Abstract
Purpose
The aim of this study was to examine hospitalisation profiles related to postprocedural disorders of eye and adnexa in England and Wales.
Patients and Methods
This was an ecological study using publicly available data extracted from the “Hospital Episode Statistics (HES) database” in England and the “Patient Episode Database for Wales (PEDW)” for the period between April 1999 and April 2020. Diagnostic code for postprocedural disorders of eye and adnexa (H59) was used to identify hospital admission. We used the chi-squared test to assess the difference between the hospital admission rates between 1999 and 2020.
Results
Hospital admission rate decreased by 6.3% [from 4.98 (95% CI 4.79–5.17) in 1999 to 4.67 (95% CI 4.50–4.84) in 2020 per 100,000 persons, trend test, p<0.05]. The most common hospital admissions causes were other postprocedural disorders of eye and adnexa “Chorioretinal scars after surgery for detachment.” The age group 75 years and above accounted for 44.3% of the total number of admissions. Hospital admission rate among females decreased by 30.2% [from 5.90 (95% CI 5.61–6.19) in 1999 to 4.12 (95% CI 3.89–4.35) in 2020 per 100,000 persons]. Hospital admission rate among males increased by 30.2% [from 4.02 (95% CI 3.77–4.26) in 1999 to 5.23 (95% CI 4.97–5.49) in 2020 per 100,000 persons].
Conclusion
This study revealed that hospital admission rates for postprocedural disorders of the eye and adnexa decreased over the course of the study period. Eye and adnexa disorders accounted for the preponderance of hospital admissions among the elderly. Further research is required to identify risk factors that can be avoided.
Introduction
In the healthcare system, surgical procedure is a fundamental part.Citation1 Worldwide, over 230 million principal surgeries are performed annually.Citation2 All postoperative complications (serious or transient) are significant to patients.Citation3 The potential for postoperative complications is influenced by several factors, including the following: the pre-existing comorbid condition of the patients, the surgery type, and the perioperative management.Citation3 Furthermore, studies have demonstrated that aspects associated with postoperative complications include the following: anaesthesia, advanced age, longer duration of surgery, higher body mass index, intraoperative adverse events, comorbidities, combined organ resection, and smoking.Citation4–10
Although surgery risks are low for most patients, evidence increasingly indicates that postoperative complications are a significant reason for mortality.Citation11–14 Studies estimate that the proportion of patients who will experience postoperative complications when undergoing major surgical procedures is 7–15%.Citation15,Citation16 Globally, about three million of the 25 million patients who undergo high-risk surgeries die before being discharged from the hospital each year.Citation14,Citation17 The overall postoperative mortality rate is estimated at 0.8%-5.7%.Citation18 In the UK, approximately 10% of surgical patients are at high risk for complications.Citation3
In addition to the fact that postoperative complications cause suffering and death, they cause hospital stays for more extended periods and thus increase costs even more.Citation3,Citation18,Citation19 Postoperative complications can be specific to certain operations or general.Citation3 In this article, we examined trends of hospital admissions due to postprocedural disorders of eye and adnexa in England and Wales from 1999 to 2020. Between 2018 and 2019, about 20,000 cataract surgeries were performed in Wales and 452,000 in England.Citation20 According to a national ophthalmology database audit, 47,248 patients underwent procedures on both eyes.Citation20 No previous studies in the United Kingdom have examined hospitalisation due to postprocedural disorders of eye and adnexa. The aim of this study was to examine hospitalisation profiles related to postprocedural disorders of eye and adnexa in England and Wales. Understanding and handling postprocedural disorders are of utmost importance in ensuring the welfare of patients who have had ocular operations or procedures. Furthermore, the examination of postprocedural complications in the ocular region and its surrounding structures has the potential to drive progress in surgical methodologies, postoperative care guidelines, and the creation of procedures that are both safer and more efficient. Enhancing patient outcomes in the future can be facilitated by comprehending the etiology and risk factors associated with these complications.
Methods
Study Sources and the Population
This was an ecological study using publicly available data extracted from the “Hospital Episode Statistics (HES) database” in England and the “Patient Episode Database for Wales (PEDW)” for the period between April 1999 and April 2020.Citation21,Citation22 These medical databases were previously used to examine hospitalisation profiles for different health conditions.Citation23–27 The HES and PEDW databases contain hospital admission data for patients with postprocedural disorders of eye and adnexa from all age groups, which are subdivided into four categories; “below 15 years, 15–59 years, 60–74 years, and 75 years and above.” Diagnostic code for postprocedural disorders of eye and adnexa (H59) was used to identify hospital admission. HES and PEDW databases record all hospital admissions, Outpatients, and Accident and Emergency (A&E) activities performed at all National Health Service (NHS) trusts and any independent sector funded by NHS trusts. Data for hospital admissions in England and Wales are available from the years 1999/2000 onwards. Available data include patient demographics, clinical diagnoses, procedures, and duration of stay. Mid-year population data were collected from the Office for National Statistics (ONS).
Statistical Analysis
Hospital admission rates with 95% confidence intervals (CIs) were calculated using the finished consultant episodes of postprocedural disorders of eye and adnexa-related admission divided by the mid-year population. We used the chi-squared test to assess the difference between the hospital admission rates between 1999 and 2020. Trends in hospital admissions were assessed using a Poisson model. All analyses were conducted using SPSS version 25 (IBM Corp, Armonk, NY, USA).
Results
The total annual number for postprocedural disorders of eye and adnexa hospital admissions for various causes increased by 7.3% from 2598 in 1999 to 2788 in 2020, representing a decrease in the hospital admission rate of 6.3% [from 4.98 (95% CI 4.79–5.17) in 1999 to 4.67 (95% CI 4.50–4.84) in 2020 per 100,000 persons, trend test, p<0.05].
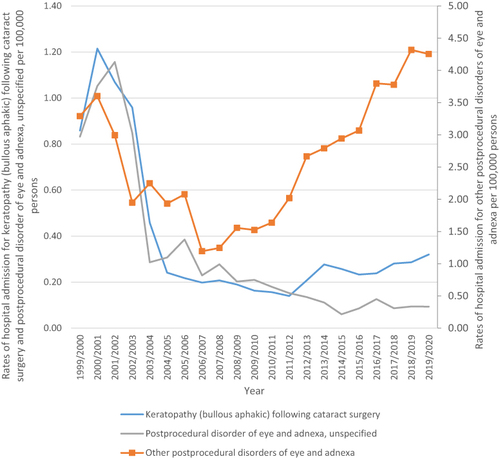
The most common postprocedural disorders of eye and adnexa hospital admissions causes were other postprocedural disorders of eye and adnexa, which accounted for 79.1% (). The average length of stay for keratopathy (bullous aphakic) following cataract surgery and postprocedural disorder of eye and adnexa, unspecified was 1 day. The average length of stay for other postprocedural disorders of eye and adnexa (Chorioretinal scars after surgery for detachment) was 2 days.
Table 1 Percentage of Postprocedural Disorders of Eye and Adnexa from Total Number of Admissions
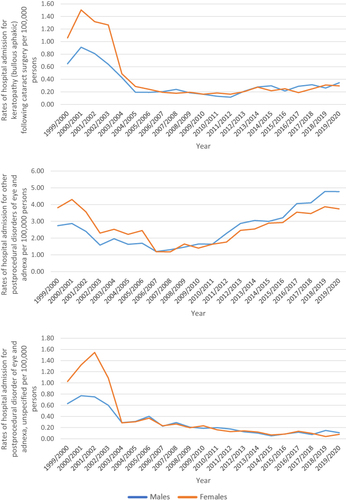
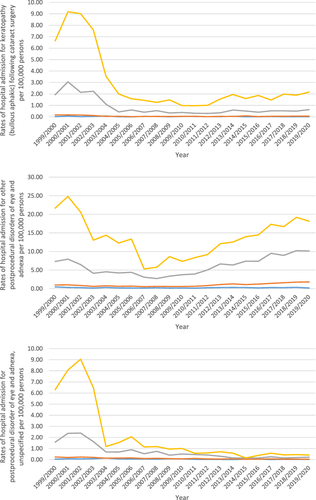
Over the study duration, postprocedural disorders of eye and adnexa admissions rates for the postprocedural disorder of eye and adnexa, unspecified and keratopathy (bullous aphakic) following cataract surgery were decreased by 88.7% and 62.8%, respectively. Besides, postprocedural disorders of eye and adnexa hospital admissions rates for other postprocedural disorders of eye and adnexa were increased by 29.3% (, ).
Table 2 Percentage Change in Hospital Admission Rates
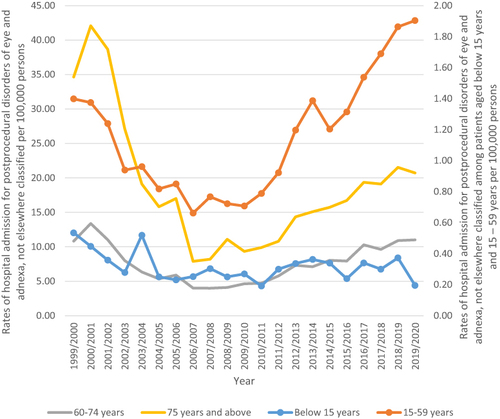
Concerning age group difference for postprocedural disorders of eye and adnexa, not elsewhere classified hospital admission: the age group 75 years and above accounted for 44.3% of the total number of postprocedural disorders of eye and adnexa, not elsewhere classified hospital admissions, followed by the age group 60–74 years with 33.3%, the age group 15–59 years with 20.8%, and then the age group below 15 years with 1.7%. Rates of hospital admission for postprocedural disorders of eye and adnexa, not elsewhere classified among patients aged below 15 years decreased by 63.5% [from 0.53 (95% CI 0.39–0.68) in 1999 to 0.20 (95% CI 0.11–0.28) in 2020 per 100,000 persons]. Rates of hospital admission for postprocedural disorders of eye and adnexa, not elsewhere classified among patients aged 15–59 years increased by 36.1% [from 1.40 (95% CI 1.27–1.53) in 1999 to 1.90 (95% CI 1.76–2.05) in 2020 per 100,000 persons]. Rates of hospital admission for postprocedural disorders of eye and adnexa, not elsewhere classified among patients aged 60–74 years increased by 1.7% [from 10.81 (95% CI 10.04–11.59) in 1999 to 11.00 (95% CI 10.33–11.67) in 2020 per 100,000 persons]. Rates of hospital admission for postprocedural disorders of eye and adnexa, not elsewhere classified among patients aged 75 years and above decreased by 40.2% [from 34.64 (95% CI 32.79–36.48) in 1999 to 20.73 (95% CI 19.49–21.97) in 2020 per 100,000 persons] ().
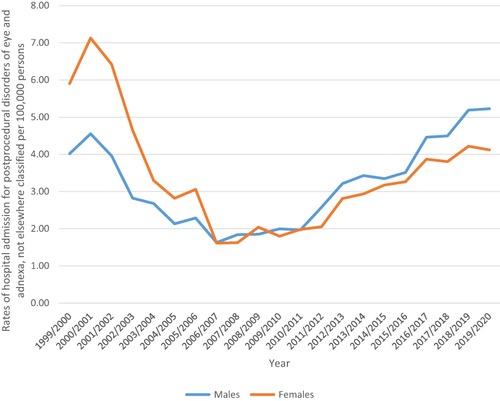
A total of 38,984 postprocedural disorders of eye and adnexa, not elsewhere classified hospital admission episodes were reported in England and Wales during the study time. Females contributed to 52.4% of the total number of postprocedural disorders of eye and adnexa, not elsewhere classified hospital admission accounting for 20,443 hospital admission episodes by a mean of 973 per year. Postprocedural disorders of eye and adnexa, not elsewhere classified hospital admission rate among females decreased by 30.2% [from 5.90 (95% CI 5.61–6.19) in 1999 to 4.12 (95% CI 3.89–4.35) in 2020 per 100,000 persons]. Postprocedural disorders of eye and adnexa, not elsewhere classified hospital admission rate among males were increased by 30.2% [from 4.02 (95% CI 3.77–4.26) in 1999 to 5.23 (95% CI 4.97–5.49) in 2020 per 100,000 persons] ().
Postprocedural Disorders of Eye and Adnexa, Not Elsewhere Classified Admission Rate by Gender
All postprocedural disorders of eye and adnexa, not elsewhere classified hospital admission rates were higher among females compared to males ().
Postprocedural Disorders of Eye and Adnexa, Not Elsewhere Classified Admission Rate by Age
All postprocedural disorders of eye and adnexa, not elsewhere classified hospital admission rates were directly related to age (more common among the age group 75 years and above), .
Discussion
This ecological study looked at hospital admission rate for postprocedural disorders of eye and adnexa in the UK between 1999 and 2020. We found that the total annual number for postprocedural disorders of eye and adnexa, not elsewhere classified hospital admissions for various causes increased by 7.3% from 2598 in 1999 to 2788 in 2020, representing a decrease in the hospital admission rate of 6.3% [from 4.98 (95% CI 4.79–5.17) in 1999 to 4.67 (95% CI 4.50–4.84) in 2020 per 100,000 persons]. The most common postprocedural disorders of eye and adnexa, not elsewhere classified hospital admissions causes were other postprocedural disorders of eye and adnexa, which accounted for 79.1%. Concerning age group difference: we found that the age group 60 years and above accounted for the majority (77.0%) of the total number of postprocedural disorders of eye and adnexa, not elsewhere classified hospital admissions, followed by other age groups. We also found that females contributed to 52.4% of the total number of postprocedural disorders of eye and adnexa, not elsewhere classified hospital admission.
Previous studies investigating the overall trend in post-operative eye surgeries complications are limited, and most of the studies focused on specific eye surgeries or diagnosis. However, the findings of the study are generally consistent with previous study that looked into the rate of postprocedural complications of eye and adnexa. A previous study by Alrawashdeh et al investigated the trend of hospital admissions concerning diseases of the eye and adnexa in the United Kingdom in the past 20 years using HES data, and they concluded that the postprocedural complications of eye and adnexa were decreased by 6% over the study period.Citation28 These findings were consistent with our results as we found that postprocedural disorders of eye and adnexa, not elsewhere classified hospital admissions rates for postprocedural disorders of eye and adnexa, unspecified and keratopathy (bullous aphakic) following cataract surgery decreased by 88.7% and 62.8%, respectively.
Lens and eye surgeries are the most common ophthalmic procedures, in which the risk of hospitalization for these two conditions can be considered generally low.Citation29 In addition, taking into consideration the advancement in the medical technology, one-day surgery, and the cost-effectiveness approaches, the results of this study seem to be a representative estimate of the current clinical practice in the UK and the reduction the hospital admission.
The most common postprocedural disorders of eye and adnexa, not elsewhere classified hospital admissions causes were other postprocedural disorders of eye and adnexa including chorioretinal scars after surgery for detachment, which accounted for 79.1%, this was followed by Keratopathy (bullous aphakic) following cataract surgery, which accounted for nearly 11% of the hospital admissions. These results were also in line with previous studies that investigated frequency of retinal detachment admissions and vitreo-retinal surgery procedures performed between 2000 and 2018 in England. The authors found that the frequency of admissions to hospital for surgically treated retinal detachment seems to have been increasing significantly since 2000.Citation30 This observation can also be explained by multiple reasons including the aging population. Several studies have reported that age is an important risk factor for retinal detachment conditions,Citation31,Citation32 and other factors that may explain this observation include an increase in number of comorbidities including diabetes and improvement in public awareness.Citation33
This study found that the older age group 60 and above accounted for the majority of the hospital admission cases, these findings can be explained by multiple reasons including the fact that majority of the eye procedures are for the older age group but also may be explained by the fact that older age group usually have other comorbidities such as diabetes, hypertension, which may increase the risk of post-procedural complications such as infections.Citation30,Citation34,Citation35
This study showed a decreasing trend in hospital admission rate for postprocedural disorders of eye and adnexa in the UK during the past two decades in the UK. This indicates a better health-care system and early detection, fewer complications, and cost-effectiveness approaches.Citation36 However, the rise in other postprocedural disorders of eye and anexa, including chorioretinal scars after surgery for detachment, is also related to the increase in the aging population.
This study has several strength points including that this is the first study to explore trends in hospital admission rate for postprocedural disorders of eye and adnexa in the UK between 1999 and 2020. The study was a population study at the national level, and we analyse the data stratified by age and gender variations over 20 years’ period. However, this study has some limitations, in this study we did not have patient-level data and our data do not directly address the underlying reasons for the trends.Citation37 Factors such as demographic changes obesity, lifestyles, health guidelines, and comorbidities were not considered in our analysis. In addition, for each ICD-10 code range, we were unable to specifically identify which eye problems had the greatest impact on the hospital admission rate.
Conclusion
This study found that postprocedural disorders of eye and adnexa, not elsewhere classified hospital admissions rates for postprocedural disorders of eye and adnexa, were decreased over the study period. Elder age group accounted for the majority of hospital admission due to disorders of eye and adnexa.
Data and Materials Availability
All data associated with this study are presented in this paper. The data accessed complied with relevant data protection and privacy regulations.
Ethical Approval
The study was approved by the Institutional Review Board at Isra University, Amman, Jordan (SREC/22/08/49).
Author Contributions
M.R.N. and A.Y.N. participated in protocol design, data collection, investigation, supervised this study, and drafted the first manuscript. All authors reviewed and approved the final manuscript. All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
No conflicts of interests to be declared.
Additional information
Funding
References
- Reid J, Clarke J. Progressing safer surgery. J Perioper Pract. 2009;19(10):336–341. doi:10.1177/175045890901901006
- Weiser TG, Regenbogen SE, Thompson KD, et al. An estimation of the global volume of surgery: a modelling strategy based on available data. Lancet. 2008;372(9633):139–144. doi:10.1016/S0140-6736(08)60878-8
- Hobson B, Liu DY-M, Hadjipavlou DN. An Introduction to Postoperative Complications. University College London; 2016.
- Boyd-Carson H, Gana T, Lockwood S, Murray D, Tierney GM. A review of surgical and peri-operative factors to consider in emergency laparotomy care. Anaesthesia. 2020;75(1):e75–e82. doi:10.1111/anae.14821
- Cai M, Zeng XY, Xiong Z, et al. Early postoperative complications and risk factors in laparoscopic D2 radical gastrectomy for gastric cancer. Zhonghua Wei Chang Wai Ke Za Zhi. 2019;22(8):742–747. doi:10.3760/cma.j.issn.1671-0274.2019.08.008
- Gajdos C, Hawn MT, Campagna EJ, Henderson WG, Singh JA, Houston T. Adverse effects of smoking on postoperative outcomes in cancer patients. Ann Surg Oncol. 2012;19(5):1430–1438. doi:10.1245/s10434-011-2128-y
- Greenstein AJ, Wahed AS, Adeniji A, et al. Prevalence of adverse intraoperative events during obesity surgery and their sequelae. J Am Coll Surg. 2012;215(2):1–13. doi:10.1016/j.jamcollsurg.2012.03.008
- Kim BD, Hsu WK, De Oliveira GS, Saha S, Kim JY. Operative duration as an independent risk factor for postoperative complications in single-level lumbar fusion: an analysis of 4588 surgical cases. Spine. 2014;39(6):510–520. doi:10.1097/BRS.0000000000000163
- Rampersaud YR, Moro ER, Neary MA, et al. Intraoperative adverse events and related postoperative complications in spine surgery: implications for enhancing patient safety founded on evidence-based protocols. Spine. 2006;31(13):1503–1510. doi:10.1097/01.brs.0000220652.39970.c2
- Sandler RS, Maule WF, Baltus ME. Factors associated with postoperative complications in diabetics after biliary tract surgery. Gastroenterology. 1986;91(1):157–162. doi:10.1016/0016-5085(86)90452-X
- Findlay GP GA, Protopapa K. Knowing the Risk: a review of the perioperative care of surgical patients; 2011. Available from: https://www.ncepod.org.uk/2011poc.html. Accessed June 17, 2023.
- Jhanji S, Thomas B, Ely A, Watson D, Hinds CJ, Pearse RM. Mortality and utilisation of critical care resources amongst high-risk surgical patients in a large NHS trust. Anaesthesia. 2008;63(7):695–700. doi:10.1111/j.1365-2044.2008.05560.x
- Khuri SF, Henderson WG, DePalma RG, Mosca C, Healey NA, Kumbhani DJ. Participants in the VA national surgical quality improvement program. Determinants of long-term survival after major surgery and the adverse effect of postoperative complications. Ann Surg. 2005;242(3):326–343. doi:10.1097/01.sla.0000179621.33268.83
- Pearse RM, Harrison DA, James P, et al. Identification and characterisation of the high-risk surgical population in the United Kingdom. Critical Care. 2006;10(3):1–6.
- Haynes AB, Weiser TG, Berry WR, et al.; Safe Surgery Saves Lives Study Group. A surgical safety checklist to reduce morbidity and mortality in a global population. N Engl J Med. 2009;360(5):491–499. doi:10.1056/NEJMsa0810119
- Tevis SE, Cobian AG, Truong HP, Craven MW, Kennedy GD. Implications of multiple complications on the postoperative recovery of general surgery patients. Ann Surg. 2016;263(6):1213–1218. doi:10.1097/SLA.0000000000001390
- Pearse RM, Moreno RP, Bauer P, et al. European Surgical Outcomes Study (EuSOS) group for the trials groups of the European Society of Intensive Care Medicine and the European Society of Anaesthesiology. Mortality after surgery in Europe: a 7 day cohort study. Lancet. 2012;380(9847):1059–1065. doi:10.1016/S0140-6736(12)61148-9
- Tevis SE, Kennedy GD. Postoperative complications and implications on patient-centered outcomes. J Surg Res. 2013;181(1):106–113. doi:10.1016/j.jss.2013.01.032
- Khan NA, Quan H, Bugar JM, Lemaire JB, Brant R, Ghali WA. Association of postoperative complications with hospital costs and length of stay in a tertiary care center. J Gen Intern Med. 2006;21(2):177–180. doi:10.1007/s11606-006-0254-1
- The Royal College of Ophthalmologists. National ophthalmology database audit, key findings summary 2020; 2020. Available from: https://www.nodaudit.org.uk/u/docs/20/ctshjnsvvi/NODAuditKeyFindingsSummary2020.pdf. Accessed June 17, 2023.
- National Health Services. Hospital admitted patient care activity, 2019–20: procedures and interventions. Digital.Nhs.Uk.; 2020. Available from: https://files.digital.nhs.uk/20/0864E6/hosp-epis-stat-admi-proc-2019-20-tab.xlsx. Accessed June 17, 2023.
- PEDW Data Online. Digital health and care wales. Digital Health and Care Wales; 2023. Available from: https://nwis.nhs.wales/information-services/health-intelligence/pedw-data-online/. Accessed June 17, 2023.
- Al-Daghastani T, Naser AY. Hospital admission profile related to poisoning by, adverse effect of and underdosing of psychotropic drugs in England and Wales: an ecological study. Saudi Pharm J. 2022;30(9):1262–1272. doi:10.1016/j.jsps.2022.06.025
- Mustafa Ali MK, Naser AY, AbuAlhommos A, et al. Hospital admissions secondary to diseases of the blood, blood-forming organs, and immune system in England and wales. Cureus. 2022;14(10):e30179. doi:10.7759/cureus.30179
- Mustafa Ali S, Naser AY, Alghanemi AG, et al. Musculoskeletal system and connective tissue related hospital admission in England and Wales between 1999 and 2019: an ecologic study. Cureus. 2022;14(12):e32453. doi:10.7759/cureus.32453
- Naser AY, Dahmash EZ, Al-Daghastani T, et al. An ecological analysis of hospitalization patterns for diseases of the nervous system in England and Wales over the last 20 years. Healthcare. 2022;10(9):1670. doi:10.3390/healthcare10091670
- Naser AY, Dahmash EZ, Alqahtani JS, Alsairafi ZK, Alsaleh FM, Alwafi H. Trends in hospital admissions for mental, behavioural and neurodevelopmental disorders in England and Wales between 1999 and 2019: an ecological study. Healthcare. 2022;10(11):2191. doi:10.3390/healthcare10112191
- Alrawashdeh HM, Naser AY, Alwafi H, et al. Trends in hospital admission due to diseases of the eye and adnexa in the past two decades in England and Wales: an ecological study. Int J Gen Med. 2022;15:1097–1110. doi:10.2147/IJGM.S344380
- Wang SY, Blachley TS, Andrews CA, Ayanian JZ, Lee PP, Stein JD. Hospitalization after cataract surgery in a nationwide managed-care population. PLoS One. 2016;11(2):1–14.
- Madi HA, Keller J. Increasing frequency of hospital admissions for retinal detachment and vitreo-retinal surgery in England 2000–2018. Eye. 2022;36(8):1610–1614. doi:10.1038/s41433-021-01647-2
- Faghihi H, Jalali KH, Amini A, Hashemi H, Fotouhi A, Esfahani MR. Rhegmatogenous retinal detachment after LASIK for myopia. J Ref Surg. 2006;22(5):448–452. doi:10.3928/1081-597X-20060501-05
- Raczyńska D, Glasner L, Serkies-Minuth E, Wujtewicz MA, Mitrosz K. Eye surgery in the elderly. Clin Interv Aging. 2016;11:407–414. doi:10.2147/CIA.S101835
- Bastawrous A, Mathenge W, Nkurikiye J, et al. Incidence of visually impairing cataracts among older adults in Kenya. JAMA network open. 2019;2(6):1–15. doi:10.1001/jamanetworkopen.2019.6354
- Desai P, Reidy A, Minassian DC. Profile of patients presenting for cataract surgery in the UK: national data collection. Br J Ophthalmol. 1999;83(8):893–896. doi:10.1136/bjo.83.8.893
- Yong GY, Mohamed-Noor J, Salowi MA, Adnan TH, Zahari M, Grzybowski A. Risk factors affecting cataract surgery outcome: the Malaysian cataract surgery registry. PLoS One. 2022;17(9):1–11. doi:10.1371/journal.pone.0274939
- Syed ZA, Moayedi J, Mohamedi M, et al. Cataract surgery outcomes at a UK independent sector treatment centre. Br J Ophthalmol. 2015;99(11):1460–1465. doi:10.1136/bjophthalmol-2014-306586
- Sivasubramaniam V, Patel HC, Ozdemir BA, Papadopoulos MC. Trends in hospital admissions and surgical procedures for degenerative lumbar spine disease in England: a 15-year time-series study. BMJ open. 2015;5(12):e009011. doi:10.1136/bmjopen-2015-009011