Abstract
Objective
To evaluate the expressions of circulating angiogenic factors affected by pamidronic acid (PA) intravenous infusion in bone metastatic breast cancer patients and the impact on their prognosis.
Methods
Peripheral blood of ten bone metastatic breast cancer patients was collected for serum insulin-like growth factor-1 (IGF-1) and platelet endothelial cell adhesion molecule-1 expression detection just before and 2 days after PA infusion.
Results
Both IGF-1 and platelet endothelial cell adhesion molecule-1 concentrations decreased after PA treatment for 48 hours (P<0.05). Modification was defined as >20% decrease recorded 2 days after PA administration. The decrease of IGF-1 was more significant in breast cancer patients who had received previous hormonotherapy. Moreover, the progression-free survival of first-line chemotherapy treatment of IGF-1 modified patients was longer than that of IGF-1 unmodified patients (P=0.009).
Conclusion
PA treatment could suppress circulating serum IGF-1 and platelet endothelial cell adhesion molecule-1 concentrations; moreover, the prognosis of patients in IGF-1 unmodified group was relatively poor.
Introduction
Bone tissue is one of the most common sites in malignant tumor distant metastasis. It is particularly common in patients with breast cancer; the incidence rate of bone metastasis in metastatic breast cancer patients is ~65%–75%, among which the proportion of bone metastasis as the first symptom is 27%–50%, including bone pain, pathological fracture, hypercalcemia, spinal cord, or nerve root compression syndromes.Citation1
Bisphosphonates (BPs) are well established for the treatment and prevention of the skeletal-related events of breast cancer patients with bone metastases. BPs have been shown to reduce and delay skeletal-related events as well as to improve patients’ quality of life. Recent studies have shown that BPs might also act as a potential inhibitor of tumor angiogenesis by affecting the vascular endothelial growth factor (VEGF).Citation2–Citation4
Insulin-like growth factor-1 (IGF-1) is known to stimulate neovascularization by inducing factors, such as VEGF.Citation5,Citation6 Activation of IGF-1 receptor (IGF-1R)-mediating signaling in breast cancer cells promotes cell proliferation, invasion, and migration, suggesting that IGF-1/IGF-1R plays an important role in tumor angiogenesis.
Moreover, platelet endothelial cell adhesion molecule-1 (PECAM-1/CD31), a cell adhesion molecule with proangiogenic and proinflammatory activity, plays an important role in the process of angiogenesis. It is reported that there is a correlation between microvessel density and VEGF expression in many cancers.Citation7,Citation8
Santini et alCitation9 proved that pamidronic acid (PA) could downregulate circulating VEGF concentrations in vivo. His research team also showed that zoledronic acid, a potent third-generation BP, induced greater suppression of VEGF concentrations in cancer patients with metastatic bone disease.Citation10 Despite evidence on the fall of VEGF concentration after administration of BP in treatment-naïve patients, however, there is no literature about the effects of BP treatment on serum (IGF-1and PECAM-1) expression.
Therefore, the purpose of this study was to investigate the effect of PA treatment on serum IGF-1 and PECAM-1 of patients with breast cancer who had progressive osseous metastases.
Materials and methods
Patients and study design
Ten female patients with advanced breast cancer who were treated during March 2013–September 2014 at the Zhejiang Cancer Hospital were included in this study.
Eligibility criteria
Eligibility criteria included stage IV bone metastatic female breast cancer patients, 18 years of age or older; a performance status not >2 on the Eastern Cooperative Oncology Group scale; a life expectancy of >3 months; and adequate organ function, including neutrophil count >1.5×109/L, platelet count >100×109/L, normal hepatic and renal function (Cr ≤265 μmol/L, CrCl ≥30 mL/min), electrolytes within the normal range, and no acute or chronic infections or inflammatory diseases. Moreover, a negative pregnancy test was necessary for females in childbearing age. Diagnosis of bone metastases had to include the use of X-ray, CT scan, or MRI. No antitumor therapy for these patients was permitted within 28 days before PA administration.
Exclusion criteria
Patients were excluded from study participation for any of the following reasons: history of other malignancy (unless >5 years disease-free) excluding completely resected nonmelanoma skin cancer; active or uncontrolled infection; concurrent active dental problems, including infection of the teeth (maxillary or mandibular), dental trauma, or a concurrent or prior diagnosis of osteonecrosis of the jaw; recent (within 6 weeks) or planned dental or jaw surgery; history of uncontrolled or symptomatic angina, arrhythmias, or congestive heart failure; previous treatment with any BPs within 1 month before study initiation; known hypersensitivity to BPs; history of treatment with calcitonin, gallium nitrate, or mithramycin within 28 days before study; or pregnancy or lactation in potentially eligible women.
The study was approved by the medical ethics committee of Zhejiang Cancer Hospital, Hangzhou. Written informed consent was obtained from all patients prior to enrollment. The trial is registered through the Hospital Pharmaceutical Research Fund Project of Zhejiang Provincial Pharmaceutical Association, number 2011ZYY05.
Group
According to the reduction in IGF-1 circulating levels, it was defined as modified when at least a 20% reduction was recorded 2 days after PA administration, otherwise as unmodified.
Treatment and sample collection
PA was administered on an outpatient basis.
All patients received 45 mg of PA infusion in 100 mL of 0.9% saline intravenously over a period of 3 hours for 2 days. Peripheral venous blood samples (5 mL) were collected prior to PA infusion and 48 hours after infusion. After collection, the blood samples were kept at room temperature for 30 minutes to allow clotting, and then were immediately centrifuged at 3,000× g for 5 minutes. Serum samples were aliquoted and stored at −80°C until detection.
Biochemical markers
Serum levels of IGF-1 and PECAM-1 were assayed using a solid-phase sandwich enzyme-linked immunosorbent assay (Quantikine Immunoassays; R&D Systems, Inc., Minneapolis, MN, USA). The assay was performed according to the manufacturer’s instructions. Each serum sample was analyzed in duplicate.
Statistical analysis
The follow-up period was defined as the time from diagnosis to the last visit/observation or death. Progression-free survival was defined as the time between the date of the time from randomization until patient’s tumor progression or death. The log-rank test was used to estimate and compare survival. All statistical analyses were carried out on an intention-to-treat basis using the SPSS 15.0 software package (SPSS Inc., Chicago, IL, USA).
As the angiogenic cytokine levels were not normally distributed, data were summarized by median and range. The nonparametric test (Wilcoxon test) was used to assess differences among groups.
Results
Patient characteristics
summarizes the characteristics of patients evaluated in this study. The number of advanced breast cancer patients enrolled was ten, with a median age of 41 years (range 33–60). At baseline, ten patients were treated with pamidronic for 2 days. Nine patients (90.0%) had ductal breast carcinoma, and only three patients (30%) were postmenopausal. Eight patients (80.0%) had hormone receptor-positive breast cancer, and the other two patients (20.0%) had hormone receptor-negative breast cancer. No patients were ever-smokers and two patients (20%) had drinking history. Most of the patients (90%) had a reproductive history. Two patients (20%) had diabetes mellitus, and four (40%) patients had other underlying disease (mainly hypertension, cardiac disease, and hepatitis).
Table 1 Patient characteristics
Further, three (30%) patients had adjuvant radiotherapy, five (50%) patients had adjuvant chemotherapy, and five (50%) patients had adjuvant hormonotherapy. In five patients, bone was the only site of metastatic disease, whereas three patients had lung metastases and three patients had liver metastases. Advanced metastases: at the time of initial visits, before treatment, there were metastatic lesions. Recurrent metastases: metastasis occurred after treatment.
Serum angiogenic cytokine levels analysis
The number of patients who had a reduction in the circulating IGF-1 and PECAM-1 levels after PA infusion is sum-marized in . The mean ± standard deviation baseline IGF-1 and PECAM-1 concentration for the ten patients was 1,370.0±523.3 and 5,478.7±2,655.2 pg/mL, respectively. The median IGF-1 and PECAM-1 values showed a decrease of 22.6% and 30.0%, respectively, 2 days after the first infusion of PA, and these reductions were both statistically significant (P<0.05).
Table 2 Serum angiogenic cytokine levels before and after the 2-day pamidronic acid intravenous infusion
Patient characteristics according to IGF-1 modifications
Reduction in IGF-1 circulating levels was defined as >20% decrease recorded 2 days after PA administration. Ten patients were separated into two groups: six patients (60%) in whom there occurred at least 20% reduction in IGF-1 serum levels after PA infusion for 2 days were classified as the reduced IGF-1 group, and the other four patients (40%) were entered in the unmodified IGF-1 group.
All the patient characteristics according to IGF-1 modifications are summarized in . It is suggested that compared to IGF-1 unmodified patients, IGF-1 modified patients might benefit from the adjuvant hormonotherapy. Further multivariate analysis confirmed that adjuvant hormonotherapy history is a favorable factor contributing to IGF-1 modifications ().
Table 3 Patient characteristics according to IGF-1 modifications
Table 4 Multivariate analysis of factors for IGF-1 modifications
The impact of IGF-1 modification on patients’ prognosis
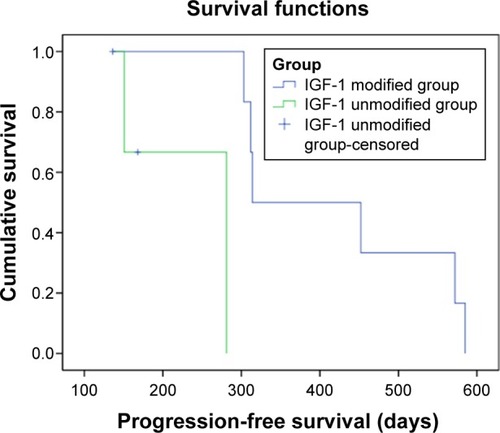
By the follow-up time of March 10, 2016, two patients had died. Both patients belonged to the IGF-1 unmodified group. Though the mortality between IGF-1 modified group and IGF-1 unmodified group had no statistical significance (P=0.053), it still had a certain value for treatment consideration. Further, the progression-free survival of subsequent first-line chemotherapy treatment in IGF-1 modified patients was longer than that of IGF-1 unmodified patients (P=0.009), indicating that the prognosis of patients in IGF-1 unmodified group was relatively poor ().
Discussion
The results of this study suggest that PA treatment could suppress circulating serum IGF-1 and PECAM-1 concentrations, and the prognosis of patients in IGF-1 unmodified group was relatively poor; moreover, previous hormonotherapy may improve patients’ responses to BP therapy in IGF-1 modification. PA, a kind of nitrogen-containing BP that inhibits the activity of farnesyl diphosphate synthase, is a key enzyme in the mevalonate pathway. Apart from anti-resorptive activity, PA has been reported to suppress tumor angiogenesis in animal models.Citation11 These findings, together with reports that PA modified circulating angiogenic factors in metastatic cancer patients, suggest its potential role in antitumor angiogenesis.Citation9
Numerous studies have suggested that IGF-1/IGF-1R- mediated activation of downstream signaling pathways plays an important part in progression of breast cancer.Citation12–Citation14 Tang et alCitation15 demonstrated that PA and clodronate functionally inhibited both in vitro and in vivo tumor angiogenesis induced by IGF-1-stimulated MCF-7 cells.
As we know, tumor angiogenesis is affected by the activity of multiple, rather than single, angiogenesis stimulators.Citation16
PECAM-1 is a molecule expressed on all cells within the vascular compartment; apart from exhibiting adhesive properties, PECAM-1 is also an efficient signaling molecule and is now known to have diverse roles in vascular biology, including roles in angiogenesis, platelet function, thrombosis, and so on.Citation17 XuCitation18 suggest that PECAM-1, VEGF, and microvessel density play roles in oncogenesis and progression of renal cell carcinoma. There is a significant correlation among abundant PECAM-1, VEGF, and microvessel density in renal cell carcinoma, and PECAM-1 and VEGF may be important targets for antiangiogenesis therapy in patients with renal cell carcinoma.
In our study, the results suggested that PA might have potential antiangiogenic properties and exhibits adhesive property in bone metastatic breast cancer by decreasing the expression of IGF-1 and PECAM-1 concentrations.
Furthermore, we found that the serum concentrations of IGF-1 in breast cancer patients who received adjuvant hormonotherapy were lower than other breast cancer patients. Since the introduction of the molecular subtypes of breast carcinoma in 2000, breast cancer has been classified based on gene expression profiling into five subtypes, including: luminal A, luminal B, Her-2, triple negative basal-like, and triple negative without basal-like markers.Citation19 About 80% of breast cancers present an estrogen receptor and/or progesterone receptor expression.Citation20 Numerous studies nowadays report that estrogens cooperate with the IGF system at multiple levels both in physiology and disease. More and more studies have focused on this bidirectional cross-talk in cancers. Notably, cancer cells show frequent deregulation of the IGF system with overexpression of IGF-1R, but frequent upregulation of the classical estrogen receptor.Citation21,Citation22 Above all, the potential effect of PA on IGF-1 in hormone receptor-positive breast cancer patients deserves more attention.
In conclusion, the present data reveal that the antiangiogenic effect of PA might act through a double blocking mechanism by downregulation of IGF-1 and PECAM-1 expression. Moreover, the prognosis of patients in IGF-1 unmodified group was relatively poor. However, there are some limitations in this investigation. First, the detection points after PA treatment, of this study are not sufficient, and the compliance management of patients who participated in the study needs to be strengthened. Second, the number of patients included was small since the number of patients who met the inclusion criteria was small. Third, this is a single-center investigation. Thus, future clinical trials with large population, and more detection points, in multicenters should be designed to evaluate the efficacy of PA, as well as other BPs, used as an antiangiogenic drug in bone metastatic breast cancer patients.
Acknowledgments
This work was sponsored by 1022 Talent Training Program of Zhejiang Cancer Hospital, Hospital Pharmaceutical Research Fund Project of Zhejiang Provincial Pharmaceutical Association (2011ZYY05), General Research Program of Medical Health in Zhejiang Province (No 2014KYB039), Scientific Research Fund Project of Integrated Chinese and Western Medicine Institute in Zhejiang Province (2014LYK021), Science and Technology in Zhejiang Province Chinese Medicine Program (2012ZA101, 2015ZA148, 2016ZA038), Hangzhou City Science and Technology Project Planning Guide (Social Development) (20130733Q15), Hangzhou City Health Science and Technology Project (2013A43), and Public Welfare Technology Application Studies Program of Zhejiang (2015C33286).
Disclosure
The authors report no conflicts of interest in this work.
References
- JemalASiegelRWardECancer statistics, 2008CA Cancer J Clin2008582719618287387
- MathewABrufskyABisphosphonates in breast cancer: a triple winner?Oncology (Williston Park)2015291373925595284
- WoodJBonjeanKRuetzSNovel antiangiogenic effects of the bisphosphonate compound zoledronic acidJ Pharmacol Exp Ther200230231055106112183663
- ReusserNMDaltonHJPradeepSClodronate inhibits tumor angiogenesis in mouse models of ovarian cancerCancer Biol Ther20141581061106724841852
- SachdevDYeeDDisrupting insulin-like growth factor signaling as a potential cancer therapyMol Cancer Ther20076111217237261
- SaxenaNKTaliaferro-SmithLKnightBBBidirectional crosstalk between leptin and insulin-like growth factor-I signaling promotes invasion and migration of breast cancer cells via transactivation of epidermal growth factor receptorCancer Res200868239712972219047149
- CaoGO’BrienCDZhouZInvolvement of human PECAM-1 in angiogenesis and in vitro endothelial cell migrationAm J Physiol Cell Physiol20022825C1181C119011940533
- DelisserHMChristofidou-SolomidouMStrieterRMInvolvement of endothelial PECAM-1/CD31 in angiogenesisAm J Pathol199715136716779284815
- SantiniDVincenziBAvvisatiGPamidronate induces modifications of circulating angiogenic factors in cancer patientsClin Cancer Res2002851080108412006522
- SantiniDVincenziBHannonRAChanges in bone resorption and vascular endothelial growth factor after a single zoledronic acid infusion in cancer patients with bone metastases from solid tumoursOncol Rep20061551351135716596210
- SoltauJZirrgiebelUEsserNAntitumoral and antiangiogenic efficacy of bisphosphonates in vitro and in a murine RENCA modelAnticancer Res2008282A93394118507039
- de OstrovichKKLambertzIColbyJKParacrine overexpres-sion of insulin-like growth factor-1 enhances mammary tumorigenesis in vivoAm J Pathol2008173382483418688034
- MoschosSJMantzorosCSThe role of the IGF system in cancer: from basic to clinical studies and clinical applicationsOncology200263431733212417786
- SachdevDYeeDThe IGF system and breast cancerEndocr Relat Cancer20018319720911566611
- TangXZhangQShiSBisphosphonates suppress insulin-like growth factor 1-induced angiogenesis via the HIF-1a/VEGF signaling pathways in human breast cancer cellsInt J Cancer20101269010319569175
- PavlakovicHHaversWSchweigererLMultiple angiogenesis stimulators in a single malignancy: Implications for anti-angiogenic tumour therapyAngiogenesis20014425926212197470
- GlenKLuuNTRossEModulation of functional responses of endothelial cells linked to angiogenesis and inflammation by shear stress: differential effects of the mechanotransducer CD31J Cell Physiol201222762710272121898411
- XuYStudy on the Expression and Relationship of PECAM-l/VEGF in Renal Cell Carcinoma [master’s thesis]TianjinTianjin Medical University2009
- PerouCMSørlieTEisenMBMolecular portraits of human breast tumoursNature2000406679774775210963602
- SotiriouCNeoSYMcShaneLMBreast cancer classification and prognosis based on gene expression profiles from a population-based studyProc Natl Acad Sci U S A200310018103931039812917485
- BartellaVDe MarcoPMalaguarneraRBelfioreAMaggioliniMNew advances on the functional cross-talk between insulin-like growth factor-I and estrogen signaling in cancerCell Signal20122481515152122481093
- SamoliELagiouAZournaPExpression of estrogen receptors in non-malignant mammary tissue modifies the association between insulin-like growth factor 1 and breast cancer riskAnn Oncol201526479379725542925