Abstract
Drug delivery system based on nanobiotechnology can improve the pharmacokinetics and therapeutic index of chemotherapeutic agents, which has revolutionized tumor therapy. Onivyde, also known as MM-398 or PEP02, is a nanoliposomal formulation of irinotecan which has demonstrated encouraging anticancer activity across a broad range of malignancies, including pancreatic cancer, esophago-gastric cancer, and colorectal cancer. This up-to-date review not only focuses on the structure, pharmacokinetics, and pharmacogenetics of Onivyde but also summarizes clinical trials and recommends Onivyde for patients with advanced solid tumors.
Introduction
Irinotecan (CPT-11) is a semisynthetic derivative of camptothecin which targets topoisomerase I, and is currently used in the treatment of multiple solid tumors, such as metastatic colorectal cancer (mCRC), small-cell lung cancer, non-small-cell lung cancer, gastric cancer, and cervical cancer.Citation1–Citation4 The pharmacology of irinotecan is complicated, with extensive metabolic conversions involved in the activation, inactivation, and elimination.Citation5–Citation7 Irinotecan as a prodrug is converted by nonspecific carboxylesterases into SN-38, which is a 100- to 1,000-fold more active metabolite.Citation7,Citation8 SN-38 is glucurono-conjugated in the liver, and this metabolite, although inactive, may participate in the enterohepatic cycling of SN-38 after hydrolysis in the intestinal lumen.Citation9 The SN-38 metabolite is cleared by the biliary route after glucuronidation by uridine diphosphate-glucuronosyltransferase 1A1 (UGT1A1). UGT1A1 activity exhibits a wide intersubject variability, in part related to UGT1A1 gene polymorphisms. Patients homozygous for the UGT1A1*28 allele are at increased risk of developing hematological and/or digestive toxicities.Citation10 However, hydrolysis of active lactone rings in irinotecan and SN-38 to inactive carboxylate forms occurs in normal physiologic pH.Citation11 The clinical disadvantage of irinotecan includes acute toxicities, fast elimination of the drug, and risk of diarrhea and neutropenia as the major dose-limiting toxicities (DLTs).Citation7,Citation8 These properties of the drug contribute to the limitation of its clinical application. Hence, the rationally designed drug delivery system (DDS) represents a strategy to improve the pharmacokinetics and biodistribution of irinotecan while protecting it from premature metabolism and extending the time of its exposure at the site of action. Advances in nanotechnology have revolutionized medicines, especially for tumor therapy. Nano-DDS is capable of passive drug delivery through the enhanced permeability and retention (EPR) effect or active targeting via binding to receptors associated with the tumor, thus improving the pharmacokinetics and therapeutic index of chemotherapeutic agents.Citation12–Citation16 Due to the perfect biocompatibility, liposome-based drug carrier has become a favorable DDS for various purposes.Citation7,Citation8 For example, liposomal doxorubicin, and particularly pegylated liposomal doxorubicin, has shown significant pharmacologic advantages and an added clinical value over doxorubicin.Citation17
Onivyde, also known as MM-398 or PEP02, has been designed and developed as a nanoliposomal formulation of irinotecan, which improves the pharmacokinetics of the drug by increasing drug encapsulation and loading efficiency, protecting the drug in the active lactone configuration, prolonging circulation time, providing sustained release, rerouting the drug from sites of toxicity such as the gastrointestinal tract, increasing tumor accumulation via the EPR effect, and reducing host toxicity.Citation7,Citation8 Based on the encouraging preclinical and clinical data available for the treatment of a variety of solid tumors, Onivyde was newly approved by the US Food and Drug Administration (FDA) in October 2015 as a combination regimen for patients with gemcitabine-based chemotherapy-resistant metastatic pancreatic cancer. In addition, it is also currently undergoing Phase II/III clinical trials for the therapy of many cancer types, such as pancreatic cancer, esophago-gastric (OG) cancer, and colorectal cancer.Citation18–Citation21 These clinical trials demonstrate that Onivyde has potential antitumor activity across a broad range of advanced solid tumors.Citation7,Citation8,Citation18–Citation21
In this review, the structure, pharmacokinetics, and pharmacogenetics of Onivyde are addressed. Clinical trials are also summarized, and recommendations are made for Onivyde for patients with advanced pancreatic cancer and other cancer types.
Structure
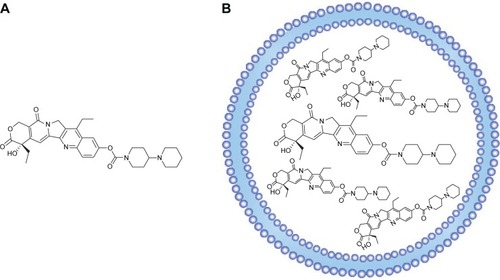
Molecular formula of irinotecan is C33H38N4O6, and chemical formula is 7-ethyl-10-[4-(1-piperidino)-1-piperidino] carbonyloxycampothecin, which is shown in . Onivyde, the nanoliposomal formulation of irinotecan, employs a modified gradient-loading method using sucrose octasulfate with unprecedented drug-loading efficiency and in vivo drug stability.Citation7 schematically illustrates the structure of Onivyde.
Pharmacokinetics
The pharmacokinetics of nanoliposomal CPT-11 formulated using either TEA-SOS or TEA-Pn was determined in normal female rats, which is summarized in .Citation7 Nanoliposomal CPT-11 was associated with significantly longer circulation times and less rapid clearance from the blood than free CPT-11. What is more, to define pharmacokinetics of Onivyde in human, a total of eleven patients were randomized into three dose levels – 60 (one patient), 120 (six patients), and 180 mg/m2 (four patients) – in a study by Chang et al.Citation22 The formulation of Onivyde may modify the pharmacokinetic parameters of irinotecan and SN-38 by liposomal encapsulation. Comparing with the pharmacokinetics after free irinotecan injection, the dose-normalized pharmacokinetics of SN-38 following Onivyde administration was characterized by lower maximum plasma concentration (Cmax), prolonged terminal half-life (t1/2), and higher area under curve (AUC), although with significant interindividual variation. The Cmax, terminal t1/2, and AUC of SN-38 after administration of 120 mg/m2 of Onivyde were 9.2±3.5 ng/mL, 75.4±43.8 hours, and 710±395 ng⋅h/mL, respectively. Slow clearance is also an advantage of Onivyde.Citation23 The levels of CPT-11 and SN-38 following Onivyde administration were persistent and remained in circulation for over 50 hours, whereas the CPT-11 and SN-38 in the plasma were cleared rapidly from circulation within 8 hours after free irinotecan injection.
Table 1 Pharmacokinetic variables for free and nanoliposomal CPT-11 in rats
Pharmacogenetics
Genetic polymorphisms affect toxicity and efficacy of irinotecan, and a pharmacogenetic study showed that a patient with a combined heterozygous genotype of UGT1A1*6/*28 had significantly higher Cmax and AUC levels of SN-38 after Onivyde administration.Citation22 In another study, in the group administered with Onivyde, the frequency of grade 3–4 neutropenia was higher among UGT1A1*6 heterozygotes compared with those with wild-type genotype (40% [two out of five] for heterozygotes vs 3% [one out of 30] for wild type, P=0.0220).Citation18 Patients with combined heterozygous genotype of UGT1A1*6/*28 had severe toxicity leading to death.
Preclinical research
In a series of preclinical studies, Onivyde demonstrated significantly superior anticancer efficacy when compared to free irinotecan in multiple cell lines and xenograft models, including colorectal, gastric, breast, cervical, pancreatic, and lung cancer and glioma, as well as Ewing’s sarcoma family of tumors.Citation7,Citation8,Citation23 At the equivalent dose, free irinotecan showed massive tumor progression, while Onivyde showed enhanced antitumor efficacy.Citation7,Citation8,Citation23 The striking antitumor activity in the majority of xenograft models showed with Onivyde was significantly correlated with its advantageous pharmacokinetic properties, by which Onivyde achieved higher intratumoral levels of the prodrug irinotecan and its active metabolite SN-38 compared with free irinotecan. Thus, the enhanced accumulation of the active metabolite within the tumor microenvironment could safely improve its antitumor activity with low systemic toxicity.
Clinical trials of Onivyde for the therapy of multiple solid tumors
The efficacy of Onivyde for the therapy of a variety of solid tumors has been investigated in several clinical trials, including various Phase I, II, and III studies on registry, which are summarized in .
Table 2 Characteristics of the clinical trials of Onivyde for the treatment of multiple solid tumors
Phase I
In the first-in-human Phase I trial, eleven patients with advanced refractory solid tumors were enrolled to determine the maximum tolerated dose (MTD), DLT, safety profile, pharmacokinetic variables, and antitumor activity of Onivyde.Citation22 The MTD of Onivyde monotherapy at 3-week interval was 120 mg/m2, which was the recommended dose for future studies. Myelosuppression and diarrhea were the major DLTs. The toxicity pattern was comparable with that of free-form irinotecan, and the most common toxicity observed in the six patients at the MTD dose level (120 mg/m2) was diarrhea (100% in all grades, 33% in grade 3–4) and vomiting (83.3% in all grades, 66.7% in grade 3–4). In addition, promising antitumor activities from Onivyde were observed in the patients who were refractory to currently available treatments. Among them, two patients achieved partial response, one with pancreatic cancer who failed several lines of treatment including gemcitabine and 5-fluorouracil/leucovorin (5-FU/LV) alone or in combination with oxaliplatin, and the other with cervical cancer whose tumor relapsed after cisplatin-based concurrent chemoradiotherapy. Another three patients with breast cancer, pancreatic neuroendocrine tumor, and thymic carcinoma had stable disease. The disease control rate was 45.5% for intent-to-treat patients.
Phase II
Onivyde for locally advanced or metastatic gastric or OG junction adenocarcinoma
OG cancer represents a significant global health problem with an estimated one million cases diagnosed every year in the world.Citation18 There may be clinical remission or disease stabilization in advanced OG cancer patients who receive first-line chemotherapy; however, most will ultimately experience disease progression, and thus, effective second-line chemotherapy is essential.Citation24 However, currently, there are no standard second-line treatments in this setting.Citation25,Citation26 Therefore, novel and more effective treatment options are urgently needed to provide survival benefit for patients with advanced OG cancer. Fortunately, the novel liposomal nanocarrier formulation of irinotecan, Onivyde, is a new therapy option providing hope for patients with advanced OG cancer who failed one prior chemotherapy regimen. In a randomized three-arm Phase II study (NCT00813072), Roy et al evaluated the efficacy and safety of single-agent Onivyde compared with irinotecan or docetaxel in the second-line treatment of advanced OG cancer.Citation18 In this trial, patients with locally advanced/metastatic OG cancer who had failed one prior chemotherapy regimen were randomly divided into three groups: Onivyde 120 mg/m2, irinotecan 300 mg/m2, and docetaxel 75 mg/m2 every 3 weeks. The primary end point was objective response rate (ORR). The secondary end points included progression-free survival (PFS), overall survival (OS), and 1-year survival rate. The outcomes demonstrated that the ORR for Onivyde, irinotecan, and docetaxel was 13.6% (6/44; 95% confidence interval [CI]: 5.2–27.4), 6.8% (3/44; 95% CI: 1.4–18.7), and 15.9% (7/44; 95% CI: 6.6–30.1), respectively. The ORR associated with Onivyde was comparable with docetaxel and numerically greater than that of irinotecan. The median overall survival (mOS) and median progression-free survival (mPFS) were similar in all the three arms. The mOS for Onivyde, irinotecan, and docetaxel was 7.3 (95% CI: 3.84–9.17), 7.8 (95% CI: 4.90–9.20), and 7.7 months (95% CI: 5.32–12.32), respectively. The mPFS was 2.7 (95% CI: 1.54–3.65), 2.6 (95% CI: 1.48–4.34), and 2.7 months (95% CI: 1.41–5.45), respectively. Kaplan–Meier estimates of 1-year survival rates were 21.3%, 30.8%, and 40.4%, respectively, in those three treatment arms. Treatment was well tolerated, and Onivyde was associated with an increased frequency of grade 3–4 diarrhea (27.3% in Onivyde group vs 18.2% in irinotecan group) and nausea, with similar rates of vomiting, neutropenia, and febrile neutropenia compared with irinotecan and docetaxel. These results illustrated that Onivyde is well tolerated and also has a comparable efficacy to docetaxel and irinotecan in patients with locally advanced or metastatic OG cancer, who failed first-line treatment.
Onivyde for mCRC
Colorectal cancer ranks as the third most common cancer worldwide as approximately one million new cases are diagnosed annually.Citation3,Citation27,Citation28 Chemotherapeutic agents are widely used for patients with mCRC to prolong survival, control symptoms, and improve the quality of life. Irinotecan is one of the key drugs used for the management of mCRC, along with oxaliplatin.Citation28 These drugs are often combined with 5-FU/LV in regimens such as FOLFIRI (irinotecan, 5-FU, and LV) or FOLFOX (oxaliplatin, 5-FU, and LV), which have exhibited clinical effects and considerably improved OS in patients with mCRC in recent decades.Citation3,Citation27,Citation28 In a randomized noncomparative Phase II study (NCT01375816), Chibaudel et al evaluated Onivyde or irinotecan in combination with 5-FU/LV as second-line therapy in patients with mCRC who had failed one prior oxaliplatin-based first-line therapy.Citation19 In the trial, 55 patients were randomly assigned to FUPEP (n=28, Onivyde + 5-FU/LV) or FOLFIRI (n=27, irinotecan + 5-FU/LV). Bevacizumab q2w (5 mg/kg) was allowed in both arms. The primary end point was ORR. The outcomes demonstrated that in the evaluable population (n=50), ORR was 16.7% (n=4/24) and 11.5% (n=3/26) in the FUPEP and FOLFIRI arms, respectively. Most common grade 3–4 adverse events reported in the respective FUPEP and FOLFIRI arms were diarrhea (21% vs 33%), neutropenia (11% vs 30%), mucositis (11% vs 11%), and alopecia (G2: 25% vs 26%). Hence, Onivyde may provide a new second-line treatment option for mCRC.
Onivyde for gemcitabine-refractory metastatic pancreatic cancer
Pancreatic cancer is well recognized as an extremely challenging disease on multiple fronts, which is characterized by late detection, poor prognosis, and aggressive metastasis.Citation29,Citation30 Early detection is uncommon with no >15%–20% of the patients being amenable for curative intent surgery at the time of diagnosis.Citation12 Even in these cases, 5-year overall survival is still only 22%. Systemic chemotherapy based on gemcitabine is the popular regimen for patients with advanced pancreatic cancer, the mOS of whom is generally ~6 months.Citation12,Citation31 For pancreatic cancer, irinotecan has not been considered as a clinically useful drug. However, since Conroy et alCitation32 demonstrated that FOLFIRINOX regimen consisting of oxaliplatin, irinotecan, and 5-FU/LV could provide significantly better ORR, PFS, and OS than gemcitabine monotherapy in patients with metastatic pancreatic cancer, irinotecan-included therapy has been receiving increased attention for advanced pancreatic cancer.Citation33 However, notably and not unexpectedly, this triplet regimen is often hindered by the significant toxicity. Fortunately, the novel nanoliposomal formulation of irinotecan, Onivyde, could present safe therapeutic option. In an international, multicenter, open-label, Phase II trial (NCT00813163), Ko et al evaluated Onivyde monotherapy as second-line treatment for patients with gemcitabine-based chemotherapy-resistant metastatic pancreatic cancer.Citation20 In the study, a total of 40 patients were enrolled. The primary end point of this trial was 3-month survival rate (OS3-month). Secondary end points included ORR, PFS, clinical benefit response, CA19-9 tumor marker response, and safety profile. Of the 40 treated patients, three patients (7.5%) achieved an objective response, with an additional 17 (42.5%) demonstrating stable disease for a minimum of two cycles. Ten (31.3%) out of 32 patients with an elevated baseline CA19-9 had a 45% biomarker decline. The study met its primary end point with an OS3-month of 75% and mOS and mPFS of 5.2 and 2.4 months, respectively. The most common severe adverse events included neutropenia (40%), abdominal pain (37.5%), and diarrhea (75%). These results illustrated that Onivyde showed moderate antitumor activity with a manageable side effect profile in patients with metastatic, gemcitabine-refractory pancreatic cancer.
Phase III
As illustrated, Onivyde provides a new treatment option and a new hope for patients with gemcitabine-based chemotherapy-resistant metastatic pancreatic cancer. Further study was carried out. A randomized, open-label, Phase III trial by Von Hoff et al investigated Onivyde, with or without 5-FU/LV, vs 5-FU/LV, in patients with metastatic pancreatic cancer progressed on or following gemcitabine-based therapy (NCT01494506).Citation21 Patients with metastatic pancreatic cancer after gemcitabine-based therapy were randomized 1:1:1 to receive (A) Onivyde, (B) 5-FU/LV, or (C) combination of Onivyde and 5-FU/LV. The primary end point was OS in arms A and C, each vs the control arm B. The outcomes demonstrated that OS, PFS, ORR, and time to failure were significantly improved by Onivyde + 5-FU/LV compared with 5-FU/LV. mOS was 6.1 months (95% CI: 4.8–8.9) in the Onivyde + 5-FU/LV arm and 4.2 months (95% CI: 3.3–5.3) in the 5-FU/LV arm (hazard ratio [HR] =0.67, P=0.012). mPFS was 3.1 (95% CI: 2.7–4.2) and 1.5 months (95% CI: 1.4–1.8), respectively (HR =0.56, P<0.001). Onivyde alone did not demonstrate a statistical improvement in efficacy compared with 5-FU/LV. The most common grade >3 toxicities seen with the combination of Onivyde and 5-FU/LV were neutropenia (14.5%), fatigue (13.7%), diarrhea (12.8%), and vomiting (11.1%). Given the excellent results obtained in the Phase III trial, the FDA newly approved Onivyde + 5-FU/LV regimen for patients with gemcitabine-based chemotherapy-resistant metastatic pancreatic cancer. An updated analysis of OS, 6- and 12-month survival estimates, and safety was presented in the 2016 Gastrointestinal Cancers Symposium, San Francisco, CA, USA. Onivyde + 5-FU/LV (n=117) retained an OS advantage relative to 5-FU/LV (n=119): 6.2 (95% CI: 4.8–8.4) vs 4.2 months (95% CI: 3.3–5.3) with an unstratified HR of 0.75 (P=0.0417). Six-month survival estimates were 53% (95% CI: 44%–62%) for Onivyde + 5-FU/LV vs 38% (95% CI: 29%–47%) for 5-FU/LV; 12-month survival estimates were 26% (95% CI: 18%–35%) for Onivyde + 5-FU/LV vs 16% (95% CI: 10%–24%) for 5-FU/LV.Citation34
Ongoing trials
Currently, there are also multiple ongoing clinical trials investigating antitumor efficiency of Onivyde. For example, a Phase I study which explores Onivyde + cyclophosphamide in pediatric solid tumors is underway in the South Plains Oncology Consortium (NCT02013336). A randomized, open-label, Phase II study of Onivyde-containing regimens vs nab-Paclitaxel + gemcitabine in patients with previously untreated, metastatic pancreatic adenocarcinoma is actively recruiting (NCT02551991). A study of liposomal irinotecan and veliparib in treating patients with solid tumors that are metastatic or cannot be removed by surgery is yet to recruit (NCT02631733). A dose escalation study of MM-398 + irinotecan in patients with unresectable advanced cancer is also recruiting (NCT02640365). Activity of MM-398, a nanoliposomal irinotecan (nal-IRI), in Ewing’s family tumor xenografts has been found associated with high exposure of tumor to drug and high SLFN11 expression, which improves antitumor activity compared with the current clinical formulation of irinotecan.Citation8 Other liposomal formulations of irinotecan or SN-38 have also been developed, such as IHL-305 (pegylated liposomal irinotecan) and LE-SN-38 (a liposome-encapsulated SN-38). But PEP02 at 120 mg/m2 showed higher SN-38 exposure than IHL-305 at 160 mg/m2. Notwithstanding the relatively high SN-38 AUC, unfortunately, LE-SN-38 did not meet the prespecified activity criteria in the Phase II CALGB 80402 study on mCRC patients.Citation22
Side effects of Onivyde treatment
Onivyde is generally well tolerated by patients. However, adverse effects also occur, and they are considered manageable. The most frequently observed drug-related adverse events were diarrhea, myelosuppression, vomiting, abdominal pain, asthenia, mucositis, and alopecia.Citation18–Citation22 Management of these toxicities could include antidiarrheal agents, anticholinergic agents, and dose reduction, interruption, or termination.
Conclusion and future directions for drug development
The potential advantages of Onivyde, a novel nanoliposomal formulation of irinotecan, include improvement of pharmacokinetics and biodistribution, extension of the circulation time, increase in passive targeting and tumor accumulation via EPR effect, and reduction in organ toxicity. Onivyde as a promising agent has demonstrated improved outcomes and a tolerable safety profile in the treatment of a variety of tumor types. Since single anticancer agent has not always been sufficiently effective, the combination of Onivyde with conventional cytotoxic agent and/or recently emergent molecular-targeted agent should also be investigated to improve the clinical outcomes. Moreover, the optimal dosages of Onivyde for such combinations remain to be determined. Besides, predictive biomarkers could identify cancer indications and patient populations with an increased likelihood of Onivyde responsiveness and avoid exposure to useless toxic medicine. Thus, additional studies into biomarkers may be useful in predicting personalized therapeutic response.
Acknowledgments
This work was supported by the National Natural Science Foundation of China (81371678).
Disclosure
The author reports no conflicts of interest in this work.
References
- XiaoXGXiaSZouMThe relationship between UGT1A1 gene polymorphism and irinotecan effect on extensive-stage small-cell lung cancerOnco Targets Ther201583575358326664141
- LiuYLuanLWangXA randomized Phase II clinical study of combining panitumumab and bevacizumab, plus irinotecan, 5-fluorouracil, and leucovorin (FOLFIRI) compared with FOLFIRI alone as second-line treatment for patients with metastatic colorectal cancer and KRAS mutationOnco Targets Ther201581061106825999741
- SuenagaMMizunumaNMatsusakaSPhase II study of reintroduction of oxaliplatin for advanced colorectal cancer in patients previously treated with oxaliplatin and irinotecan: RE-OPEN studyDrug Des Devel Ther2015930993108
- RyugeSJiangSXWadaMLong-term disease-free survivor of metastatic large-cell neuroendocrine carcinoma of the lung treated with amrubicin and irinotecanDrug Des Devel Ther20093213217
- Garcia-CarboneroRSupkoJGCurrent perspectives on the clinical experience, pharmacology, and continued development of the camptothecinsClin Cancer Res20028364166111895891
- MathijssenRHvan AlphenRJVerweijJClinical pharmacokinetics and metabolism of irinotecan (CPT-11)Clin Cancer Res2001782182219411489791
- DrummondDCNobleCOGuoZHongKParkJWKirpotinDBDevelopment of a highly active nanoliposomal irinotecan using a novel intraliposomal stabilization strategyCancer Res20066663271327716540680
- KangMHWangJMakenaMRActivity of MM-398, nanoliposomal irinotecan (nal-IRI), in Ewing’s family tumor xenografts is associated with high exposure of tumor to drug and high SLFN11 expressionClin Cancer Res20152151139115025733708
- RivoryLPMetabolism of CPT-11. Impact on activityAnn N Y Acad Sci200092220521511193896
- Etienne-GrimaldiMCBoyerJCThomasFUGT1A1 genotype and irinotecan therapy: general review and implementation in routine practiceFundam Clin Pharmacol201529321923725817555
- AkimotoKKawaiAOhyaKKinetic-studies of the hydrolysis and lactonization of camptothecin and its derivatives, Cpt-11 and Sn-38, in aqueous-solutionChem Pharm Bull (Tokyo)19944221352138
- TsaiCSParkJWChenLTNanovector-based therapies in advanced pancreatic cancerJ Gastrointest Oncol20112318519422811849
- ZhangHMultifunctional nanomedicine platforms for cancer therapyJ Nanosci Nanotechnol20121254012401822852341
- ZhangHWangCChenBWangXDaunorubicin-TiO2 nanocomposites as a “smart” pH-responsive drug delivery systemInt J Nanomedicine2012723524222275838
- ZhangHXiongJGuoLPatelaNGuangXIntegrated traditional Chinese and western medicine modulator for overcoming the multidrug resistance with carbon nanotubesRSC Adv201557128771296
- ZhangHPatelaNXiongJDingSTargeting and noninvasive treatment of hepatocellular carcinoma in situ by ZnO nanorod-mediated concurrent chemoradiotherapyRSC Adv201558572085729
- TahoverEPatilYPGabizonAAEmerging delivery systems to reduce doxorubicin cardiotoxicity and improve therapeutic index: focus on liposomesAnticancer Drugs201526324125825415656
- RoyACParkSRCunninghamDA randomized phase II study of PEP02 (MM-398), irinotecan or docetaxel as a second-line therapy in patients with locally advanced or metastatic gastric or gastro-oesophageal junction adenocarcinomaAnn Oncol20132461567157323406728
- ChibaudelBMaindrault-GoebelFAndréTPEPCOL: a randomized noncomparative phase II study of PEP02 (MM-398) or irinotecan in combination with leucovorin and 5-fluorouracil as second-line therapy in patients with unresectable metastatic colorectal cancer – a GERCOR StudyJ Clin Oncol201533Suppl 3 Abstr 751
- KoAHTemperoMAShanYSA multinational phase 2 study of nanoliposomal irinotecan sucrosofate (PEP02, MM-398) for patients with gemcitabine-refractory metastatic pancreatic cancerBr J Cancer2013109492092523880820
- Von HoffDLiCPWang-GillamANapoli-1: randomized phase 3 study MM-398 (nal-IRI), with or without 5-fluorouracil and leucovorin, versus 5-fluorouracil and leucovorin, in metastatic pancreatic cancer progressed on or following gemcitabine-based therapyAnn Oncol201425Suppl 2ii105ii106
- ChangTCShiahHSYangCHPhase I study of nanoliposomal irinotecan (PEP02) in advanced solid tumor patientsCancer Chemother Pharmacol201575357958625577133
- KalraAVKimJKlinzSGPreclinical activity of nanoliposomal irinotecan is governed by tumor deposition and intratumor prodrug conversionCancer Res201474237003701325273092
- ZhangHApatinib for molecular targeted therapy in tumorDrug Des Devel Ther2015960756081
- WesolowskiRLeeCKimRIs there a role for second-line chemotherapy in advanced gastric cancer?Lancet Oncol200910990391219717092
- LordickFGastrointestinal cancer: salvage chemotherapy in gastric cancer – more than a straw?Nat Rev Clin Oncol20129631231322547215
- LiangRFZhengLLThe efficacy and safety of panitumumab in the treatment of patients with metastatic colorectal cancer: a meta-analysis from five randomized controlled trialsDrug Des Devel Ther2015944714478
- SuenagaMMizunumaNMatsusakaSA phase I/II study of biweekly capecitabine and irinotecan plus bevacizumab as second-line chemotherapy in patients with metastatic colorectal cancerDrug Des Devel Ther2015916531662
- WangCZhangHChenYShiFChenBGambogic acid-loaded magnetic Fe(3)O(4) nanoparticles inhibit Panc-1 pancreatic cancer cell proliferation and migration by inactivating transcription factor ETS1Int J Nanomedicine2012778178722393285
- WangCZhangHChenBYinHWangWStudy of the enhanced anticancer efficacy of gambogic acid on Capan-1 pancreatic cancer cells when mediated via magnetic Fe3O4 nanoparticlesInt J Nanomedicine201161929193521931488
- MooreMJGoldsteinDHammJErlotinib plus gemcitabine compared with gemcitabine alone in patients with advanced pancreatic cancer: a phase III trial of the National Cancer Institute of Canada Clinical Trials GroupJ Clin Oncol200725151960196617452677
- ConroyTDesseigneFYchouMFOLFIRINOX versus gemcitabine for metastatic pancreatic cancerN Engl J Med2011364191817182521561347
- VaccaroVSperdutiIMilellaMFOLFIRINOX versus gemcitabine for metastatic pancreatic cancerN Engl J Med2011365876876921864184
- Wang-GillamALiCPBodokyGPhase III study of nanoliposomal irinotecan (nal-IRI, MM-398), with or without 5-fluorouracil and leucovorin (5-FU/LV), versus 5-FU/LV in metastatic pancreatic cancer (mPAC) previously treated with gemcitabine-based therapyJ Clin Oncol201634Suppl 4S Abstr 417