Abstract
The syndesmosis is an important fibrous joint that plays a crucial role in normal ankle weight-bearing and movements. Syndesmosis injuries include disruption of one or more of the ligaments comprising the distal tibiofibular syndesmosis and are commonly associated with ankle fractures. The treatment of grade 1 syndesmosis injury should be conservative, such as immobilization for one to three weeks followed by gradual return to activity. For the treatment of grade 2 syndesmosis injury, if it was stable enough, the patients still could be managed with conservative therapies. But majority of them strongly favor surgical treatment. For the treatment of grade 3 syndesmosis injury, it should treat with surgical reconstruction. If syndesmosis injury is associated with ankle fractures, surgical reduction, fixation, and reconstruction are usually required. Common surgical treatment methods include syndesmosis screws, composed of either metallic or bioabsorbable material; fibula intramedullary nails; and dynamic button-suture fixation, TightRope or ZipTight. Each method has advantages and disadvantages which must be considered while determining which treatment will provide the best outcomes depending on the patient’s needs. Continued exploration of new materials, devices, and methods for surgical fixation is necessary for advancement in this field.
Introduction
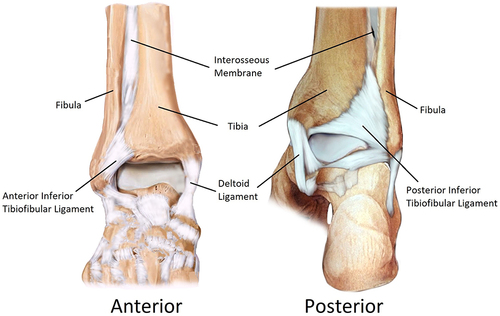
Located at the distal union of the tibia and fibula, the tibiofibular syndesmosis is tasked with maintaining the stability of the ankle joint. A syndesmosis is a fibrous joint formed by adjacent bones bound together by membrane. The tibiofibular syndesmosis is composed of four primary structures, the anterior inferior tibiofibular ligament, posterior inferior tibiofibular ligament, the transverse ligament, and the interosseous membrane (). The anterior tibiofibular ligament is located superiorly to the anterior mortise of the ankle joint and runs posteroinferiorly from the tibia to the fibula. The posterior tibiofibular ligament is located superior to the posterior mortise and runs anteroinferiorly from the tibia to the fibula. The transverse ligament is located posteriorly and runs horizontally from the tibia to fibula. The interosseous membrane spans the space between the tibia and fibula and extends the majority of the length of the 2 bones, eventually blending into the anterior and posterior tibiofibular ligaments.
Figure 1 Illustration of the normal tibiofibular syndesmosis which is composed of four primary ligaments: the interosseous membrane, the transverse ligament, the anterior inferior tibiofibular ligament, and posterior inferior tibiofibular ligament.
The tibiofibular syndesmosis is sturdy yet flexible, allowing for a degree of motion and elasticity during ambulation. When the ankle is dorsiflexed and under tension from external rotational forces, the syndesmosis is at a high risk of rupture. An injury to the tibiofibular syndesmosis, also known as a high ankle sprain, is composed of damage to at least one of the structures four components in combination with a rupture of the deltoid ligament or a fracture of the tibia or fibula.Citation1 Ankle fractures are the fourth most prevalent form of fracture in the United States, trailing only distal radius ulna fractures, metacarpal fractures, and proximal femur fractures in prevalence. There were 444,909 instances of ankle fractures in the US population in 2016 occurring at a rate of 137.7 cases/100,000 people. Trans-syndesmotic fractures accounted for about two-thirds of all ankle fractures with 292,750 cases in 2016.Citation1 Isolated syndesmosis injuries account for 5% of all ankle injuries.Citation2 However, recent studies have shown that during collision sports in which force from contact may be applied to the ankle, syndesmotic injuries account for a greater share of total ankle injuries. High-intensity athletic activity accounts for 46 to 75% of all syndesmotic ankle injuries.Citation3 Achieving a timely diagnosis, administering the correct means of treatment, and managing associated risk factors are essential to maximizing the odds of positive outcomes in patients suffering from these injuries. The consequences of failure to recognize a syndesmotic injury may lead to instability, joint pain, degeneration of the articular surface, and premature osteoarthritis.
Pathophysiology of Syndesmotic Injury
The most common mechanism of injury to the tibiofibular syndesmosis is an external rotational force applied to a planted dorsiflexed foot.Citation4 Less frequently, abduction, eversion, or hyperdorsiflexion of the ankle may cause injury. In all cases, the lateral force applies tension to the syndesmosis by pressing the talus against the distal fibula with the significance of injury directly related to the amount of force applied.Citation5 In progression from least to most significant syndesmotic ankle injuries, a tear of the anterior inferior tibiofibular ligament is the least significant injury, followed by a tear of the interosseous membrane, and rarely a tear of the posterior inferior tibiofibular ligament.Citation4 If the damage caused by force is great enough, the deltoid may be damaged independently or in conjunction with a spiral fracture of the proximal fibula.Citation5 Frequently, syndesmosis injury may be accompanied by fibular fractures due to the external force of rotation, the most common associated fractures include Weber B, Weber C, and Maisonneuve fractures.Citation6
Diagnosis of Syndesmosis Injury
Identifying a syndesmosis ankle injury is critical for developing a treatment plan to maximize the probability of a positive recovery. Diagnosis of tibiofibular syndesmosis injury involves clinical evaluation confirmed by imaging. Differentiating between different types of ankle sprains is typically done through a multifaceted approach beginning with localizing symptoms at the first presentation. Clinical exams may reveal sensitive signs of injury with tenderness during palpation of the anterior surface of the ankle typically felt over the interosseous membrane, anterior inferior tibiofibular ligament, or posterior inferior tibiofibular ligament. A positive result may be found during testing dorsiflexion and external rotation of the foot. Patients usually present with ankle instability, pain during weight bearing over the anterior distal portion of the tibia and fibula, and medial ankle joint pain.Citation7 Swelling and bruising are less common in syndesmosis injuries than would be seen with lateral and medial ankle sprains.Citation8 Specific signs of injury may be tested by examining if the patient is unable to execute a single-leg hop or from a squeeze test. If any of these exams yield a positive result, obtain ankle radiographs to rule out the possibility of fracture. In the case that fracture is not present but there is diastasis, the patient may be referred to an orthopaedic surgeon for a grade 3 syndesmotic injury.Citation9 If neither fracture nor diastasis is observed, a grade 1 or grade 2 syndesmotic injury may be present and ultrasound imaging should be procured to determine the extent of tendon injury.Citation10 If a partial anterior inferior tibiofibular ligament is observed on ultrasound, a grade 1 syndesmotic injury is present and may be approached with nonoperative treatment. If a complete anterior inferior tibiofibular ligament tear is observed on ultrasound, a grade 2 syndesmotic injury is present and referral to an orthopaedic surgeon is necessary. When ultrasound imaging is unavailable, patients should immobilize the joint, follow-up with a referral to orthopaedic surgery, and obtain imaging from MRI.Citation6
Classification of Syndesmosis Injury
Tibiofibular syndesmosis injuries without fractures are primarily classified based on the graded ankle sprain. The graded ankle sprain system considers cause of injury, stability of the joint, and involvement of ligament damage for grading. The grade 1 injury has partial tearing of anterior inferior tibiofibular ligament, with no diastasis on image studies. It considered a stable injury. The grade 2 injury has complete tear of anterior inferior tibiofibular ligament and partial tear of interosseous membrane, without diastasis seen on image studies. It considered a potentially unstable injury. The grade 3 injury usually has complete tear of the anterior inferior tibiofibular ligament and the interosseous membrane plus partial or complete tear of the posterior inferior tibiofibular ligament, usually with diastasis of the syndesmosis and/or complete deltoid ligament rupture. It clearly considered an unstable injury. If the tibiofibular syndesmosis injury is also associated with fracture, the Danis–Weber and Lauge-Hansen classification systems are the preferred method used for the classification. The Lauge-Hausen system classifies fractures according to their radiographic appearance and mechanism of injury. It is a simple system for the classification of lateral malleolar fractures, which is based on comparing the level of the fracture in relation to the ankle joint, specifically the distal tibiofibular syndesmosis. The Danis-Weber system classifies fractures based upon the location and appearance of the fibular injury.Citation11,Citation12
Treatment of Syndesmosis Injury
The treatment of grade 1 syndesmosis injury should be conservative, such as immobilization for one to three weeks followed by gradual return to activity. For the treatment of grade 2 syndesmosis injury, if it was stable enough, the patients still could be managed with conservative therapies. But majority of them strongly favor surgical treatment. For the treatment of grade 3 syndesmosis injury, it should treat with surgical reduction, fixation and reconstruction.
Syndesmotic injuries with fracture of the fibula or posterior malleolus require surgical treatment stabilization. Less commonly, isolated with complete syndesmotic disruption requires surgery to improve short- and long-term outcomes.
Reduction of the syndesmosis is the greatest clinical predictor for post-recovery outcome. With surgical intervention, there is a risk for unplanned reoperations that may occur as frequently as in 27% of cases.Citation13 The most common causes for secondary operation are misdiagnosed syndesmotic injuries, failure to achieve anatomic reduction, and loss of reduction due to failure of the fixation device.
There are currently static and dynamic methods of surgical revision that may be used for stabilization. The primary goal of both treatment methods is to return the ankle to its original anatomical structure. Restoring anatomical stability allows for the syndesmosis to properly heal.Citation13 Reducing the fibula in the fibular notch is the first step in avoiding posttraumatic arthritis.Citation14 The severity of the syndesmosis injury will determine or direct the methods of reduction and reconstruction of the syndesmosis. Acute grade 2 or grade 3 injuries should undergo surgery to reduce the syndesmosis and stabilize the joint through dynamic or static fixation with cortical screws, bolt and hook, suture buttons, or intramembranous fibular nails.Citation14 The surgical approach used should be determined by the surgeon and patient preferences based off condition and comorbidities. Subacute and chronic injuries are treated differently through surgery. Acute injuries will typically be repaired through ligament reconstruction and syndesmosis fixation.Citation15 Chronic injuries are usually treated with syndesmotic fusion.Citation16 A post-surgery rehabilitation plan should be implemented with physical therapy to improve outcome results.
The preferred method of care for tibiofibular syndesmotic injuries is static fixation with a trans-syndesmotic screw. The screw may be composed of metallic or bioabsorbable material, which is developed from material that will be absorbed into the structure of the body throughout the healing process. Screws may vary in size to allow for the accommodation of different positions and needs of treatment. Drawbacks accompany the high levels of invasiveness the placement of screws require. Increased risk of complications from infection, delayed union, and nonunion in patients with comorbidities must be considered while deciding to implement this form of treatment.Citation17 Six to eight weeks of immobilization and non-weight-bearing are typically required before a second operation is needed to remove the syndesmosis screw. During this time, there is a risk of recurrence of the diastasis and fracture of the screw due to force.Citation17 Biodegradable implants remove the need for a secondary operation to remove implanted devices. Biodegradable screws are promising and frequently used for fixation but are limited by being less mechanically stable than their metallic counterparts. Premature degradation of implants is believed to be responsible for malunion in nearly 26% of cases with high rates of osteolysis and sterile wound sinuses.Citation18
Intramedullary fibular nails are a static fixation option in the surgical repair of syndesmotic ankle injuries. Reaming of the nail canal is an invasive process after which the ankle requires immobilization and for the ankle to be held non-weight bearing before a second operation for removal.Citation16 A secondary surgery poses a risk for recurrence of diastasis and infection, which must be considered while determining a course of treatment in patients with comorbidities.
Dynamic fixation using an implanted suture-button device, or TightRope or ZipTight fixation, may offer some benefits over static fixation options such as syndesmosis screws or intramembranous fibular nails. With dynamic fixation, patients have a reduced risk of pain from the implanted device and a decreased chance of recurrent diastasis.Citation16 Patients may begin to ambulate without the need of a second surgery for removal of the device. With the implant of a suture-button device, a screw is placed in the tibiotalar joint 2 to 4 cm above the tibial plafond.Citation16 The placement and angle of the screw allow for proper fixation of the fibula. The screw should be implanted, while the foot is dorsiflexed so that the anterior talus widens the ankle mortise and avoids impairment. Recently, suture-button techniques using a trans-syndesmotic fiber wire have been used for surgical stabilization in substitution for trans-syndesmotic screws. The primary benefit of this dynamic fixation technique is that it allows for reduction while maintaining movement between the tibia and fibula. Drawbacks to this procedure have been seen due to a lack of distal fibula fixation function. An invasive surgical procedure must be undergone for the implantation of a required fibula plate fixation in conjunction with suture-button implants, increasing the risk of complications from infection and delayed union.Citation15
The goal of treatment should be to restore stability, mobility, and strength while minimizing the risk of negative consequences. Until recently, instability has been treated primarily with static fixation methods such as trans-syndesmotic screws. More recently, dynamic fixation techniques like suture-button have become increasingly prominent due to advantages in post-surgery weight bearing ambulation and the avoidance of follow-up procedures. The decision to use either static or dynamic fixation techniques must be determined by the physician and patient to accommodate for the needs of care and the risk of comorbidities. Weightbearing may be achieved in a shorter time period through the use of dynamic fixation compared to static fixation. It is typically recommended to be between 6 and 8 weeks before weightbearing is resumed after a static fixation procedure, which is similar to the time needed to regain mobility with dynamic fixation.Citation17 The true benefit of dynamic procedures is allowed freedom of motion and the avoidance of a second procedure to remove the dynamic suture-button, as is required with a static screw.Citation19 Because of this, suture-button devices may be safer in patients at-risk of complications from additional surgical procedures.Citation15,Citation19 However, suture-button devices are associated with an increased risk of neurovascular bundle entrapment, infections caused by the fiber wire, and osteomyelitis.Citation18 Pain and irritation have been found similar in both static and dynamic procedures. The risks and benefits of different surgical approaches must be weighed while determining treatment.
In conclusion, the tibiofibular syndesmosis is an important fibrous joint that plays a key role in ankle normal weight bearing and movements. Syndesmosis injuries include disruption of one or more of the ligaments comprising the distal tibiofibular syndesmosis and are also commonly associated with ankle fractures. Surgical treatments are usually required to restore stability. Currently, common surgical treatment methods include syndesmosis screws, composed of either metallic or bioabsorbable material; fibula intramedullary nail; and a dynamic button-suture fixation, TightRope or ZipTight. Each method has its own advantages and disadvantages which should be considered while determining which treatment or treatments should be used depending on the individual patient’s needs. Continued exploration of new materials, devices, and methods is necessary in this field.
Disclosure
The authors report no conflicts of interest in this work.
Additional information
Funding
References
- Rockwood CA, Green DP, Robert W. Rockwood and Green’s Fractures in Adults. 6th ed. Philadelphia: Lippincott Williams & Wilkins; 2006.
- Signs & Symptoms. Syndesmosis Sprain of the Ankle. Available from: http://syndesmosis.weebly.com/signs--symptoms.html. Accessed April 12, 2022.
- Prakash AA. Epidemiology of high ankle sprains: a systematic review. Foot Ankle Spec. 2020;13(5):420–430. doi:10.1177/1938640020916266
- Boytim MJ, Fischer DA, Neumann L. Syndesmotic ankle sprains. Am J Sports Med. 1991;19(3):294–298. doi:10.1177/036354659101900315
- Hopkinson WJ, St Pierre P, Ryan JB, Wheeler JH. Syndesmosis sprains of the ankle. Foot Ankle. 1990;10(6):325–330. doi:10.1177/107110079001000607
- Porter DA, Jaggers RR, Barnes AF, Rund AM. Optimal management of ankle syndesmosis injuries. Open Access J Sports Med. 2014;5:173–182. doi:10.2147/OAJSM.S41564
- de-Las-Heras Romero J, Alvarez AML, Sanchez FM, et al. Management of syndesmotic injuries of the ankle. EFORT Open Rev. 2017;2(9):403–409. doi:10.1302/2058-5241.2.160084
- Gan K, Zhou K, Hu K, Lu L, Gu S, Shen Y. Dynamic fixation versus static fixation for distal tibiofibular syndesmosis injuries: a meta-analysis. Med Sci Monit. 2019;25:1314–1322. doi:10.12659/MSM.913324
- Michelson JD, Magid D, McHale K. Clinical utility of a stability-based ankle fracture classification system. J Orthop Trauma. 2007;21(5):307–315. doi:10.1097/BOT.0b013e318059aea3
- Calder JD, Bamford R, Petrie A, McCollum GA. Stable versus unstable grade II high ankle sprains: a prospective study predicting the need for surgical stabilization and time to return to sports. Arthroscopy. 2016;32(4):634–642. doi:10.1016/j.arthro.2015.10.003
- Molloy A, Selvan D. Ligamentous injuries of the foot and ankle. In: Thompson SR, editor. DeLee & Drez’s Orthopaedic Sports Medicine Principles and Practice. 4th ed. Philadelphia: Elsevier Saunders; 2015:1392.
- Miller MD, Thompson SR, DeLee J, Drez D. DeLee & Drez’s orthopaedic sports medicine: principles and practice; 2015. Available from: http://www.mdconsult.com/books/about.do?eid=4-u1.0-B978-1-4557-4376-6.C2011-0-06696-6--TOP&isbn=978-1-4557-4376-6&about=true&uniqId=449996769-20. Accessed April 12, 2022.
- Skeletal Trauma. Available from: https://www.med-ed.virginia.edu/courses/rad/ext/8ankle/01anatomy.html. Accessed April 12, 2022.
- Stiene A, Renner CE, Chen T, Liu J, Ebraheim NA. Distal tibiofibular syndesmosis dysfunction: a systematic literature review of dynamic versus static fixation over the last 10 years. J Foot Ankle Surg. 2019;58(2):320–327. doi:10.1053/j.jfas.2018.08.050
- Liu J, Pathak G, Joshi M, Andrews K, Lee J. A meta-analysis comparing the outcomes of syndesmotic injury treated with metal screw, dynamic fixation, and bioabsorbable screw. J Pediatr Orthop. 2021;25:82–87. doi:10.1016/j.jor.2021.04.006
- Lee JS, Curnutte B, Pan K, Liu J, Ebraheim NA. Biomechanical comparison of suture-button, bioabsorbable screw, and metal screw for ankle syndesmotic repair: a meta-analysis. Foot Ankle Surg. 2021;27(2):117–122. doi:10.1016/j.fas.2020.03.008
- Ebraheim NA, Vander Maten JW, Delaney JR, White E, Hanna M, Liu J. Cannulated intramedullary screw fixation of distal fibular fractures. Foot Ankle Spec. 2019;12(3):264–271. doi:10.1177/1938640018790082
- Ebraheim NA, Dailey M, Huff S, Qu Y, White E, Liu J. Minimal invasive fixation can decrease infection rates in diabetic and obese patients with severe ankle fracture and syndesmotic injury. Foot Ankle Spec. 2019;12(1):62–68. doi:10.1177/1938640018766627
- Bafna KR, Jordan R, Yatsonsky D 2nd, Dick S, Liu J, Ebraheim NA. Revision of syndesmosis screw fixation. Foot Ankle Spec. 2020;13(2):138–143. doi:10.1177/1938640019843328
