Abstract
Introduction
Worldwide, amblyopia prevalence among children is in the range of 0.13% to 12.9%. However, there are no known community-based data regarding amblyopia prevalence and its associated factors among school age children in Ethiopia. The aim of this study was to determine the prevalence of amblyopia and to identify factors associated with amblyopia among school age children in Bahir Dar city, northwest Ethiopia.
Methods and Materials
A cross-sectional study among a school age community of Bahir Dar city was conducted from April 1 to May 29, 2018. Data were collected using a pretested structured questionnaire and checklist through interview and physical examination. Bivariable logistic regression was done, and variables with p value <0.2 were entered to multivariable logistic regression using SPSS 20. Variables with p value of <0.05 in the multivariable binary logistic regression were considered as significant predictors.
Results
In total 601 (94.8%) subjects participated. Amblyopia was prevalent in 6.5% of school age children in Bahir Dar city. The odds of being amblyopic among participants who had anisometropia >2D were about 9.3 times (AOR=9.35, CI: 2.86–30.60) more as compared to those who had no anisometropia. The odds of being amblyopic among participants having a refractive error >+5D hypermetropia were about 22 times (AOR=21.77, CI: 7.15–66.34) more as compared to participants who had no hypermetropia.
Conclusion
The prevalence of amblyopia among school age children at Bahir Dar city is higher than the World Health Organization cut point. Having anisometropia greater than 1 diopter, anisometropia >2 diopter, having anisometropia less than 1 diopter, having a history of strabismus, having a hyperopia of > +5 diopter, > +2 diopter, having a positive history of visual deprivation and having a positive history of strabismus in the family were the significant factors positively associated with amblyopia.
Introduction
Amblyopia, a Greek word meaning “blunt or blurry vision”, is defined as a reduction of best corrected visual acuity (BCVA) in one or both eyes caused by form deprivation or abnormal binocular interaction with no pathology in the visual system.Citation1–Citation3 It is a common problem in childrenCitation4 and has a wider range of impacts on childhood and adulthood life of an individual and community at large. Amblyopia has a drastic impact on individuals' academic performance,Citation5 career choice, visuomotor skills, social interaction, psychological development and economic participation.Citation5,Citation6 Children with unilateral amblyopia are also more at risk for a bilateral visual impairment.Citation7 While the prognosis for late treatment initiation is not promising, early treatment can eliminate amblyopia.Citation4 Ocular media opacity,Citation8–Citation10 strabismus,Citation8,Citation9,Citation11–Citation16 anisometropia,Citation13–Citation15,Citation17 hypermetropia, astigmatism,Citation8–Citation15,Citation17 myopia,Citation8,Citation9 blepharoptosisCitation8,Citation10,Citation16 and reduced unaided distance visual acuityCitation8,Citation9,Citation18 are the common risk factors for amblyopia. Civil servant mother at time of child birth,Citation19 mother without formal education,Citation19 birth weight ≤2.50 kg,Citation13,Citation19 child history of past eye complaint,Citation19 child history of past eye surgery,Citation19 history of past spectacle use,Citation19 family history of wearing spectacles,Citation16,Citation19 family history of crossed eyes,Citation19 family history of eye surgery,Citation19 gestational period <37 weeks,Citation13,Citation15,Citation16 admission to NICU,Citation13 maternal smoking during pregnancy,Citation13 child history of seizureCitation16 and being a twinCitation16 are also factors that are positively associated with amblyopia. Worldwide, the prevalence of amblyopia in children was estimated between 0.13% and 12.9%.Citation5,Citation14,Citation19–Citation31
Even though the World Health Organization in its “vision 2020” strategy projected a 1–2% and 3% prevalence of amblyopia among screened and non-screened preschool children, respectively,Citation32,Citation33 there are no known community-based data regarding prevalence of amblyopia and the factors associated with amblyopia among school age children particularly in Ethiopia. The purpose of this study was to determine amblyopia prevalence and to identify factors associated with amblyopia in the community of school age children in Bahir Dar city, northwest Ethiopia.
Methods and Materials
Study Design, Setting and Sampling
A cross-sectional study to determine amblyopia prevalence and to identify factors associated with amblyopia among a school age community of Bahir Dar city was conducted from April 1 to May 29, 2018. Bahir Dar, the capital city of Amhara regional state of Ethiopia, is found 578 km northwest of Addis Ababa, the capital of Ethiopia. An estimated 243,300 people live in Bahir Dar city.Citation34 There were approximately 53,725 households and 86,872 school age children (age range between 6 and 18 years old) living in six administrative sub-cities and 17 kebeles. There are three governmental hospitals, five private health sectors that provide eye-care services in Bahir Dar city.Citation34 All children in the age range of 6–18 years old that were living in the city longer than 6 months were included in this study. However, children with recent eye disorders including severe trauma that affect vision or with recent ocular surgery were excluded from the study. The sample size was calculated by Open Epi software. Because of the absence of community-based data on amblyopia in Ethiopia, 50%, 5, 1.5 and 10% were taken as prevalence, margin of error, design effect and non-response rate, respectively. The calculated sample size was 634. Multistage sampling was used to get the sample. First, the Bahir Dar City Statistical Agency gave us the list of allCitation17 kebeles in the city. Then four kebeles were selected randomly by lottery method of SRS. The total number of households and population in the selected kebeles was 12,015 and 44,438, respectively.Citation35 The household of the participant was selected using a proportionally allocated systematic random sampling technique with a sampling fraction of 19. A lottery method was used to select the participating child when more than one child was eligible for participation in that house. The houses were revisited if the participating child and/or guardians/parents were not present in the house. The next three consecutive households were visited for schoolage children, when there was no school age children in the selected house.
Operational Definitions
Amblyopia: Amblyopia was categorized as “Yes” if a child has a best corrected distance visual acuity less than 6/9 in at least one eye or greater than or equal to two lines differences between the two eyes best corrected distance visual acuity in the absence of ocular pathology, and “No” if a child has best corrected distance visual acuity of 6/9 or better in both eyes or if the eye has/had a known ophthalmic pathology that would account for the reduction of vision.
School age children: Children aged between 6 and 18 years.
Prematurity: Birth before 37 weeks of gestation.
Cigarette smokers: Mothers were categorized as “Smokers” if they currently smoke at least one cigarette daily and as “non smokers” if theysmoke less than one cigarette per day.
“Alcohol drinkers“ were those who reported drinking any alcoholic beverage at least three times per week and above, but less than daily.
Refractive error: Depending on the result of the best vision sphere of the cycloplegic refraction result of the eye, refractive error was categorized as “Hypermetropia” if the child’s eye has a best vision sphere of ≥ +0.50DS and “Myopia” if the child’s eye has a best vision sphere of ≥ -0.50DS.
Strabismus: Depending on the cover–uncover test result strabismus was categorized as “Yes” if the uncovered eye during the cover–uncover test has any type of movement, and “No” if the uncovered eye has no movement during the cover–uncover test.
Mother's systemic illness: Systemic illness was categorized as “Yes” if the mother had a known positive history of diabetes mellitus and/or hypertension, and “No” if the mother had no known history of diabetes mellitus or hypertension.
Deprivation: deprivation was categorized as “Yes” if a child had a positive history of visual deprivation due to cataract and/or secondary or primary blepharoptosis which may or may not exist at the time of data collection, and “No” if the child had no positive history of visual deprivation due to cataract and/or blepharoptosis.
Data Collection Procedures and Tool
Data were collected using a pretested structured questionnaire that was developed from different literatures and a checklist through interview and physical examination. The questionnaire was pretested on 5% of the sample size outside the study area, and necessary modifications were made. Cronbach’s alpha was used to assess the reliability of the tool, and the scale was 0.72. Socio-demographic, socio-economic, maternal-related factors, gestation-related factors, developmental, familial and personal systemic and ophthalmic clinical factors were collected through the questionnaire at the subjects' home. After interviewing the parents/guardians, the children were brought in to FelegeHiwot Comprehensive Specialized Hospital for physical examination.
Distance VA was taken using a Snellen chart at 6 meters. Dry retinoscopy and cycloplegic refraction using 0.5% cyclopentolate eye drops were done for all study participants. A subjective refraction was done after 36 hours of installation of the cycloplegic drug for all study participants. Direct ophthalmoscopy was performed to detect any ophthalmic pathology in the eye. A cover test was done to detect the ocular deviations, and angles of deviation were estimated using a prism bar. These physical examinations were performed carefully by two trained senior clinical optometrists. The interview was conducted by four trained junior optometrists. One chief optometrist supervised the process and procedures of data collection. The parents/guardians of the participants were informed in detail, and a written consent was obtained. The participants/guardians of the participants were briefed that participation in this study was voluntary. They were informed that information gathered for the study will be used for academic purposes and it will also be an input for policy making purposes. Participants who volunteered to participate in this study were first interviewed at their home and then brought their child to the hospital for physical examination. During subjective refraction, the final subjective refraction prescription was given to the participating children's parents/guardians if the child had a refractive error.
Statistical Analysis
The collected data were cleaned and coded and entered to EPI info 7. Finally it was exported to and analyzed by SPSS version 20. Summary statistics, frequencies and cross-tabulations were performed for the descriptive analysis of the data. The effect of independent variables on the outcome variable was analyzed using binary logistic regression analysis. Multivariable logistic regression was done on all variables that had p value <0.2 in the bivariable logistic regression by using the “Backward: Conditional” method. Hosmer–Lemeshow goodness of fit test, variation inflation factor and Cronbach’s alpha were used to check the fulfillment of necessary assumptions, multicolinearity and reliability, respectively. The strength and direction of association were determined by adjusted odds ratio (AOR) with 95% level of significance.
Variables that had a p value <0.05 were taken as significant.
Results
Socio-Demographic Characteristics of Study Participants
In total 601 subjects participated in the study. The response rate was 91.79%. More than half (52.1%) of them were male, and about half (55.4%) of respondents were above 12 years old. A majority (28.1%) of study participants were in the age range of 13–15 years old. The mean age (in years) of study participants was 12 (SD=4.44 years) ().
Table 1 Socio-Demographic Characteristics of the Study Participants at Bahir Dar City, Northwest Ethiopia, 2018 (n=601)
Socio-Economic Characteristics of Study Participants
The majority of participating children had parents who were both employed (52.7%), and most households (43.9%) had 3–6 children ().
Table 2 Socio-Economic Characteristics of the Study Participants at Bahir Dar City, Northwest Ethiopia, 2018 (n=601)
Gestation, Birth and Maternal Characteristics of Study Participants
Out of the total participants, 21.5% were born before 37 weeks of gestation, 27.5% were admitted to the neonatal intensive care unit and 5.2% weighed less than 2.5 kg at birth ().
Table 3 Gestation, Birth and Maternal Characteristics of the Study Participants at Bahir Dar City, Northwest Ethiopia, 2018 (n=601)
Family-Related Factors of Study Participants
A positive family history of strabismus was reported for 2.2% of study participants. Nearly 15% of the parents of study participants used spectacles, either for assisting their vision or for protection purpose. About a quarter of the siblings of the study participants had a known visual complaint ().
Table 4 Family-Related Amblyogenic Characteristics of the Study Participants at Bahir Dar City, Northwest Ethiopia, 2018 (n=601)
Clinical Characteristics of Study Participants
More than 93% of study participants had completed their immunization. Only 1% of children had a presenting visual acuity less than 6/60. Myopia was found in the range of −0.50D to −22.00DS, and hyperopia was found between +0.50 and +9.00. The median of the myopia was −2.00DS (IQR 1.62 to −2.38). The median hyperopia was +2.12DS (IQR +1.00 to +3.88DS). High hyperopia was found in 2.5% of study participants ().
Table 5 Clinical Characteristics of the Study Participants at Bahir Dar City, Northwest Ethiopia, 2018 (n=601)
Prevalence and Types of Amblyopia
Amblyopia was prevalent in 6.5% (95% CI: 4.7–8.7%) of school age children in Bahir Dar city.
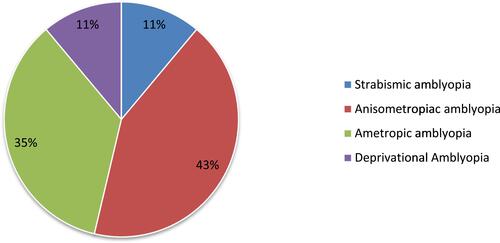
Anisometropic amblyopia and ametropic amblyopia are the commonest types of amblyopia. Some of the participants (15 children out of 39 amblyopic children) had more than one cause for amblyopia. Ten of 15 children had both refractive and anisometropic amblyopia. Three children had refractive and strabismic amblyopia. One child was found to have deprivational, refractive and strabismic amblyopia, and one more child had strabismic and anisometropic amblyopia ().
Factors Associated with Amblyopia
Variables that were significant in the bivariable logistic regression analysis included: age, sex, visual deprivation, anisometropia, strabismus, gestational age, NICU admission, mode of delivery, refractive error, exclusive breast feeding, systemic illness during pregnancy, presenting visual acuity of the child, family history of strabismus and past eye complaint; these were entered into the multivariable logistic regression model. In the multivariable binary logistic regression, the odds of being amblyopic among participants with a present or past positive history of visual deprivation were 8.3 times (AOR=8.34, CI: 2.45–28.44) more as compared to those who had no a present or past positive history of visual deprivation. The odds of being amblyopic among participants who had anisometropia of greater than 2D were about 9.3 times (AOR=9.35 CI: 2.86–30.60) more as compared to those who had no anisometropia. The odds of being amblyopic among participants having a refractive error > +5D hypermetropia were about 22 times (AOR=21.77, CI: 7.15–66.34) more as compared to those participants who had no/mild refractive error ().
Table 6 Factors Associated with Amblyopia Among the Study Participants at Bahir Dar City, Northwest Ethiopia, 2018 (n=601)
Discussion
This study showed that 6.5% (95% CI: 4.7–8.7%) of study participants had amblyopia. Among all study participants, anisometropic amblyopia was found in 3.8% (95% CI 2.3–5.3%), ametropic amblyopia was found in 3.2% (95% CI 1.8–4.7%), strabismic amblyopia was found in 1% (95% CI 0.3–1.8%) and deprivational amblyopia was also found in 1% (95% CI 0.3–1.8). This result is in line with two studies done in IndiaCitation23,Citation37 and one in Gondar, Ethiopia,Citation21 which reported 4.8%, 6.6% and 4.7%, respectively. The similarities could be due to similarities in the operational definition for the studies done in India and similarities in the socio-demographic factors of study participants for the study that was done in Gondar, Ethiopia.
However, the result of this study is higher than studies done in Egypt, Lagos state Nigeria,Citation19 Southern India,Citation22 Eastern Europe,Citation29 Saudi ArabiaCitation5 and Qassim province of Saudi Arabia,Citation24 which reported 1.49%, 1.41%, 1.1%, 2.8%, 2.5% and 3.5%, respectively. These differences might be due to the difference in study set up. Ours was a community-based study, whereas all these studies were conducted in schools, which missed those school age students who left schooling because of their poor vision. The reason for the difference between this study and the study in Egypt might be due to variations in the socio-demographic characteristics of study participants. In addition the study in Egypt includes 7–9-year-old primary school children only. Ageing increases the tendency of being amblyopic, thus the result of this study is higher because it includes older students up to 18 years old.
The result of this study is lower than other studies done in southwest Nigeria,Citation25 Menelik II
Hospital, Addis Ababa, EthiopiaCitation26 and Saudi Arabia,Citation27 which reported 12.9%, 9.1% and 9.5%, respectively.
This can be explained by the variation in the study set up. All those researches were done at hospitals, which means participants are those who had eye complaints. Thus, the result in this research is expected to be lower than those researches.
In this study, the odds of being amblyopic among school age children who had anisometropia greater than 1D were about 10.44 times (AOR=10.44, 95% CI: 3.57–30.56) more than those who had no anisometropia. This result is in line with studies done in AustraliaCitation14 and in China.Citation15,Citation17, The agreement between this study and the studies in Australia and ChinaCitation17 could be due to similarities in the study setting, as all of these researches are community-based studies. This research and one study conducted in ChinaCitation15 followed similar technical procedures during examining and diagnosing amblyopia, and this could be a reason for the agreement between the study findings.
In this study the odds of being amblyopic among participants who had anisometropia of greater than 2D were 9.3 times (AOR=9.35 CI: 2.86–30.60) more as compared to those who had no anisometropia. This result is in line with a study done in China,Citation17 and this can be explained by similarities in the study setting and design. This result is also supported by another study done in a sample of 6-year-old Australian children.Citation13
In this study, the odds of being amblyopic among participants who had anisometropia of less than 1D were about 4 times (AOR=4.12, 95% CI: 1.23–13.87) more as compared to those who had no anisometropia.
This research revealed that the odds of being amblyopic among participants having a refractive error of > +5D hypermetropia were about 22 times (AOR=21.77, 95% CI: 7.15–66.34) more than those participants who had no/mild refractive error. This finding is consistent with a study done in China,Citation17 and this could be due to the nature of the study setting. Both studies were done in a community setting, unlike other studies that were done in school settings; this similarity may lead in to similar findings.
The odds of being amblyopic among participants with a refractive error > +2D hypermetropia were about 7.31 times (AOR=7.31, 95% CI: 1.93–27.79) more as compared to those participants who had no/mild refractive error. This community-based study is in agreement with other community-based studies in AustraliaCitation14 and China.Citation17 These similarities in the designs of researches could be the reason for the agreement of the findings in the researches.
The odds of being amblyopic among participants with a present or past positive history of visual deprivation were 8.3 times (AOR=8.34, CI: 2.45–28.44) more as compared to those who had no present or past positive history of visual deprivation.
The odds of being amblyopic among participants with strabismus were 6.21 times (AOR=6.21, 95% CI: 1.70–22.70) more than those who had no strabismus. This result is in line with another study in Australian preschool children.Citation14 This result is also supported by another study done in a population-based sample of 6-year-old Australian children,Citation13 which reported that participants with strabismus were 65 times more likely to be amblyopic than those who had no strabismus.
The odds of being amblyopic among participants with a positive family history of strabismus were about 8 times (AOR=7.95, 95% CI: 2.09–30.22) more than those who had no positive family history of strabismus. This result also agreed with a study done in Kosofe Town, Lagos state, Nigeria.Citation19 This can be explained by similarities in the socio-demographic characteristics of study participants.
However, in the present study gestational age <37 weeks, admission to NICU and history of maternal cigarette smoking were not significantly associated with amblyopia. In contrast these factors were reported as significant positive factors for amblyopia in the studies done in Australia.Citation13 This might be justified by variations in the socio-economic and socio-demographic characteristics of the study participants.
Generally, this research provides important information regarding the prevalence of amblyopia and its associated factors among school age children in Bahir Dar city, northwest Ethiopia. However, it has the following limitations. Questions regarding the child's history, like birth weight of the child, history of admission to NICU, exclusive breast feeding, maternal alcohol consumption during pregnancy and history of eye diseases, need memory of the more distant past, so that the study might suffer from recall bias. This study also missed astigmatism as one factor for amblyopia, which was reported in studies from other countries. As this was a cross-sectional study, it has all the limitations of cross-sectional study design.
Based on the study findings, we recommend the Federal Ministry of Health, regional health bureaus and Bahir Dar city health authorities to set up a regular school age community screening program. It is imperative for the national, regional and zonal health sectors to develop a plan for community screening to detect amblyopia early. Depending on the findings of this study, the community and eye care workers are also recommended to further investigate children with strabismus, anisometropia and a history of visual deprivation due to media opacity (cataract), blepharoptosis or other causes for evaluation and appropriate management of amblyopia. Researchers are also recommended to conduct studies on amblyopia prevalence and associated factors among children including preschoolers and young adults in the community setting and involving a larger sample size as well as considering other factors like astigmatism in the analysis.
Conclusion
The prevalence of amblyopia among school age children at Bahir Dar city, northwest Ethiopia is higher than the WHO cut point.Citation32,Citation33 Having anisometropia greater than 1D, anisometropia > 2D, having anisometropia less than 1D, having a history of strabismus, having a hyperopia of > +5D, having a hyperopia of > +2D, having a positive history of visual deprivation and having a positive familial history of eye deviation were the significant factors positively associated with amblyopia.
Abbreviations
AOR, adjusted odds ratio; BCA, best corrected visual acuity; CI, confidence interval; COR, crude odds ratio; D, diopter; DS, diopter sphere; ETB, Ethiopian Birr; EPI INFO, epidemiological information; kg, kilogram; NICU, neonatal intensive care unit; SD, standard deviation; SPSS, Statistical Package for Social Sciences; SRS, simple random sampling; VA, visual acuity; WHO, World Health Organization.
Data Sharing Statement
The data used in this study can be accessed from the principal investigator upon reasonable request.
Ethical Approval and Consent to Participate
In this study the ethical Declaration of Helsinki was absolutely respected. The University of Gondar Institutional Review Board approved the ethical issue of the study. The College of Medicine and Health Sciences, School of Medicine Ethical Review Committee gave us ethical clearance. We obtained an informed written consent from the parents/guardians of each respondent. Verbal assent was also taken from the participants in the age range of 14 to 18 years old. After interviewing the guardians at their home, they were told to visit the eye care unit of FelegeHiwot Comprehensive Specialized Hospital for the physical examination. Children with a kind of eye problem were managed accordingly. Participants with refractive error were given their prescription to treat their optical disorders. Participants' information was gathered anonymously and confidentially.
Consent for Publication
For this study it is not applicable.
Author Contributions
MM conceptualized the idea, wrote the protocol, analyzed and interpreted the data and drafted the manuscript. ASA was involved in revising the protocol, coordinating the data collection and critically revised the manuscript. YAM critically read and commented on the protocol and the manuscript, and coordinated the data collection. All authors have read and approved the manuscript. All authors contributed to data analysis, drafting or revising the article, have agreed on the journal to which the article will be submitted, gave final approval of the version to be published and agree to be accountable for all aspects of the work.
Acknowledgments
Our acknowledgement goes to the Bahir Dar city administration office, FelegeHiwot Comprehensive Specialized Hospital and all study participants and their parents/guardians for their initiation and willingness to take part in this study.
Disclosure
The authors reported no conflicts of interest for this work.
Additional information
Funding
References
- Carlton J, Karnon J, Czoski-Murray C, Smith K, Marr J. The clinical effectiveness and costeffectiveness of screening programmes for amblyopia and strabismus in children up to the age of 4–5 years: a systematic review and economic evaluation. Health Technol Assess. 2008;12(25). doi:10.3310/hta12250
- Chuka-Okosa C. Amblyopia: types, presentation and treatment–A Review. Niger J Ophthalmol. 2003;11(2):54–62.
- Von Noorden GK. Binocular vision and ocular motility. Theory Manag Strabismus. 1990.
- Shaw D, Minshull C, Fielder A, Rosenthal A. Amblyopia—factors influencing age of presentation. Lancet. 1988;332(8604):207–209. doi:10.1016/S0140-6736(88)92301-X
- Al-Falki YH, Alamri DS, Fayi KA, Alahmari DS. Prevalence of amblyopia and its impact on the academic performance of male medical students in Southern Saudi Arabia. Saudi J Opthalmol. 2018;32(4):290–294. doi:10.1016/j.sjopt.2018.09.002
- Webber AL, Wood J. Amblyopia: prevalence, natural history, functional effects and treatment. Clin Exp Optom. 2005;88(6):365–375. doi:10.1111/j.1444-0938.2005.tb05102.x
- Van Leeuwen R, Eijkemans MJ, Vingerling JR, Hofman A, de Jong PT, Simonsz HJ. Risk of bilateral visual impairment in individuals with amblyopia: the Rotterdam study. Br J Opthalmol. 2007;91(11):1450–1451. doi:10.1136/bjo.2006.113670
- Donahue SP, Arnold RW, Ruben JB. Preschool vision screening: what should we be detecting and how should we report it? Uniform guidelines for reporting results of preschool vision screening studies. J AAPOS. 2003;7(5):314–316.
- Group M-ePEDS. Prevalence of amblyopia and strabismus in African American and Hispanic children ages 6 to 72 months: the multi-ethnic pediatric eye disease Study. Ophthalmology. 2008;115(7):1229–36. e1. doi:10.1016/j.ophtha.2007.08.001
- Ph M. cordonnier MD, Ph v DM. Comparison between two hand-held autorefractors: the sure-sight and the retinomax. Strabismus. 2004;12(4):261–274. doi:10.1080/09273970490886594
- Friedman DS, Repka MX, Katz J, et al. Prevalence of amblyopia and strabismus in white and African American children aged 6 through 71 months: the baltimore pediatric eye disease Study. Ophthalmology. 2009;116(11):2128–34. e2. doi:10.1016/j.ophtha.2009.04.034
- Ottar WL, Scott WE, Holgado SI. Photoscreening for amblyogenic factors. J Pediatr Ophthalmol Strabismus. 1995;32(5):289–295. doi:10.3928/0191-3913-19950901-06
- Robaei D, Rose KA, Ojaimi E, Kifley A, Martin FJ, Mitchell P. Causes and associations of amblyopia in a population-based sample of 6-year-old Australian children. Arch Ophthalmol. 2006;124(6):878–884. doi:10.1001/archopht.124.6.878
- Pai AS-I, Rose KA, Leone JF, et al. Amblyopia prevalence and risk factors in Australian preschool children. Ophthalmology. 2012;119(1):138–144. doi:10.1016/j.ophtha.2011.06.024
- Fu J, Li SM, Li SY, et al. Prevalence, causes and associations of amblyopia in year 1 students in Central China. Graefes Arch Clin Exp Ophthalmol. 2014;252(1):137–143. doi:10.1007/s00417-013-2451-z
- Rajavi Z, Sabbaghi H, Baghini AS, et al. Prevalence of amblyopia and refractive errors among primary school children. J Ophthalmic Vis Res. 2015;10(4):408. doi:10.4103/2008-322X.176909
- Huang D, Chen X, Zhu H, et al. Prevalence of amblyopia and its association with refraction in Chinese preschool children aged 36–48 months. Br J Opthalmol. 2018;102(6):767–771. doi:10.1136/bjophthalmol-2016-310083
- Robaei D, Rose K, Ojaimi E, Kifley A, Huynh S, Mitchell P. Visual acuity and the causes of visual loss in a population-based sample of 6-year-old Australian children. Ophthalmology. 2005;112(7):127582. doi:10.1016/j.ophtha.2005.01.052
- Ikuomenisan SJ, Musa KO, Aribaba OT, Onakoya AO. Risk factors associated with amblyopia among primary school pupils in Kosofe town, Lagos state, Nigeria. Niger J Ophthalmol. 2018;26(1):67. doi:10.4103/njo.njo_29_17
- Matsuo T, Matsuo C. The prevalence of strabismus and amblyopia in Japanese elementary school children. Ophthalmic Epidemiol. 2005;12(1):31–36. doi:10.1080/09286580490907805
- Haile W, Ayanaw T, Alemayehu D, Destaye S. Prevalence and types of amblyopia among primary school children in Gondar town, Northwest Ethiopia. Open Access Journal of Ophthalmology. 2017;2(3):000124.
- Ganekal S, Jhanji V, Liang Y, Dorairaj S. Prevalence and etiology of amblyopia in Southern India: results from screening of school children aged 5–15 years. Ophthalmic Epidemiol. 2013;20(4):228–231. doi:10.3109/09286586.2013.809772
- Janti SS, Raja A, Matheen A, Charanya C, Pandurangan R. A cross sectional study on prevalence of amblyopia in school going children. J Evol Med Dent Sci. 2014;3(30):8561–8566. doi:10.14260/jemds/2014/3086
- Aldebasi YH. Prevalence of amblyopia in primary school children in Qassim province, Kingdom of Saudi Arabia. Middle East Afr J Ophthalmol. 2015;22(1):86. doi:10.4103/0974-9233.148355
- Alarape AT, Ulaikere M, Okoye O, et al. Burden and spectrum of amblyopia in a pediatric hospital population Southwest Nigeria. Ann Med Health Sci Res. 2017;7(6).
- Woldeyes A, Girma A. Profile of amblyopia at the pediatric ophthalmology clinic of menilik II hospital, addisababa. Ethiop J Health Dev. 2008;22(2).
- Al-Tamimi ER, Shakeel A, Yassin SA, Ali SI, Khan UA. A clinic-based study of refractive errors, strabismus, and amblyopia in pediatric age-group. J Family Community Med. 2015;22(3):158. doi:10.4103/2230-8229.163031
- Elflein HM, Fresenius S, Lamparter J, et al. The prevalence of amblyopia in Germany: data from the prospective, population-based Gutenberg Health Study. Dtsch Arztebl Int. 2015;112(19):338.
- Mocanu V, Horhat R. Prevalence and risk factors of amblyopia among refractive errors in an Eastern European population. Medicina. 2018;54(1):6. doi:10.3390/medicina54010006
- McKean-Cowdin R, Cotter SA, Tarczy-Hornoch K, et al. Prevalence of amblyopia or strabismus in asian and non-Hispanic white preschool children: multi-ethnic pediatric eye disease study. Ophthalmology. 2013;120(10):2117–2124. doi:10.1016/j.ophtha.2013.03.001
- Mehari ZA. Pattern of childhood ocular morbidity in rural eye hospital, Central Ethiopia. BMC Ophthalmol. 2014;14(1):50. doi:10.1186/1471-2415-14-50
- Williams C, Northstone K, Harrad RA, Sparrow JM, Harvey I. Amblyopia treatment outcomes after screening before or at age 3 years: follow up from randomised trial. BMJ. 2002;324(7353):1549. doi:10.1136/bmj.324.7353.1549
- Newman DK, East MM. Prevalence of amblyopia among defaulters of preschool vision screening. Ophthalmic Epidemiol. 2000;7(1):67–71. doi:10.1076/0928-6586(200003)711-2FT067
- Kc S, Barakat B, Goujon A, Skirbekk V, Sanderson W, Lutz W. Projection of populations by level of educational attainment, age, and sex for 120 countries for 2005–2050. Demogr Res. 2010;22:383–472. doi:10.4054/DemRes.2010.22.15
- Huizink AC, Mulder EJ. Maternal smoking, drinking or cannabis use during pregnancy and neurobehavioral and cognitive functioning in human offspring. Neurosci Biobehav Rev. 2006;30(1):24–41. doi:10.1016/j.neubiorev.2005.04.005
- Anjaneyulu K, Reddy GN. Prevalence of amblyopia in children aged from 5–15 years in rural population Kurnool Dist. Andhra Pradesh, India. Indian J Ophthalmol. 2005;53(4):227–234. doi:10.4103/0301-4738.18903
- Abdelrazik ST, Khalil MF. Prevalence of amblyopia among children attending primary schools during the amblyogenic period in Minia county. J Egypt Ophthalmol Soc. 2014;107(4):220. doi:10.4103/2090-0686.150657