ocular health and lens conditions.
Introduction
There is an increasing clinical interest in myopic progression in children. In addition, scientific interest in various myopic control methods has also been strong. In recent years, orthokeratology (ortho-k) treatment has become a clinically acceptable and effective method. The treatment involves a special curved lens fitted to mold the corneal contour in order to achieve myopic reduction and has also resulted in myopic retardation. Clinicians are required to refine the technique and remain up to date in this field.
This review provides an overview of ortho-k, clinical considerations, and outcomes for different forms of ametropia, as well as clinical efficacy and safety. Ortho-k treatment is long term and requires patient care and rapport to monitor ocular health and lens conditions.
Overview of ortho-k
An initial study on corneal reshaping, or ortho-k, was reported in the 1950s, but the clinical term “ortho-k” was not introduced until 1962. Kerns carried out the first large-scale clinical studies to investigate the safety and efficacy of ortho-k.Citation1–Citation8 However, he admitted that the change in refractive errors was unpredictable. Initially, ortho-k was a corneal molding procedure that involved wearing a rigid gas permeable lens.Citation9–Citation12 The myopic reduction was ~1.00 D,Citation1,Citation2,Citation7,Citation10,Citation13 but the progress of myopic reduction was slow, and the procedures involved a series of lenses with different back optic zone radii (BOZR). A breakthrough in ortho-k was achieved when high gas permeable materials and computerized corneal topographers were introduced.Citation14,Citation15 The lens was modified for “accelerated ortho-k,” which achieved faster responses and up to 5.00 D in myopic reduction. This meant that the reduction effect can be achieved within the first month of lens wear.Citation12,Citation16,Citation17
A conventional rigid gas permeable lens is a bicurved lens that has a BOZR and a peripheral curve. A basic standard ortho-k lens, or reverse geometry lens, has three curves, from center to periphery: a BOZR, a reverse curve, and a peripheral curve. The reverse curve assists the corneal molding effect. In order to improve lens centration, the lens is further modified to multicurve design. An alignment curve is introduced and incorporated between the reverse curve and the peripheral curve. This alignment curve may also be divided into two curves (AC1 and AC2) to form a five-zone lens.
This combination of different curves controls the lens sag height to create a molding effect. Adjusting the BOZR alone does not affect the lens fitting. Induced corneal changes are dependent on the combination of the BOZR and the used reverse curve, that is, overall lens sag.
In closed eye condition, the tear layer under the lens sag creates both a positive force and a negative force on the cornea to change the efficacy of treatment. The positive force is exerted to flatten the central cornea, and the negative force is extracted against the mid-peripheral cornea. With these two forces, the epithelial cells are driven from center to mid-peripheral cornea, resulting in a negative epithelial lenticule to reduce the myopia. The zone of the reverse curves is a relief area for tissue redistribution.Citation12
The lens centration is determined by using the alignment curve where the lens is landed on the peripheral cornea. The tear exchange is maintained by adequate edge lift under the peripheral curve.Citation12
In contact lens assessment with the application of fluorescein, an ortho-k lens shows bearing at the corneal apex because the thickness of tear layer is ~5 µm.Citation18 Bearing is also found at the alignment curve because no tears exist when the alignment curve aligns the peripheral cornea. The thickness of tear layer is maximal at the BOZR/reverse curve junction. Any tear layer thickness >20 µm is visible in green when fluorescein is applied.Citation18
Clinical considerations
Ortho-k was originally prescribed for adults to reduce myopia. As a myopic control effect was found in many studies, it is now mainly prescribed for children. In order to enhance the efficacy and safety of ortho-k, practitioners should consider the following factors before prescribing the lens.
Basic patient criteria
Many studies have been conducted with children at the age of 7 years,Citation16,Citation19–Citation26 and some schools/colleges of optometry have reported age recommendations for myopia treatment with ortho-k in children as young as 5–6 years.Citation27 However, ortho-k treatment depends more on the maturity level of the patient rather than on age. In addition to patient maturity level, practitioners should also consider the level of parent participation.Citation27
Parents should help their children in monitoring lens insertion and removal, as well as lens usage and care.Citation28 Incomplete instructions or deviation from the procedures will lead to lens contamination. Moreover, parental support applies also to aftercare visits, in which practitioners will evaluate ocular health and refractive change.Citation29 Both the parties will discuss and agree on a solution if any abnormality is found.
Cho et al recommended that informed consent should be obtained from the patient, his/her parents, and practitioners.Citation29 Both the patient and his/her parents should be informed about potential effects, patient alternatives, and the importance of compliance. Practitioners should provide an emergency contact number for any serious issues. The three parties share equal responsibility for good, long-term clinical care under ortho-k treatment. As with any kind of medical treatment, a good rapport is also required.
Baseline refraction errors
Most studies reported patients with mild-to-moderate myopia (−0.75 D to −5.00 D) and low astigmatism (up to 1.50 D) as good candidates for ortho-k treatment. This is because ~90% of myopia and 50% of astigmatism have been corrected under these conditions.Citation16,Citation19–Citation26,Citation30,Citation31 Several studies have reported that toric ortho-k could reduce astigmatism up to −3.00 D,Citation21,Citation32–Citation34 and scattered cases have reported full correction for high myopia (myopia >6.00 D).Citation24 However, these studies included no details on ocular health after lens wear. Clinically, practitioners may use a series of ortho-k lenses to correct high myopia.
Corneal profile
Keratometers can measure only up to 3 mm and cannot reflect the true corneal profile after ortho-k treatment. Therefore, corneal topography is crucial in prescribing ortho-k because it helps in screening out unqualified patients who show a decentered corneal apex, keratoconus, or irregular corneas.Citation35–Citation37 Topography should be accurate and repeatableCitation35,Citation36 and should provide various maps including axial (for corneal power), tangential (for corneal shape), refractive, and curvature maps in different adjustable scales.Citation37 Practitioners must measure the corneal profile in every aftercare visit to monitor any subtle changes in corneal curvature.
During the initial assessment, both the axial and tangential power maps are used to check for any corneal asymmetry or abnormality. Once ortho-k is fitted, the cornea will be molded, and the molding response is always compared with the baseline topography. The subtraction map function is essential to evaluate topographical changes and the lens–corneal relationship. The common ortho-k responses include bull’s eye, central island (central curvature steepens than periphery), frowny face (lens decenters down), and smiley face (lens decenters up). With any undesirable responses, practitioners should amend the lens fitting accordingly.
Apart from screening out unsuitable patients, corneal astigmatism is judged by the corneal profile. Baseline corneal astigmatism was suggested to be <1.50 D in the previous studiesCitation30 until toric ortho-k was introduced to correct up to −3.00 D astigmatism.Citation32,Citation33,Citation38,Citation39 Clinically, good centration and a reduction effect are found when the refraction astigmatism is in line with the corneal astigmatism, in terms of diopter and axis, to prevent residual astigmatism. Any against-the-rule or limbus-to-limbus corneal astigmatism may affect lens centration.
Horizontal visual iris diameter (HVID) and pupil diameter HVID is used to determine the lens diameters and can be measured by a ruler, by adjustable slit size on a slit lamp, or based on a corneal topographical map. Some lens manufacturers suggest that the lens size should cover 95% of the HVID at most as lateral decentration may occur in a smaller lens.
Pupil diameter should be measured under both photopic and scotopic environments. If the treatment zone is smaller than the pupil size, then the patients may experience flare and glare, especially in dim light. According to Munnerlyn’s formula, the more the myopic reduction using ortho-k, the smaller the treatment zone size.Citation40 van der Worp and Ruston suggested that the treatment zone should be 3.5 mm with changes in corneal thickness of 20 µm and myopic reduction of 4.90 D.Citation41
Eyelid features
Loose eyelids may not exert enough force, whereas tight eyelids may exert too much force on the ortho-k lens in closed eye condition. As this is difficult to measure clinically, an overnight trial is essential to assess topographical responses.Citation37
Lens design consideration
A spherical or toric ortho-k lens is prescribed based on corneal profile and refractive errors. A spherical lens can only correct slight astigmatism.Citation16,Citation30 When corneal astigmatism is ≥1.50 D, fitting a spherical lens leads to induced astigmatism or lens decentration and results in poor vision. A toric lens is suggested under these conditions.Citation21,Citation34,Citation39 Only the reverse, alignment, and/or peripheral curves are toric to enhance the centration of lens fit.
Practitioners can use computer software to generate a new lens or select an initial lens from a set of trial lenses.Citation21,Citation34 Some computer software uses patient information including spectacle prescription, HVID, and corneal sagittal height data to determine the ortho-k lens parameter. Practitioners may be allowed to adjust the lens parameters by using the software to estimate the lens fit. Some manufacturers provide a diagnostic lens set so that practitioners can evaluate fit in-office. The first lens from the diagnostic lens set can be selected according to the flat K, eccentricity, and/or manufacturer’s fitting guide.
When practitioners receive the diagnostic lenses, both static and dynamic assessments of contact lens fitting are suggested to eliminate major size discrepancies. However, fluorescence can only be seen with the naked eye if the tear layer is >20 µm,Citation18,Citation42 and therefore, it is difficult to assess lens performance in-office. Overnight topographical response is the most valid procedure for evaluating lens fit. It determines the centration of the lens and the physiological response to the treatment while also monitoring changes, assisting with problem-solving, and refining the lens fit.
Ortho-k effect on different forms of ametropia
Myopia
A myopic ortho-k effect results from a central corneal flattening and a paracentral corneal steepening. Studies have indicated that ~80% reduction would be resulted if the baseline myopia is <5.00 D. The most significant reduction occurs after the first overnight wear (~60%) and keeps down steady for the next week. The reduction rate levels off after 1 month of lens wear.Citation19,Citation21,Citation22,Citation24–Citation26,Citation43
Hyperopia
A hyperopic ortho-k effect results from a central corneal steepening and a paracentral corneal flattening. Several short-term pilot studies have shown hyperopic reduction after 1 h and an increased effect with longer lens wear. According to Gifford et al, “A good (hyperopic) lens fit must exhibit central clearance over the optical zone and progress to mid-peripheral touch while maintaining adequate edge lift.”Citation44,Citation45 However, there are limited studies on the corneal effect and clinical assessment on hyperopic ortho-k.
Astigmatism
Astigmatism correction has been reported at 50% of with-the-rule astigmatism when the corneal cylinder is <1.50 D. However, additional case studies have shown more promising results by using toric ortho-k to correct astigmatism.Citation21,Citation32–Citation34,Citation38 Chen et al reported 80% reduction on astigmatism in 6 months by using toric ortho-k.Citation21 In their study, the astigmatism was decreased from −1.86±0.64 D to −0.37±0.39 D in 6 months. The reduction was maintained throughout a 2-year study.
Corneal thickness changes
In myopia reduction, previous studies have shown a change in corneal thickness at the epithelium (thinning at the central epithelium, but thickening at the mid-peripheral epithelium).Citation46–Citation48 In hyperopic ortho-k, the central epithelium remains the same, whereas the mid-peripheral epithelium was thinned by 15% after 8 h of lens wear. However, more detailed studies are required to investigate the progress of refractive changes and corneal thickness changes in the hyperopic ortho-k effect.Citation45,Citation49
Daytime regression in myopic ortho-k effect
Mountford found that the regression of refractive errors was ~0.50–0.75 D after 8 h of lens removal in Caucasians,Citation50 but he did not find a correlation between refractive change and regression. Gardiner et al further traced the refractive errors changed after lens removal.Citation51 The subjects in their study wore ortho-k for 6 h. They traced the refractive changes in every 5 h. The regressions were 0.39 D and 0.60 D after 6 h and 15 h of lens removal, respectively. They suggested a correlation between baseline myopia and the total regression. Chan et al reported that the daytime regression in refractive errors was insignificant in Chinese, and they did not find the correlation.Citation16 They commented that the regression was unpredictable, which may not be reflected by objective refractive and topographic responses.
Clinical efficacy of ortho-k
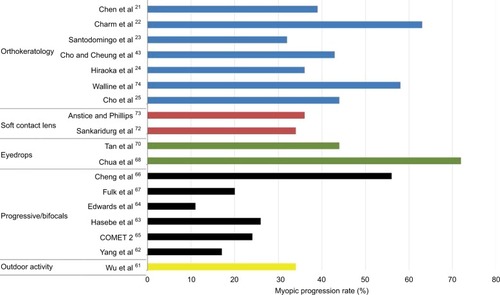
Myopia increases with the elongation of axial length. Hence, a correlation between the axial elongation and visual feedback is suggested. A normal cornea is steepened centrally and gradually flattens to the periphery. Light will be focused at the macula, and it is behind the retina at the periphery (peripheral hyperopia). Studies found that the relative periphery hyperopia is greater in myopes than in emmetropes or hyperopes.Citation52–Citation56 It was proposed that the peripheral hyperopic defocus may promote axial myopia.Citation52–Citation56 The corneal shape was changed after ortho-k treatment. The central cornea flattening and mid-periphery steepening reduce the relative peripheral hyperopia in myopic eyes. This is considered a potent myopia-inhibiting indicator.Citation57–Citation60 Recent randomized myopic control studies have indicated that ortho-k retards myopic progression in low myopes, high myopes, and astigmatic patients (). The retardation rate was comparable to those using atropine, but it was higher than in those wearing special soft contact lenses and progressive/bifocal glasses.Citation21–Citation25,Citation43,Citation61–Citation75
Ortho-k on high myopes
Most commercially available ortho-k lenses and those used in published reports are limited to moderate myopes (~5.00 D) only. Several reports were suggested that visual acuities were good on high myopes after ortho-k treatment,Citation76 and they did not present details on ocular health condition after lens wear. Clinically, when the lens target is increased to ≥5.00 D, significant corneal staining and lens decentration are found.Citation31,Citation77 A cautious ortho-k treatment on high myopes was introduced.Citation22 A certain amount of myopia was reduced by using ortho-k (partial reduction [PR]), and the remaining refractive errors were corrected by spectacles. In a high myopia study,Citation22 the high myopes (myopia of ≥5.75) were randomly enrolled in study (PR with ortho-k and spectacles) and control (correction with spectacles only) groups. In the study group, ortho-k lens was fitted to reduce 4.00 D myopia, whereas a pair of single-vision spectacles was prescribed to correct any remaining refractive errors. In the control group, only a pair of single-vision spectacles was prescribed. The myopic progression and axial lengths were monitored for 2 years. The axial lengths were 0.19±0.21 mm and 0.51±0.32 mm in the study and control groups, respectively. The results suggest that myopic reduction and control would also be achieved for high myopes by using ortho-k and spectacles.
Safety
Liu et al investigated the safety of ortho-k by reviewing 170 publications.Citation78 It was concluded that corneal staining was the most typical complication. Chan et al reported that the incidence and severity of corneal staining increased with ortho-k wear.Citation16 When lens binding occurred, central corneal staining was the result. Chan et al suggested to use fenestrated lenses or to ask the patients to instill artificial tears before lens removal in order to minimize the severity of the lens binding.Citation16,Citation79 It has been suggested that central corneal staining is common, and practitioners should monitor the patients carefully.
Some microbial keratitis (MK) cases have been reported with ortho-k treatment.Citation80–Citation82 Underlying risk factors include inadequate training of practitioners and wearers, poor lens handling, poor patient compliance, and inadequate follow-up. A recent review indicated a drop in ortho-k-related MK.Citation83 Bullimore et al estimated the incidence of MK in children at the rate of 13.9 in 10,000 patients, which is similar to the risk with overnight contact lens wear.Citation84 Hence, practitioners should provide clear instructions and regular follow-up to make sure good lens care and compliance in ortho-k treatment to minimize complications. It is also important to provide up-to-date training courses by schools/colleges of optometry worldwide.Citation27
Pigmented iron depositsCitation85–Citation87 and fibrillary linesCitation88,Citation89 have been reported in long-term ortho-k wear. Intensity increased with the continuance of ortho-k wear, but both will disappear after the termination of the treatment.
Patient perspectives
Ortho-k reshapes the corneal profile and changes the optical quality of the cornea. The higher-order aberrations were increased significantly after ortho-k treatment.Citation90–Citation92 Although most studies showed comparable visual acuity in high contrast between pre- and post-ortho-k treatment, contrast sensitivity was reduced.Citation93 Common complaints were halos and glare perceived in dim light. Undesired visual anomalies are expected to disappear after the first weeks of treatment,Citation94 and it has been hypothesized that the increase in light distortion is a short-term condition that improves when the subject adapts.Citation95
Cho et alCitation77 and Chan et alCitation16 conducted interviews with 61 and 94 ortho-k patients, respectively. More than 70%Citation77 and 90%Citation16 of the subjects ranked “good” or “very good” unaided distance vision after lens wear. Those with high baseline myopia reported worsened distance vision toward the end of the day. Hiraoka et al confirmed that patients with higher baseline myopia were likely to report lower levels of satisfaction and that post-ortho-k unaided visual acuity was associated with patient satisfaction.Citation96 When the patients did not wear ortho-k every night, the vision quality varied. Patients who wore the lens every night reported higher satisfaction than those who reported skipping at least one night of lens wear.Citation97
Santodomingo et al delivered questionnaires to evaluate the satisfactions between ortho-k-wearing and spectacle-wearing groups.Citation98 Children wearing ortho-k lenses were more satisfied than those wearing spectacles in terms of overall vision, appearance, academic performance, and peer perception. The guardians of children under ortho-k group preferred that they continue wearing ortho-k.
Conclusion
The ultimate clinical goals were full myopic reduction, good myopic control, and good ocular health. Sufficient evidence was found that ortho-k is a clinically safe option for myopic reduction and myopic control. However, center lens fitting (centered topographical response) is only a starting point. Long-term healthy treatment requires combined efforts from practitioners, parents, and children.
Disclosure
The author reports no conflicts of interest in this work.
References
- KernsRLResearch in orthokeratology. Part I: introduction and backgroundJ Am Optom Assoc1976478104710511021577
- KernsRLResearch in orthokeratology. Part II: experimental design, protocol and methodJ Am Optom Assoc19764710127512851022795
- KernsRLResearch in orthokeratology. Part III: results and observationsJ Am Optom Assoc19764712150515151027768
- KernsRLResearch in orthokeratology. Part VII: examination of techniques, procedures and controlJ Am Optom Assoc1977481215411553599249
- KernsRLResearch in orthokeratologyPart VI: statistical and clinical analysesJ Am Optom Assoc197748911341147903556
- KernsRLResearch in orthokeratology. Part V: results and observations–recovery aspectsJ Am Optom Assoc1977483345359864189
- KernsRLResearch in orthokeratology. Part IV: results and observationsJ Am Optom Assoc1977482227238853211
- KernsRLResearch in orthokeratology. Part VIII: results, conclusions and discussion of techniquesJ Am Optom Assoc1978493308314348745
- PolseKAOrthokeratology as a clinical procedureAm J Optom Physiol Opt1977546345346907023
- CoonLJOrthokeratology: part I historical perspectiveJ Am Optom Assoc19825331871957042802
- EfronNOvernight orthokeratologyOptom Vis Sci2000771262762911147730
- SwarbrickHAOrthokeratology review and updateClin Exp Optom200689312414316637967
- BinderPSMayCHGrantSCAn evaluation of orthokeratologyOphthalmology19808787297447443201
- LuiWOEdwardsMHChoPContact lenses in myopia reduction – from orthofocus to accelerated orthokeratologyCont Lens Anterior Eye2000233687616303435
- NicholsJJMarsichMMNguyenMBarrJTBullimoreMAOvernight orthokeratologyOptom Vis Sci200077525225910831215
- ChanBChoPCheungSWOrthokeratology practice in children in a university clinic in Hong KongClin Exp Optom200891545346018355342
- ChanBChoPMountfordJRelationship between corneal topographical changes and subjective myopic reduction in overnight orthokeratology: a retrospective studyClin Exp Optom201093423724220579079
- MountfordJChoPChuiWSIs fluorescein pattern analysis a valid method of assessing the accuracy of reverse geometry lenses for ortho-keratology?Clin Exp Optom2005881333815658924
- SwarbrickHAAlharbiAWattKLumEKangPMyopia control during orthokeratology lens wear in children using a novel study designOphthalmology2015122362063025439432
- RajabiMTHosseiniSSGhorbaniZUtility of orthokeratology contact lenses; efficacy of myopia correction and level of patient satisfaction in Iranian myopic/myope-astigmatic patientsJ Curr Ophthalmol2015273–49910227239586
- ChenCCheungSWChoPMyopia control using toric orthokeratology (TO-SEE study)Invest Ophthalmol Vis Sci201354106510651724003088
- CharmJChoPHigh myopia-partial reduction ortho-k: a 2-year randomized studyOptom Vis Sci201390653053923645372
- Santodomingo-RubidoJVilla-CollarCGilmartinBGutierrez-OrtegaRMyopia control with orthokeratology contact lenses in Spain: refractive and biometric changesInvest Ophthalmol Vis Sci20125385060506522729437
- HiraokaTKakitaTOkamotoFTakahashiHOshikaTLong-term effect of overnight orthokeratology on axial length elongation in childhood myopia: a 5-year follow-up studyInvest Ophthalmol Vis Sci20125373913391922577080
- ChoPCheungSWEdwardsMThe longitudinal orthokeratology research in children (LORIC) in Hong Kong: a pilot study on refractive changes and myopic controlCurr Eye Res2005301718015875367
- WallineJJRahMJJonesLAThe Children’s Overnight Orthokeratology Investigation (COOKI) pilot studyOptom Vis Sci200481640741315201713
- ParkerKELeachNEOrthokeratology: an academic perspectiveEye Contact Lens2016421566026595212
- ChoPBoostMChengRNon-compliance and microbial contamination in orthokeratologyOptom Vis Sci200986111227123419786928
- ChoPCheungSWMountfordJWhitePGood clinical practice in orthokeratologyCont Lens Anterior Eye2008311172817714977
- MountfordJPesudovsKAn analysis of the astigmatic changes induced by accelerated orthokeratologyClin Exp Optom200285528429312366349
- ChoPCheungSWEdwardsMHPractice of orthokeratology by a group of contact lens practitioners in Hong Kong. Part 2: orthokeratology lensesClin Exp Optom2003861424612568650
- ChenCChoPToric orthokeratology for high myopic and astigmatic subjects for myopic controlClin Exp Optom201295110310821895768
- ChenCCCheungSWChoPToric orthokeratology for highly astigmatic childrenOptom Vis Sci201289684985522561203
- ChanBChoPde VechtAToric orthokeratology: a case reportClin Exp Optom200992438739119323673
- ChoPLamAKMountfordJNgLThe performance of four different corneal topographers on normal human corneas and its impact on orthokeratology lens fittingOptom Vis Sci200279317518311915858
- ChuiWSChoPA comparative study of the performance of different corneal topographers on children with respect to orthokeratology practiceOptom Vis Sci200582542042715894918
- DaveTCorneal topography and its measurementMountfordJDaveTRustonDOrthokeratology: Principles and PracticeOxfordButterworth-Heinemann20041745
- LuoMMaSLiangNClinical efficacy of toric orthokeratology in myopic adolescent with moderate to high astigmatismEye Sci201429420921321826016072
- PauneJCardonaGQuevedoLToric double tear reservoir contact lens in orthokeratology for astigmatismEye Contact Lens201238424525122735626
- MunnerlynCRKoonsSJMarshallJPhotorefractive keratectomy: a technique for laser refractive surgeryJ Cataract Refract Surg198814146523339547
- van der WorpERustonDOrthokeratology: an updateOiP200674760
- CarneyLGLuminance of fluorescein solutionsAm J Optom Arch Am Acad Optom19724932002044502354
- ChoPCheungSWRetardation of myopia in orthokeratology (ROMIO) study: a 2-year randomized clinical trialInvest Ophthalmol Vis Sci201253117077708522969068
- GiffordPAuVHonBSiuAXuPSwarbrickHAMechanism for corneal reshaping in hyperopic orthokeratologyOptom Vis Sci2009864e306e31119225436
- GiffordPSwarbrickHATime course of corneal topographic changes in the first week of overnight hyperopic orthokeratologyOptom Vis Sci200885121165117119050471
- LiFJiangZXHaoPLiXA meta-analysis of central corneal thickness changes with overnight orthokeratologyEye Contact Lens201642214114625828512
- Nieto-BonaAGonzalez-MesaANieto-BonaMPVilla-CollarCLorente-VelazquezAShort-term effects of overnight orthokeratology on corneal cell morphology and corneal thicknessCornea201130664665421282996
- AlharbiASwarbrickHAThe effects of overnight orthokeratology lens wear on corneal thicknessInvest Ophthalmol Vis Sci20034462518252312766051
- GiffordPAlharbiASwarbrickHACorneal thickness changes in hyperopic orthokeratology measured by optical pachometryInvest Ophthalmol Vis Sci20115263648365321372013
- MountfordJAn analysis of the changes in corneal shape and refractive error induced by accelerated orthokeratologyICLC1997244128144
- GardinerHKLeongMAGundelREQuantifying regression with orthokeratologyContact Lens Spec2005204043 Available from: http://www.clspectrum.com/articleviewer.aspx?articleID=12892Accessed December 20, 2016
- CooperJSchulmanEJamalNCurrent status on the development and treatment of myopiaOptometry201283517919923249121
- KangPGiffordPMcNamaraPWuJYeoSVongBSwarbrickHPeripheral refraction in different ethnicitiesInvest Ophthalmol Vis Sci201051116059606520505193
- TaberneroJOhlendorfAFischerMDBruckmannARSchieferUSchaeffelFPeripheral refraction profiles in subjects with low foveal refractive errorsOptom Vis Sci2011883E388E39421258260
- MuttiDOHayesJRMitchellGLRefractive error, axial length, and relative peripheral refractive error before and after the onset of myopiaInvest Ophthalmol Vis Sci20074862510251917525178
- MuttiDOSinnottLTMitchellGLRelative peripheral refractive error and the risk of onset and progression of myopia in childrenInvest Ophthalmol Vis Sci201152119920520739476
- KangPSwarbrickHTime course of the effects of orthokeratology on peripheral refraction and corneal topographyOphthalmic Physiol Opt201333327728223347397
- KangPSwarbrickHPeripheral refraction in myopic children wearing orthokeratology and gas-permeable lensesOptom Vis Sci201188447648221317669
- QueirosAGonzalez-MeijomeJMJorgeJVilla-CollarCGutierrezARPeripheral refraction in myopic patients after orthokeratologyOptom Vis Sci201087532332920375751
- CharmanWNMountfordJAtchisonDAMarkwellELPeripheral refraction in orthokeratology patientsOptom Vis Sci200683964164816971842
- WuPCTsaiCLWuHLYangYHKuoHKOutdoor activity during class recess reduces myopia onset and progression in school childrenOphthalmology201312051080108523462271
- YangZLanWGeJThe effectiveness of progressive addition lenses on the progression of myopia in Chinese childrenOphthalmic Physiol Opt2009291414819154279
- HasebeSOhtsukiHNonakaTEffect of progressive addition lenses on myopia progression in Japanese children: a prospective, randomized, double-masked, crossover trialInvest Ophthalmol Vis Sci20084972781278918579755
- EdwardsMHLiRWLamCSLewJKYuBSThe Hong Kong progressive lens myopia control study: study design and main findingsInvest Ophthalmol Vis Sci20024392852285812202502
- Correction of Myopia Evaluation Trial 2 Study Group for the Pediatric Eye Disease Investigator GroupProgressive-addition lenses versus single-vision lenses for slowing progression of myopia in children with high accommodative lag and near esophoriaInvest Ophthalmol Vis Sci20115252749275721282579
- ChengDSchmidKLWooGCDrobeBRandomized trial of effect of bifocal and prismatic bifocal spectacles on myopic progression: two-year resultsArch Ophthalmol20101281121920065211
- FulkGWCyertLAParkerDEA randomized trial of the effect of single-vision vs. bifocal lenses on myopia progression in children with esophoriaOptom Vis Sci200077839540110966065
- ChuaWHBalakrishnanVChanYHAtropine for the treatment of childhood myopiaOphthalmology2006113122285229116996612
- ChiaAChuaWHCheungYBAtropine for the treatment of childhood myopia: safety and efficacy of 0.5%, 0.1%, and 0.01% doses (atropine for the treatment of myopia 2)Ophthalmology2012119234735421963266
- TanDTLamDSChuaWHShu-PingDFCrockettRSAsian Pirenzepine Study GroupOne-year multicenter, double-masked, placebo-controlled, parallel safety and efficacy study of 2% pirenzepine ophthalmic gel in children with myopiaOphthalmology20051121849115629825
- SankaridurgPDonovanLVarnasSSpectacle lenses designed to reduce progression of myopia: 12-month resultsOptom Vis Sci201087963164120622703
- SankaridurgPHoldenBSmithE3rdDecrease in rate of myopia progression with a contact lens designed to reduce relative peripheral hyperopia: one-year resultsInvest Ophthalmol Vis Sci201152139362936722039230
- AnsticeNSPhillipsJREffect of dual-focus soft contact lens wear on axial myopia progression in childrenOphthalmology201111861152116121276616
- WallineJJJonesLASinnottLTCorneal reshaping and myopia progressionBr J Ophthalmol20099391181118519416935
- KakitaTHiraokaTOshikaTInfluence of overnight orthokeratology on axial elongation in childhood myopiaInvest Ophthalmol Vis Sci20115252170217421212181
- OguriANishimuraMAdvanced orthokeratology for Japanese patients with high myopiaInvest Ophthalmol Vis Sci200344133290
- ChoPCheungSWEdwardsMHFungJAn assessment of consecutively presenting orthokeratology patients in a Hong Kong based private practiceClin Exp Optom200386533133814558855
- LiuYMXiePThe safety of orthokeratology–a systematic reviewEye Contact Lens2016421354226704136
- CheungSWChoPSubjective and objective assessments of the effect of orthokeratology–a cross-sectional studyCurr Eye Res200428212112714972717
- WattKSwarbrickHAMicrobial keratitis in overnight orthokeratology: review of the first 50 casesEye Contact Lens200531520120816163011
- WattKGBonehamGCSwarbrickHAMicrobial keratitis in orthokeratology: the Australian experienceClin Exp Optom2007903182187 quiz 188–18917425764
- Van MeterWSMuschDCJacobsDSKaufmanSCReinhartWJUdellIJAmerican Academy of OphthalmologySafety of overnight orthokeratology for myopia: a report by the American Academy of OphthalmologyOphthalmology20081151223012313.e118804868
- SongXXuLSunSZhaoJXieLPediatric microbial keratitis: a tertiary hospital studyEur J Ophthalmol201222213614121574163
- BullimoreMASinnottLTJones-JordanLAThe risk of microbial keratitis with overnight corneal reshaping lensesOptom Vis Sci201390993794423892491
- Gonzalez-MeijomeJMGonzalez-PerezJGarcia-PortaNDiaz-ReyAParafita-MatoMAPigmented corneal ring associated with orthokeratology in Caucasians: case reportsClin Exp Optom201295554855222725834
- ChoPChuiWSCheungSWReversibility of corneal pigmented arc associated with orthokeratologyOptom Vis Sci2003801279179514688541
- CheungSWChoPCheungAWhite lesion in the corneal pigmented ring associated with orthokeratologyOphthalmic Physiol Opt200525326426815854075
- LumESwarbrickHFibrillary lines in overnight orthokeratologyClin Exp Optom200790429930217535370
- CheungSWChoPBronAJChuiVChanBCase report: the occurrence of fibrillary lines in overnight orthokeratologyOphthalmic Physiol Opt200626552553116918780
- MaoXJLuFQuJEffects after orthokeratology on corneal topography and monochromic wavefront aberrationZhonghua Yan Ke Za Zhi2004407471473 Chinese15454062
- HiraokaTOkamotoCIshiiYKakitaTOshikaTContrast sensitivity function and ocular higher-order aberrations following overnight orthokeratologyInvest Ophthalmol Vis Sci200748255055617251449
- HiraokaTOkamotoCIshiiYTakahiraTKakitaTOshikaTMesopic contrast sensitivity and ocular higher-order aberrations after overnight orthokeratologyAm J Ophthalmol2008145464565518241829
- HiraokaTOkamotoCIshiiYKakitaTOkamotoFOshikaTTime course of changes in ocular higher-order aberrations and contrast sensitivity after overnight orthokeratologyInvest Ophthalmol Vis Sci200849104314432018502987
- StillitanoISchorPLipenerCHofling-LimaALLong-term follow-up of orthokeratology corneal reshaping using wavefront aberrometry and contrast sensitivityEye Contact Lens200834314014518463478
- Santolaria SanzECervinoAQueirosAVilla-CollarCLopes-FerreiraDGonzalez-MeijomeJMShort-term changes in light distortion in orthokeratology subjectsBiomed Res Int2015201527842525699265
- HiraokaTOkamotoCIshiiYPatient satisfaction and clinical outcomes after overnight orthokeratologyOptom Vis Sci200986787588219543136
- SantolariaECervinoAQueirosABrautasetRGonzalez-MeijomeJMSubjective satisfaction in long-term orthokeratology patientsEye Contact Lens201339638839324172066
- Santodomingo-RubidoJVilla-CollarCGilmartinBGutierrez-OrtegaRMyopia control with orthokeratology contact lenses in Spain: a comparison of vision-related quality-of-life measures between orthokeratology contact lenses and single-vision spectaclesEye Contact Lens201339215315723392299