Abstract
Purpose
Multifocal soft contact lenses (MFCLs) have been proposed and used for controlling the rate of myopia progression; however, little is known on the performance and adaptation with MFCLs in non-presbyopes. This study aims to evaluate the visual performance of four commercially available MFCLs in non-presbyopic myopic eyes during an adaptation period.
Methods
Fifty-two experienced myopic contact lens wearers (67% female; mean age 21.4±2.0 years) were enrolled in this trial and 40 completed the trial. Twenty-six participants (Group 1) wore Lotrafilcon B single vision (SV, control), Omafilcon A MFCL center-distance (D) and center-near (N) and the other 26 participants (Group 2) wore Lotrafilcon B SV, Lotrafilcon B MFCL N, and Balafilcon A MFCL N. Lens order was randomized. Participants wore each allocated lens for a minimum of 8 days over four scheduled visits (dispensing and three follow-up visits) with a 1-week washout period between the lens types. At each visit, high-contrast visual acuity (HCVA) (in logarithm of the minimum angle of resolution [logMAR]) and seven subjective performance variables (via questionnaire) were obtained. Power profiles of each lens type, pupil size, and contact lens centration, with lens placed on the eye, were measured.
Results
The SV control outperformed the MFCLs in all variables (P<0.05). There were no significant differences in HCVA over time, with the exception of monocular HCVA with Omafilcon A MFCL N, which at the end of the adaptation period had significantly (P<0.05) improved by 0.10 logMAR. No differences were found between visits for any subjective variables. Subjectively, Lotrafilcon B MFCL N performed best and was the only lens that did not decenter significantly compared to the SV control. Conversely, Omafilcon A MFCL N was the worst performing and most decentered lens (P<0.05, y=−0.39 mm), with the greatest plus area under the power profile.
Conclusion
MFCLs with greatest power variation across the optic zone, a greater plus area under the distance labeled power profile, and/or lenses that were significantly decentered resulted in the lowest subjective ratings. Over time, quality of vision with MFCLs did not change in non-presbyopic myopic participants, with the exception of Omafilcon A MFCL N, which showed some adaptation effects.
Introduction
Myopia, with its increasing prevalence worldwide,Citation1 has become a significant global health problem, particularly due to the associated risks of developing glaucoma,Citation2 cataract,Citation3 and retinal detachment.Citation4
Conventionally, myopia is corrected with single vision (SV) spectacle or contact lenses, which provide clear foveal distance vision. Over the last decade, multifocal contact lenses (MFCLs) have been proposed and tested as a method of controlling myopia progression.
To date, three hypotheses have been postulated for justifying an intervention with MFCLs. The first approach is based on the associations found between increased accommodative lag and myopia.Citation5–Citation8 It was hypothesized that lenses that reduce accommodative lag, that is, on-axis hyperopic defocus, may reduce the rate of myopia progression. It has been shown that lenses incorporated with negative spherical aberration reduce accommodative lag.Citation9,Citation10 Given that center-near MFCLs (MFCL N) have inherent negative spherical aberration,Citation11 it can be argued that they may potentially be producing a therapeutic benefit. The second hypothesis relies on the designs that have shown to reduce the peripheral hyperopic defocus and/or induce peripheral myopic defocus. Such an optical manipulation was proposed to discourage myopia progression.Citation12,Citation13 The third hypothesis includes a class of lenses that are designed to impose simultaneous defocus on the visual system, where one zone corrects the refractive error, while the other zone (with relative plus to the baseline prescription power) offers a stop signal (eg, concentric-ring bifocal).Citation14,Citation15
All types of MFCLs tested for the reduction of rate of progression reported an efficacy of approximately 35%–45%.Citation14–Citation17 On the other hand, the results obtained with bifocal or progressive spectacle lenses based on similar hypothesis remain equivocal.Citation18–Citation20 One plausible explanation offered to support results with MFCLs is that perhaps MFCLs deliver a more controlled treatment compared to bifocal or progressive addition spectacle lenses, as the downward ocular deviation with spectacles can significantly reduce the therapeutic effect.Citation21
Depending on the optical design, MFCLs can reduce hyperopic defocus, on-axis (eg, MFCL N) or in the periphery of the eye (eg, center-distance MFCL [MFCL D]). Although, the actual theory that underpins the treatment effect still remains questionable, one could infer from the literature that, in general, MFCLs seem to offer a protective effect against myopia progression. One of the main limiting factors for using MFCLs in non-presbyopes is the unwarranted accompaniment of visual compromise. While it is expected from theory that such optics would bring in compromise when compared to SV lenses, there seems to be a prevailing argument that given some time for neural adaptation, the performance is expected to improve. Fernandes et alCitation22 assessed changes in visual performance with MFCL correction in a presbyopic group after 15 days of lens wear and found some adaptation effects. However, to our knowledge no studies have investigated adaptation effects, particularly when MFCLs are prescribed to non-presbyopic individuals. Further, the majority of the studies investigating therapeutic benefit with MFCLs include custom-designed optics. However, it would be in the practitioner’s interest to know the commercially available options at hand, should they be proactive enough to offer MFCLs to their progressing myopic patients. Therefore, we only explored MFCLs available in the market. To date, only MFCL D and concentric-ring bifocal “type” lenses have been explored in the clinical trials that investigated for myopia control. The underlying drive for avoiding MFCL N, albeit its potential to reduce on-axis hyperopic defocus, would have been primarily driven by concern for a presumed greater visual performance degradation than MFCL D and concentric-type MFCLs counterparts. Given that the majority of contact lens manufacturers offer MFCL N designs, we sought to gauge visual performance of such designs as well.
Although several MFCLs have been tested with respect to their efficacy in slowing myopia progression,Citation14,Citation16,Citation23,Citation24 only a few studies (with limited designs) have thoroughly evaluated the visual performance, and none have looked into adaptation with such lenses in myopic non-presbyopic eyes.Citation25–Citation28 Lastly, differences in visual performance between MFCLs can be attributed to differences in their power profiles,Citation11,Citation29 pupil size,Citation30,Citation31 and contact lens centration.Citation28,Citation32,Citation33
Based on this, the objectives of the current study were to assess the visual performance of four commercially available MFCL designs, ie, one MFCL D and three MFCL N, during an adaptation period and to measure and discuss the impact of vision-dependent factors, such as the power profiles, pupil size, and lens centration of the different MFCLs.
Methods
Study design and contact lenses
This was a prospective, participant-masked, multiple-group, cross-over, randomized clinical trial in which participants wore three of five different contact lens types bilaterally. details the outline of the study visits. Participants were randomized into one of two groups. The multiple group design was chosen to avoid discontinuations by participants due to the otherwise extended trial duration. Participants in Group 1 were assigned to wear Lotrafilcon B SV (control), Omafilcon A MFCL D, and Omafilcon A MFCL N, whereas participants in Group 2 were assigned to wear Lotrafilcon B SV (control), Lotrafilcon B MFCL N, and Balafilcon A MFCL N. All MFCLs had high add powers, in order to allow for a direct comparison of visual performance with respect to the lens designs. The Lotrafilcon B SV lens was chosen as a control lens due to its minimal spherical aberration.Citation11 The order of lens designs tested in each group was randomized. details the lenses used in this trial. AOSept Plus (Alcon, Fort Worth, TX, USA) was used for disinfection and storage of the contact lenses.
Figure 1 Outline of study visits.
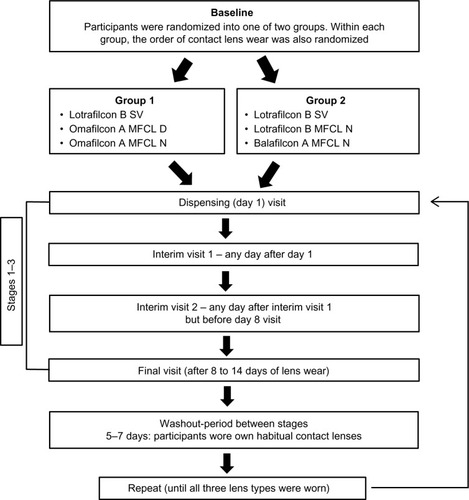
Table 1 Description of contact lenses and modality used in both groups
The lens power for all lenses was selected based on the spherical equivalent of the distance subjective refraction performed at the baseline visit with the control lens and adjusted for vertex distance. It should be noted that, although using the same distance power for all study lenses permits a direct comparison of visual performance if the lenses were to be fitted as potential myopia control lenses, better vision at distance would be anticipated if an over-refraction was performed, in particular with the MFCL N.
Each participant was asked to wear each of the three lens types on a daily wear schedule for a minimum of 6 hours per day. In total, there were three stages for each participant corresponding to each lens type worn. For each of the three stages, the participant had to attend four visits: a lens dispensing visit, two interim visits, and a final visit. The final visit was performed after 8–14 days of lens wear. The interim visits were performed on any day between day 1 and the final visit of contact lens wear. During all four visits, a series of ocular assessments was performed, which included assessments of monocular and binocular high-contrast visual acuity (HCVA), contact lens fitting, and a questionnaire on vision and comfort with these lenses. To avoid lens bias when answering the questionnaires, the participants were masked to the study contact lenses they wore. The appointments for the two interim visits and the final visit were aimed to be scheduled before 2 pm to avoid taking measurements that might be affected by fatigue of the eyes. At the end of each stage, participants were asked to wear their habitual correction for 5 (+2) days to allow a washout period before commencing the next stage.
Participants
The protocol and informed consent were reviewed and approved by the Bellberry Human Research Ethics Committee, and the research followed the tenets of the Declaration of Helsinki. The study was registered with the Australian and New Zealand Clinical Trial Registry (ACTRN12611001004954) prior to the enrollment of participants. Participants were screened for general trial suitability and written informed consent was obtained prior to any clinical procedures. The inclusion criteria of the study were: myopia between −1.00 D and −4.00 D, astigmatism no greater than −1.00 DC, and experienced contact lens wearers, aged 18–25 years. Although it would have been preferred to enroll younger participants, ie, an age group in which myopia control therapies are more likely to be tested, previous experience in recruiting young myopes in Sydney proved to be very difficult, and thus the population in this study was limited to young adults. Exclusion criteria included any ocular disease or systemic disease that would contraindicate contact lens wear, or anisometropia above 1.00 D. Fifty-two participants were recruited, of whom 40 participants completed all 12 visits. There were no significant differences (P>0.05) in the number of discontinuations between the groups or lenses. Discontinuations were primarily related to unacceptable vision or discomfort with the study lenses.
Procedures
Binocular and monocular HCVA (in logarithm of the minimum angle of resolution [logMAR]) was assessed under high illumination (557±11 lux at participant eye position) using a computer-generated LogMAR vision letter chart (David Thomson Chart 2000; IOO Marketing, London, UK) at a distance of 6 m.Citation34 At each visit, participants rated each lens monocularly for comfort and vision as indicated in . The questionnaire used a numeric rating scale, which ranged from 0 to 10, in steps of 1 unit, where 0 indicates lowest performance and 10 indicates best performance. Pupil sizes were measured at each of the three dispensing visits, under mesopic (80 Lux) illumination condition, using a custom-built, infrared pupillometer. The power profiles of all study lenses were measured using NIMO TR1504 (Lambda-X, Nivelles, Belgium).
Table 2 Subjective response variables and the corresponding questions asked
Using a Nikon SLR camera (NIKON FS-3V; Nikon Corporation, Tokyo, Japan) mounted on a slit lamp, photos of the contact lens position post-settling time were taken in straight-ahead gaze at each visit. A custom-written Matlab software was used to determine the amount of x- and y-contact lens decentration with respect to the pupil center. Positive numbers indicate nasal and superior decentration, while negative numbers indicate temporal and inferior decentration. The exact details of this measurement procedure have been explained previously.Citation35
Analysis
Data were summarized as mean ± standard deviation for variables measured on an interval scale. Performance variables (HCVA, questionnaire ratings), pupil size, and contact lens centration data were compared between lenses using linear mixed model with subject random intercepts after adjusting for visits. The interaction of lenses with visit was also tested. Post hoc multiple comparisons were adjusted using Bonferroni correction. Analyses were performed separately for the two groups. Level of statistical significance was set at 5%. Analysis was performed using SPSS 21 (IBM Corporation, Armonk, NY, USA).
Results
A total of 52 participants were enrolled into the study and 40 participants completed each stage of the trial. Thirty-five participants (67%) were female (female: Group 1: N=15 (58%), Group 2: N=20 (77%); P=0.139), the mean age was 21.4±2.0 years (Group 1: 21.3±2.0 years, Group 2: 21.5±2.1 years; P=0.742), and the mean spherical equivalent obtained via subjective refraction was −2.82±0.89 D (Group 1: −2.92±0.92 D, Group 2: −2.72±0.87 D; P=0.418). There were no significant differences between the groups (P=0.193) or the lens types (P=0.731) with respect to the days the lenses were worn at each of the three follow-up visits. On average, the lenses were worn for 3.8±2.1 days at the first interim visit, for 5.3±2.1 days at the second interim visit, and for 9.0±2.4 days at the final visit.
shows the results for binocular and monocular HCVAs as measured with the different lenses of each group at each of the four visits. When compared to all four MFCLs, significantly better results were achieved with the control lens, ie, Lotrafilcon B SV (P<0.05). Omafilcon A MFCL D was the test lens with the overall best HCVA (P<0.05). Group standard deviations were highest for measurements obtained with Omafilcon A MFCL N. Over time, no significant differences (P>0.05) were found between the four visits in both groups for binocular HCVA and in Group 2 for monocular HCVA. There were also no interactions (P>0.05) between lens types and visits. However, there was a significant improvement in monocular HCVA over time with the Omafilcon A MFCL N lens, which was as great as 0.10 logMAR between the dispensing visit and the final visit.
Table 3 Binocular and monocular high-contrast visual acuity (logMAR) as measured with the different lenses at all visits
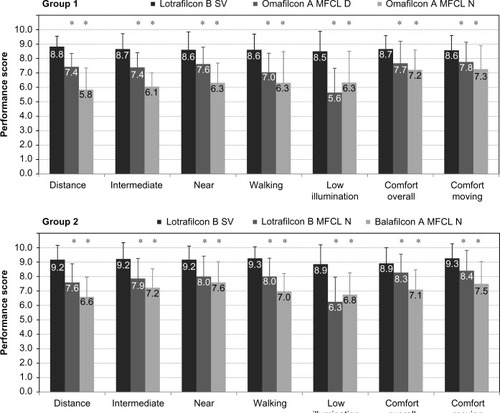
No statistically significant differences were found for any of the subjective ratings between the visits (P>0.05). shows the mean scores for the ratings obtained on final visit of lens wear in both groups. When compared to control, all MFCLs performed significantly worse in all subjective ratings. Among all the MFCLs, the Lotrafilcon B MFCL N lens achieved the overall highest ratings and Omafilcon A MFCL N was the overall worst performing lens. Based on paired differences to the control lens, Lotrafilcon B MFCL N lens was rated significantly higher than Omafilcon A MFCL N for distance, intermediate and near (P<0.05).
Figure 2 Mean scores for the subjective responses obtained on the final visit of lens wear.
Abbreviations: SV, single vision; MFCL, multifocal soft contact lens; D, center-distance; N, center-near.
The mesopic pupil sizes with MFCLs were not significantly different from those obtained with the SV lens (P>0.05). This observation was noticed in both the groups. In Group 1, patients wearing Lotrafilcon B SV, Omafilcon A MFCL D, and Omafilcon A MFCL N had average pupil sizes of 4.7±1.1, 5.2±1.3, and 4.9±1.0 mm, respectively. While in Group 2, patients wearing Lotrafilcon B SV, Lotrafilcon B MFCL N, and Balafilcon A MFCL N were found to have average pupil sizes of 4.4±1.1, 4.5±0.9, and 4.6±0.8 mm, respectively.
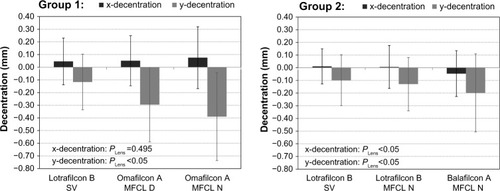
shows the average contact lens centration data for the different lens types. While there were no significant differences in Group 1 with respect to x-centration of the lens, in Group 2, the Balafilcon A MFCL N lens was slightly but significantly decentered toward the temporal side (x=−0.05 mm, P<0.05) when compared to the control (x=0.01 mm). With the exception of the Lotrafilcon B MFCL N lens (P>0.05), all other test lenses were significantly inferiorly decentered (P<0.05), when compared to the control. On average, the greatest y-decentration of −0.39 mm was observed for the Omafilcon A MFCL N lens. Linear mixed model showed no significant differences (P>0.05) between visits in terms of contact lens position, and there were also no interactions between lens types and visits. All subjective ratings showed a small but significant positive correlation (r>0.10, P<0.05) with y-decentration, indicating a decrease in visual performance as y-decentration became more negative.
Figure 3 Contact lens centration data (average of four visits).
Abbreviations: SV, single vision; MFCL, multifocal soft contact lens; D, center-distance; N, center-near.
The power profiles of the different study lenses are shown in , indicating the greatest power variations across the optic zone for the Omafilcon A MFCLs. lists the fourth-order polynomials that were fitted to the power profiles and the calculated corresponding areas under the distance labeled power profiles between the half chords of 0.00 and 3.00 mm. Although the greatest plus area under the distance labeled power profile was found with the Omafilcon A MFCL N lens, the area of the Lotrafilcon B MFCL N lens comprised the least plus power of all MFCLs.
Figure 4 NIMO power profile measurements for all study lenses (distance power label −3.00 D, high add).
Abbreviations: SV, single vision; MFCLD, multifocal soft contact lens center-distance; MFCLN, multifocal soft contact lens center-near.
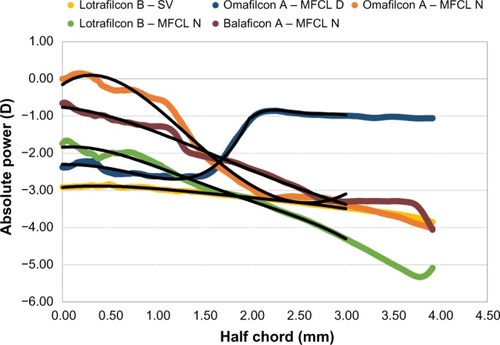
Table 4 Fourth-order polynomial fits for the different study lenses and the calculated area under the distance corrected power profiles between the half chords of 0.00 and 3.00 mm
Discussion
The current study showed that for the HCVAs and subjective visual performance variables, the SV control lens was superior when compared to the four MFCLs (one MFCL D and three MFCL N designs). Similarly, previous studies in non-presbyopesCitation25–Citation27 also reported some reduction in vision with MFCLs but the results differed between MFCL D and MFCL N designs. Specifically, when testing a concentric bifocal lens with a central distance zone (Acuvue Bifocal), the study by Shah and GundelCitation27 found a significant reduction in low-contrast VA, but not in HCVA when compared to an SV lens. Likewise, Kollbaum et alCitation26 reported good HCVA but reduced visual quality ratings with the two test lenses, as both featured a central distance zone. Conversely, with MFCL N designs, Montés-Micó et alCitation25 found a significant reduction in high-contrast VA when compared to an SV lens. In agreement with previous studies, a better HCVA was also achieved with the MFCL D lens (Omafilcon A MFCL D) used in the current study when compared to the three MFCL N lenses. The findings on good HCVA with MFCL D lenses can primarily be explained by the fact that it is easier to resolve fine details at distance with a central distance zone lens than when using the peripheral distance zone of a center-near lens. Nevertheless, the overall best performing lens with respect to the subjective response ratings (distance, intermediate, and near) was a center-near lens, ie, the Lotrafilcon B MFCL N lens. This suggests that good distance visual acuity alone does not necessarily imply good overall visual performance in non-presbyopes.
The differences in overall visual performance between the lenses can mainly be attributed to the power profile differences between the lenses and the magnitude of the plus area under the distance labeled power profiles. While the power profiles of the Omafilcon A MFCL D lenses show a distinct jump in the power profile, a more gradual and smooth power transition across the optical zone occurs with the Lotrafilcon B MFCL N and the Balafilcon A MFCL N lenses.Citation11 As noted previously,Citation28 the greater the refractive power variations across the optical zone, the greater the magnitudes of higher-order aberrations and, thus, the impact of ghosting. The level of ghosting not only depends on the lens design (ie, power profiles), but also on the near add power, pupil size, and contact lens centration.Citation28 The latter factor is supported by the findings of the current study, as Lotrafilcon B MFCL N subjectively performed the best and was the only lens not significantly decentered when compared to the control. On the contrary, Omafilcon A MFCL N was the worst performing and most inferiorly decentered lens. Significant inferior contact lens decentration with Omafilcon A MFCLs has been reported previouslyCitation28,Citation35 and may be due to a general looser fit with those lenses. It has been shown that a significant decentration can lead to an increase in odd higher-order aberrations,Citation28 which could have adversely affected the visual performance. Overall, the results of the current study suggest that MFCLs with the greatest refractive power variations across the optical zone, and/or being significantly decentered, resulted in the lowest overall visual performance in non-presbyopic myopic eyes. These findings should be kept in mind when practitioners attempt to fit non-presbyopes with MFCLs.
Finally, the current study is the first study to concomitantly report assessment of visual performance changes with MFCLs over time in myopic non-presbyopes. Unlike the study with presbyopes by Papas et al,Citation36 which reported a significant reduction in subjective vision responses over 4 days of MFCL wear, no significant changes in the subjective performance variables were found over a minimum of 8 days of lens wear with the multifocal lenses used in the current study. However, a clinically and statistically signifi-cant improvement in monocular distance HCVA was achieved with the Omafilcon A MFCL N lens, which is in agreement with the study by Fernandes et al,Citation22 who assessed the same lens design in presbyopes over 15 days of lens wear. It is possible that the size of the plus area under the distance labeled power profile required more time from the participant to adapt to this lens type.
The exact duration needed for a complete neuroadaptation to MFCLs has been debated for decades. The opinions vary from a few days to several weeks;Citation22,Citation36,Citation37 however, recent data on presbyopic individuals suggest that 3–4 days of MFCL wear should be sufficient.Citation36,Citation37 However, all the studies investigating adaptation with MFCLs were done on presbyopes. Our current findings from a non-presbyopic sample suggest that the adaptation, if any, would occur in a couple of days. It is worthwhile to note that despite the fact that some adaptation effect was found for monocular HCVA with the Omafilcon MFCL N lens, there was no change in any of the subjective performance variables with this or any other test lens. This constant subjective performance suggests that over time improvement in HCVA perhaps did not impact the participants’ daily visual tasks. Based on this observation, and as reported previously,Citation26,Citation28,Citation36 subjective measures appear to be more realistic indicators for the assessment of visual performance with MFCLs, when compared to acuity-based measures.
Conclusion
MFCLs with greatest power variation across the optic zone, a greater plus area under the distance labeled power profile, and/or lenses that were significantly decentered resulted in the lowest subjective ratings. Over time, quality of vision with MFCLs did not change in non-presbyopic myopic participants, with the exception of Omafilcon A MFCL N, which showed some adaptation effects.
Acknowledgments
This work was carried out at the clinics and laboratories of the Brien Holden Vision Institute, Sydney, Australia. The research was fully funded by the Brien Holden Vision Institute. The authors would like to acknowledge the clinical team (Ms Robertson, Ms Crompton, Ms Chung, and Mr Ozkan) and the database management team (Dr Naduvilath and Ms Laarakkers) for their invaluable support to run the study at the Clinical Trial Research Centre, Brien Holden Vision Institute, Sydney, Australia. Authors would like to extend their thanks to Dr Flanagan for reviewing the manuscript and to Dr Kim for measuring the power profiles of the study lenses.
Disclosure
The Brien Holden Vision Institute receives royalties from the sale of Lotrafilcon B MFCL N. The authors report no other conflicts of interest in this work.
References
- Bar DayanYLevinAMoradYThe changing prevalence of myopia in young adults: a 13-year series of population-based prevalence surveysInvest Ophthalmol Vis Sci2005462760276516043848
- PereraSAWongTYTayWTFosterPJSawSMAungTRefractive error, axial dimensions, and primary open-angle glaucoma: the Singapore Malay Eye StudyArch Ophthalmol201012890090520625053
- WongTYKleinBEKleinRTomanySCLeeKERefractive errors and incident cataracts: the Beaver Dam Eye StudyInvest Ophthalmol Vis Sci2001421449145411381046
- BabaTOhno-MatsuiKFutagamiSPrevalence and characteristics of foveal retinal detachment without macular hole in high myopiaAm J Ophthalmol200313533834212614751
- GwiazdaJEHymanLNortonTTAccommodation and related risk factors associated with myopia progression and their interaction with treatment in COMET childrenInvest Ophthalmol Vis Sci2004452143215115223788
- GwiazdaJThornFBauerJHeldRMyopic children show insufficient accommodative response to blurInvest Ophthalmol Vis Sci1993346906948449687
- MuttiDOMitchellGLHayesJRAccommodative lag before and after the onset of myopiaInvest Ophthalmol Vis Sci20064783784616505015
- AbbottMLSchmidKLStrangNCDifferences in the accommodation stimulus response curves of adult myopes and emmetropesOphthalmic Physiol Opt19981813209666906
- GambraESawidesLDorronsoroCMarcosSAccommodative lag and fluctuations when optical aberrations are manipulatedJ Vis200994
- TheagarayanBRadhakrishnanHAllenPMCalverRIRaeSMO’LearyDJThe effect of altering spherical aberration on the static accommodative responseOphthalmic Physiol Opt200929657119154282
- WagnerSConradFBakarajuRCFedtkeCEhrmannKHoldenBPower profiles of single vision and multifocal soft contact lensesCont Lens Anterior Eye20143821425139719
- SmithEL3rdKeeCSRamamirthamRQiao-GriderYHungLFPeripheral vision can influence eye growth and refractive development in infant monkeysInvest Ophthalmol Vis Sci2005463965397216249469
- MuttiDOHayesJRMitchellGLRefractive error, axial length, and relative peripheral refractive error before and after the onset of myopiaInvest Ophthalmol Vis Sci2007482510251917525178
- AnsticeNSPhillipsJREffect of dual-focus soft contact lens wear on axial myopia progression in childrenOphthalmology20111181152116121276616
- LamCSTangWCTseDYTangYYToCHDefocus Incorporated Soft Contact (DISC) lens slows myopia progression in Hong Kong Chinese schoolchildren: a 2-year randomised clinical trialBritish Journal of Ophthalmology201498404524169657
- SankaridurgPHoldenBSmithE3rdDecrease in rate of myopia progression with a contact lens designed to reduce relative peripheral hyperopia: one-year resultsInvest Ophthalmol Vis Sci2011529362936722039230
- WallineJJGreinerKLMcVeyMEJones-JordanLAMultifocal contact lens myopia controlOptom Vis Sci2013901207121424061152
- EdwardsMHLiRWLamCSLewJKYuBSThe Hong Kong progressive lens myopia control study: study design and main findingsInvest Ophthalmol Vis Sci2002432852285812202502
- GwiazdaJHymanLHusseinMA randomized clinical trial of progressive addition lenses versus single vision lenses on the progression of myopia in childrenInvest Ophthalmol Vis Sci2003441492150012657584
- LeungJTBrownBProgression of myopia in Hong Kong Chinese schoolchildren is slowed by wearing progressive lensesOptom Vis Sci19997634635410416928
- HasebeSNakatsukaCHamasakiIOhtsukiHDownward deviation of progressive addition lenses in a myopia control trialOphthalmic Physiol Opt20052531031415953115
- FernandesPRNevesHILopes-FerreiraDPJorgeJMGonzalez-MeijomeJMAdaptation to multifocal and monovision contact lens correctionOptom Vis Sci20139022823523376896
- AllerTAWildsoetCBifocal soft contact lenses as a possible myopia control treatment: a case report involving identical twinsClin Exp Optom20089139439918601670
- WallineJJMcVeyLMyopia control with a soft bifocal contact lensOptom Vis Sci201188395403
- Montés-MicóRMadrid-CostaDRadhakrishnanHCharmanWNFerrer-BlascoTAccommodative functions with multifocal contact lenses: a pilot studyOptom Vis Sci201188998100421552179
- KollbaumPSJansenMETanJMeyerDMRickertMEVision performance with a contact lens designed to slow myopia progressionOptom Vis Sci20139020521423376894
- ShahASGundelRLow-contrast visual acuity measurements in single-vision and bifocal soft lens wearersInt Cont Lens Clin200027119123
- FedtkeCBakarajuRCEhrmannKChungJThomasVHoldenBVisual performance of single vision and multifocal contact lenses in non-presbyopic myopic eyesCont Lens Anterior Eye201639384626228543
- PlainisSAtchisonDACharmanWNPower profiles of multifocal contact lenses and their interpretationOptom Vis Sci2013901066107723995515
- BakarajuRCEhrmannKHoAPapasEInherent ocular spherical aberration and multifocal contact lens optical performanceOptom Vis Sci2010871009102221037495
- PlainisSNtzilepisGAtchisonDACharmanWNThrough-focus performance with multifocal contact lenses: effect of binocularity, pupil diameter and inherent ocular aberrationsOphthalmic Physiol Opt201333425023199097
- GuiraoAWilliamsDRCoxIGEffect of rotation and translation on the expected benefit of an ideal method to correct the eye’s higher-order aberrationsJ Opt Soc Am A20011810031015
- CharmanWNWalshGRetinal image quality with different designs of bifocal contact lensTransactions BCLA1986
- EhrmannKFedtkeCRadicAAssessment of computer generated vision chartsCont Lens Anterior Eye20093213314019362877
- BakarajuRCFedtkeCEhrmannKHoAComparing the relative peripheral refraction effect of single vision and multifocal contact lenses measured using an autorefractor and an aberrometer: A pilot studyJ Optom20158320621825662364
- PapasEBDecenzo-VerbetenTFonnDUtility of short-term evaluation of presbyopic contact lens performanceEye Contact Lens20093514414819421021
- WoodsJWoodsCFonnDVisual Performance of a Multifocal Contact Lens versus Monovision in Established PresbyopesOptom Vis Sci20159217518225525891
