Abstract
This study aimed to explore the relationship between computed tomography morphology and prognosis of patients with stage I non-small cell lung cancer (NSCLC). From May 2009 to May 2011, a total of 124 patients diagnosed with stage I NSCLC were included. All patients had complete chest computed tomography scans. Five-year follow-up was conducted. Univariate and multivariate Cox regression analyses were performed to estimate the prognostic factors for patients with stage I NSCLC. The 5-year survival rate was 67.74% (84/124). The 5-year survival rates of patients with stage T1a, T1b, and T2a were 89.19%, 75.00%, and 41.86%, respectively. The 5-year survival rates of patients with homogeneity, inhomogeneity, vacuole, and cavity were 68.42%, 72.09%, 59.46%, and 83.33%, respectively. The 5-year survival rates of patients with different margin features were 83.33% (slick margin), 79.73% (lobulation sign), and 39.47% (short burr). The 5-year survival rates of patients with normal, halo, vessel convergence, bronchial transection, and vascular bundle thickening were 84.38%, 72.73%, 71.79%, 52.00%, and 47.06%, respectively. The 5-year survival rates of patients with normal and pleura thickening/indentation were 81.93% and 39.02%. Univariate analysis demonstrated that tumor node metastasis staging, tumor margin, tumor periphery, and pleural invasion were related to the prognosis of stage I NSCLC patients. Cox regression analysis confirmed that T2a stage, pleura thickening/indentation were independent risk factors for poor prognosis of stage I NSCLC. In conclusion, our findings indicate that T2a stage, pleura thickening/indentation might be prognostic factors in stage I NSCLC.
Introduction
Lung cancer, as a malignant disease of heterogeneous nature, is the largest contributor to new cancer diagnosis and the leading cause of cancer-related mortality in China, followed by gastric, liver, and breast cancer.Citation1 It is believed that the development of lung cancer is influenced by factors such as cigarette smoking, secondhand or passive smoking, excessive alcohol consumption, air pollution, occupational carcinogens, and ionizing radiation.Citation2 Clinically, lung cancer can be categorized as small cell lung cancer and non-small cell lung cancer (NSCLC), and the latter accounts for ~75%–80% of lung cancer.Citation3 Interestingly, the incidence and mortality rates of NSCLC are highest in developed countries, and the number of patients dying from NSCLC continues to increase globally.Citation4 Currently, most NSCLC is diagnosed clinically when patients present with symptoms such as persistent hemoptysis, chest pain, low fever, weight loss, anorexia, dyspnea, and emptysis.Citation5 NSCLC patients in the early stages have a 5-year survival rate of 40%–67%, but the key problem is that most NSCLC patients are diagnosed at advanced stages, when potential interventions have limited positive effects on survival outcome and prognosis.Citation6,Citation7 Thus, early diagnosis is critical for advancing the treatment and prognosis of NSCLC.
With the development of medical technologies, great advances have been made in imaging examination technologies and diagnostic workup. Computed tomography (CT) is considered an efficacious method for the diagnosis of asymptomatic patients with recurrent breast cancer, providing earlier diagnosis with complete whole-body staging as a “one-stop shop” procedure.Citation8 Currently, the accuracy of CT screening for early lung cancer detection in heavy smokers is being examined by several randomized trials.Citation9–Citation11 CT is also an important technique to diagnose early peripheral lung cancer.Citation12 Many potential lung cancers develop as small pulmonary nodules that appear as incidental findings on CT scans, and thus surface morphology is a significant indicator of malignant potential for solid-type lung nodules detected by CT.Citation13 In this study, we studied the CT morphological features of patients with stage I NSCLC and analyzed the survival time of patients with different CT morphological features to explore whether CT morphological features can act as prognostic factors for patients with stage I NSCLC.
Materials and methods
Study subjects
From May 2009 to May 2011, a total of 124 stage I NSCLC patients who were admitted to the Department of Radiology, Beijing Friendship Hospital, Capital Medical University, and the Department of Radiology, the Affiliated Hospital of Beihua University, were enrolled in our study. The inclusion criteria were as follows: 1) all patients were confirmed as stage I NSCLC according to the tumor node metastasis (TNM) staging of lung cancer published by the Union for International Cancer Control (UICC) in 2009.Citation14 2) Before operation, conventional chest CT scans, head CT scan/magnetic resonance imaging (MRI), B-ultrasound of the epigastrium and adrenal gland, or CT scan of the epigastrium were performed without observing distant metastasis. 3) Pulmonary status was tolerable for relevant operations as assessed by the lung function test, and no obvious contraindications were noted. 4) There were no postoperative complications, recurrence, metastasis, or death within 1 month after operation. The exclusion criteria were as follows: 1) patients who had received chemoradiotherapy before operation; 2) females who were pregnant or lactating; and 3) patients for whom complete case data were not available. All patients received chest CT scans and had surgical pathology data. There were 66 males and 58 females, with an age range of 27–63 years and a mean age of 46.77±11.12 years. Among these patients, there were 75 cases of adenocarcinoma, 32 of squamous cell carcinoma, 8 of large cell carcinoma, 5 of squamous adenocarcinoma, and 4 of sarcomatoid carcinoma. Therapeutic measures for all patients included standard lobectomy and mediastinal lymph node dissection. According to the TNM staging system published by UICC in 2009, the stage I NSCLC was divided into the IA and IB stages. There were 81 cases in IB stage and 43 cases in IB stage. Stage IA was further subdivided into stage T1a, referring to malignant lesions with a maximum diameter of <2 cm, and stage T1b, referring to malignant lesions with a maximum diameter of 2–3 cm. Stage IB was divided into stage T2a, defined as malignant lesions with a maximum diameter of 3–5 cm, and T2b, in which the malignant lesion impacted the primary bronchi but was >2 cm distant or impacted the visceral pleura. This study was approved by the Ethics Committee of Beijing Friendship Hospital, Capital Medical University, and the Ethics Committee of the Affiliated Hospital of Beihua University. All participants in this study or their families signed written informed consent.
Chest CT scans
A total of 124 patients received conventional chest CT scans. The Siemens Second Generation Somatom Definition Flash CT scanner was selected (Siemens Ltd, Erlangen, Germany). The scanning conditions were as follows: 120 kV tube voltage, 300 mA tube current, 250 mm field of view, 2.0 mm layer thickness, and 2.0/7.0 reconstruction thickness. After scanning, patients remained still, and contrast-enhanced CT scanning was performed. Non-ionic contrast medium (80–100 mL) and normal saline (40 mL) flush were injected into the antecubital vein using a binocular high-pressure syringe at a rate of 4.0 mL/s.
The CT images were independently analyzed by two experienced imaging specialists. Disagreements were resolved by consulting a third specialist or by discussion with the Department of Internal Medicine. The main features of NSCLC on CT imaging referred to density, margin, tumor periphery, and pleural invasion.
Density (four features)
The four features of density are homogeneity, inhomogeneity (calcification or necrosis), vacuole (tumor diameter <5 mm with low-density radiolucent shadow), and cavity (thick-walled cavity and the cavity wall >3.0 mm). The cavity was irregular and off center (or with centrality). The internal wall of the cavity is irregular with nodules. In addition, clear margin, lobulation signs, short burr, no fluid, or a low fluid level (only a few cases showed a large cavity with a high fluid level) were observed on the ektexine.
Tumor margin (three features)
The three features of tumor margin are slick (margin was smooth and clear), lobulation sign (the outline of the tumor was an arc-shaped cylindrical hill encompassing the lobular tumor), and short burr (short and straight fine line shadow existing around the tumor with a width of 1–2 mm and a length of 2–5 mm).
Tumor periphery (five features)
The five features of tumor periphery are normal, halo (ground-glass opacity around the lesion), vessel convergence (vessels around the tumor gathered together and broke at the tumor or penetrated the tumor), bronchial transection (the proliferation of tumor cells formed nodules that violated, oppressed, and pushed the adjacent bronchus, resulting in consecutive transection of the bronchus), and vascular bundle thickening (resulting from the lesion of the bronchus and adjacent pulmonary vessels and mainly formed by the infiltration of tumor cells along the bronchus and mesenchyme around the vessels).
Pleural invasion (two features)
The two features of pleural invasion are normal and pleural thickening and indentation (a malignant tumor presented as infiltrative growth; the shadow of it near the pleura was linear, tentiform or starry; the tumor was linked with the pleura to form an indentation).
Follow-up
Five-year follow-up was conducted on all patients. Based on the time of surgery as the initial period, follow-up ended in May 2016. Patients who were lost to follow-up, who died for other reasons, or who were still alive at the end of follow-up were treated as censored data.
Statistical method
Data analysis was conducted using SPSS 18.0 software (SPSS, Inc., Chicago, IL, USA). Kaplan–Meier survival analysis was used for univariate analysis and tested by log-rank. Multivariate Cox regression analysis was performed to estimate the prognostic factors for patients with stage I NSCLC. Differences were considered significant when P<0.05.
Results
CT morphological features of stage I NSCLC patients
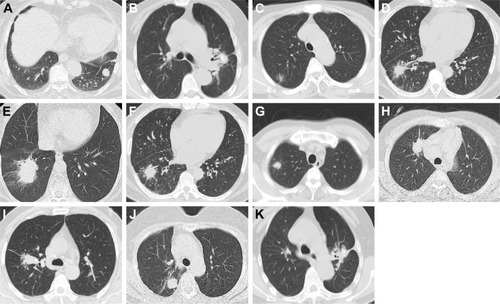
The CT morphological features of 124 patients with stage I NSCLC were analyzed based on 4 aspects: tumor density, margin, tumor periphery, and pleural invasion. The main morphological features are shown in : the lesion in the right lower lobe exhibited homogeneous density and slick and regular margins (); the density of the right lower lobe was heterogeneous, indicating focal necrosis (); vacuoles were observed in the posterior segment lesion of the right upper lobe (); cavities were noted in the lesion of the right lower lobe (); the lingual segment lesion of the left upper lobe presented signs of lobulation (); the margin of the left lower lobe was not slick, with obvious short burrs (); a halo sign was observed in the tumor periphery of the lesion (); vessel convergence was noted in the tumor periphery of the lesion of the right middle lobe (); bronchial transection was observed in the posterior segment lesion of the right upper lobe (); the surrounding bronchial vascular bundles of the right lower lobe lesion were thickened (); the adjacent pleura of the right upper lobe lesion showed indentation ().
Figure 1 The computed tomography morphological features of patients with stage I non-small cell lung cancer.
Survival analysis of stage I NSCLC patients with different TNM staging
As shown in , based on tumor diameter, patients with IA and IB stage were subdivided into T1a, T1b, T2a, and T2b stage. There were 37 cases of T1a, 44 cases of T1b, and 43 cases of T2a. No patients were T2b stage in this study. The 5-year survival rates of patients with T1a, T1b, and T2a stage were 89.19%, 75.00%, and 41.86%, respectively. There were significant differences in the 5-year survival rates among patients with different TNM staging (all P<0.05; ).
Figure 2 Survival curve of stage I non-small cell lung cancer patients with different tumor node metastasis stages.
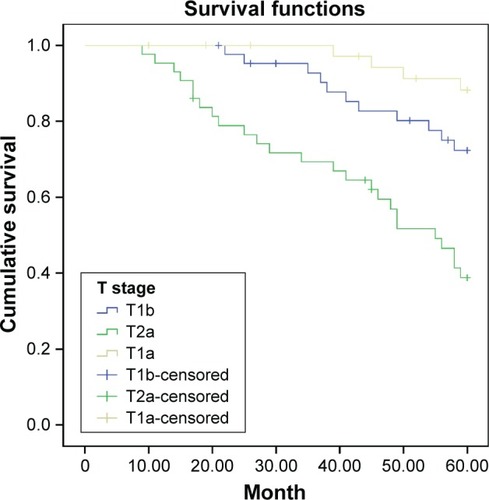
Table 1 The relationships of CT morphological features with 5-year survival rates of patients with stage I non-small cell lung cancer
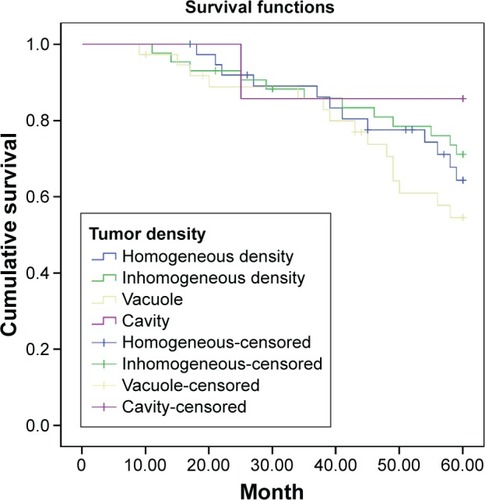
Survival analysis of stage I NSCLC patients with different CT features of tumor density
The CT morphological features of tumor density mainly included homogeneity, inhomogeneity, vacuole, and cavity. There were 38 cases of homogeneity, 43 cases of inhomogeneity, 37 cases of vacuole, and 6 cases of cavity. The 5-year survival rates of patients with homogeneity, inhomogeneity, vacuole, and cavity were 68.42%, 72.09%, 59.46%, and 83.33%, respectively. No differences in the 5-year survival rates were observed among patients with different CT features of tumor density (all P>0.05; ).
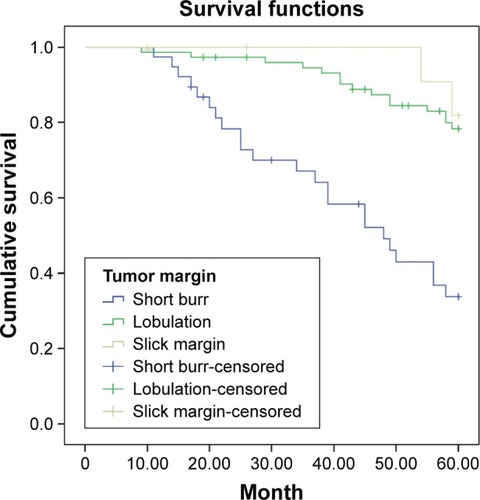
Survival analysis of stage I NSCLC patients with different CT features of tumor margin
The CT morphological features of tumor margin mainly included slick margin, lobulation sign, and short burr. There were 12 cases showing slick margin, 74 cases showing lobulation sign, and 38 cases showing short burr. The 5-year survival rates of patients with different margin features were 83.33% (slick margin), 79.73% (lobulation sign), and 39.47% (short burr). Significant differences were found in the 5-year survival rates among patients with different CT tumor margin features (P<0.05; ).
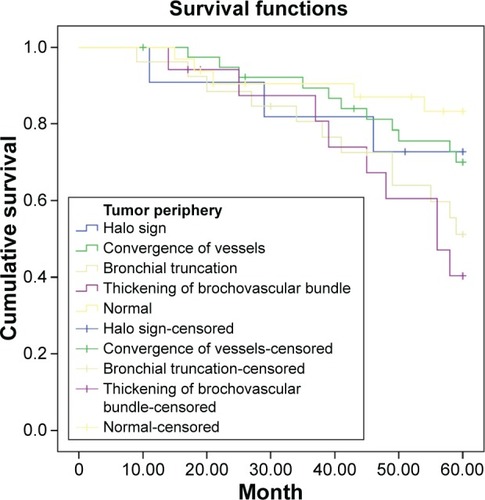
Survival analysis of stage I NSCLC patients with different CT tumor periphery features
The CT morphological features of tumor periphery mainly included normal, halo, vessel convergence, bronchial transection, and vascular bundle thickening. There were 32 cases of normal, 11 cases of halo, 39 cases of vessel convergence, 25 cases of bronchial transection, and 17 cases of vascular bundle thickening. The 5-year survival rates of patients with normal, halo, vessel convergence, bronchial transection, and vascular bundle thickening were 84.38%, 72.73%, 71.79%, 52.00%, and 47.06%, respectively. There were also significant differences in the 5-year survival rates among patients with different CT features of the tumor periphery (all P<0.05; ).
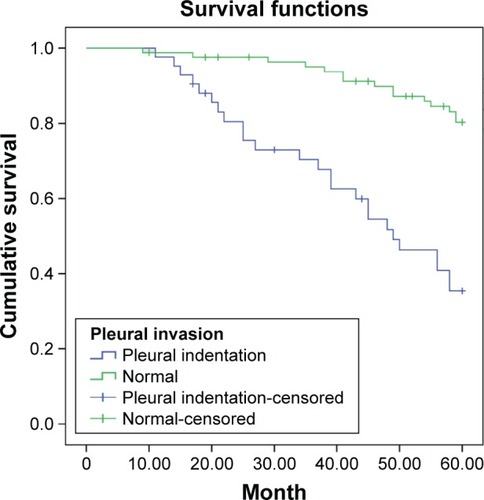
Survival analysis of stage I NSCLC patients with different CT features of pleural invasion
The CT morphological features of pleural invasion were normal or pleural thickening and indentation. There were 83 cases of normal and 41 cases of pleural thickening and indentation. The 5-year survival rates of patients with normal and pleural thickening/indentation were 81.93% and 39.02%, respectively. Significant differences were also observed among patients with different CT features of pleural invasion (all P<0.05; ).
Cox regression analysis of prognostic factors for stage I NSCLC
Cox regression analyses indicated that T2a stage (P=0.001, risk ratio [RR] =8.410, 95% confidence interval [CI] =2.261–31.283) and pleural thickening/indentation (P=0.034, RR =4.842, 95% CI =1.124–20.860) were prognostic factors of stage I NSCLC ().
Table 2 Cox regression analysis of prognostic factors for stage I non-small cell lung cancer
Discussion
With the rapid development of CT imaging, the value of CT morphological features of stage I NSCLC patients for predicting prognosis has raised concerns. In the present study, the 5-year survival rates of patients with stage I NSCLC was 67.74%. The 5-year survival rate of patients after the radical surgery is usually 60%–80%, consistent with the results of this study.Citation15 Furthermore, in our study, the 5-year survival rates of patients with T1a, T1b, and T2a stages were 89.19%, 75.00%, and 41.86%, respectively, with a significant decrease with increasing lesion diameter. The evolutionary theory of cancer suggests that smaller lesion diameter and volume are associated with earlier occurrence of lesion evolution or inhomogeneity and a lower rate of malignant change. Thus, the diameter and volume of tumors are directly related to patient prognosis.Citation16 Cox regression analysis indicated that patients in T2a and Ta1 stages of TNM staging also exhibited significantly different survival times. Tumor size is an independent factor for the prognosis of stage I NSCLC patients. Agarwal et al also demonstrated that tumor size is an important predictor of survival in surgically treated early-stage I NSCLC patients.Citation17
The CT morphological features of tumor density generally include homogeneity, inhomogeneity, vacuole, and cavity. Vacuole refers to transparent light with a diameter of <5 mm and relatively low density, which is very common in lung cancer. Recent evidence suggests that vacuole features on CT are of significance for distinguishing lung cancer from benign lesions.Citation18 Cavity formation occurs as diseased substances from lung necrosis and liquefaction are excreted through the bronchus. Air cavity formation has been associated with worse prognosis. Shi et al revealed that glitches and air cavity density are risk factors of malignancy, whereas calcification and satellite lesions are protective factors, based on CT findings of solitary pulmonary nodules. During the progression from small-to-large lesions, air cavity density is first detected in early stages, followed by glitches.Citation19 In our study, the 5-year survival rates of patients with homogeneity, inhomogeneity, vacuole, and cavity were 68.42%, 72.09%, 59.46%, and 83.33%, respectively. However, there were no differences among patients with different CT features of tumor density, most likely because our study included tumors that were small in size but had features of necrosis, calcification, vacuole, and cavity, and the inclusion of only six cases of cavity.
The CT features of tumor margin included slick margin, lobulation sign, or short burr, and these features were associated with 5-year survival rates of 83.33%, 79.73%, and 39.47%, respectively. Approximately 80% or more peripheral lung cancer cases will exhibit changes in lobulation when the CT dose is lowered, whereas the rate of change in lobulation is only 25% in benign lesions. Thus, changes in lobulation are significant for the diagnosis of malignant lesions. Lee et al reported that lobulation is associated with tumor size.Citation20 The occurrence rate of short burr in lung adenocarcinoma is high, with a rate of 81%–100% in typical lung cancer. Regression analysis found that TNM staging (T2a) and pleural thickening and indentation are key factors for the prognosis of stage I NSCLC patients. Shinohara et al found that short burr was significantly more frequent in malignant tumors than benign lesions.Citation21
The CT features of pleural invasion are normal and pleural indentation/thickening. The 5-year survival rates differed significantly and were 81.93% and 39.02%, respectively. The reported postoperative survival rate is only ~40% when a tumor without intrapulmonary and distant metastasis has impacted the visceral pleura. Currently, the treatment regime for stage I NSCLC patients is determined according to the extent of visceral pleural involvement, which is also a common prognostic indicator. The National Comprehensive Cancer Network criteria are commonly used to identify stage I NSCLC patients based on at least one of the following risk factors: vascular invasion, minimal margins, tumors >4 cm in diameter, and visceral pleural involvement.Citation22 Cox regression analysis also demonstrated that TNM staging and pleural invasion were independent prognostic factors for stage I NSCLC.
Conclusion
In conclusion, our study revealed that T2a stage and pleural thickening/indentation might be prognostic factors in stage I NSCLC. The results of this study will benefit further treatment and management of stage I NSCLC. Further prospective studies with a larger sample size are needed to validate our results.
Acknowledgments
We thank the reviewers for their helpful comments on this article.
Disclosure
The authors report no conflicts of interest in this work.
References
- SongGQinTLiuHQuantitative breath analysis of volatile organic compounds of lung cancer patientsLung Cancer201067222723119409642
- MolinaJRYangPCassiviSDSchildSEAdjeiAANon-small cell lung cancer: epidemiology, risk factors, treatment, and survivorshipMayo Clin Proc200883558459418452692
- MerrowCEWangIZPodgorsakMBA dosimetric evaluation of VMAT for the treatment of non-small cell lung cancerJ Appl Clin Med Phys2012141411023318374
- Dela CruzCSTanoueLTMatthayRALung cancer: epidemiology, etiology, and preventionClin Chest Med201132460564422054876
- EttingerDSWoodDEAkerleyWNon-small cell lung cancer, version 6. 2015J Natl Compr Canc Netw201513551552425964637
- TangSPanYWangYGenome-wide association study of survival in early-stage non-small cell lung cancerAnn Surg Oncol201522263063525145502
- XuYHLuSA meta-analysis of STAT3 and phospho-STAT3 expression and survival of patients with non-small-cell lung cancerEur J Surg Oncol201440331131724332948
- ChampionLBrainEGiraudetALBreast cancer recurrence diagnosis suspected on tumor marker rising: value of whole-body 18FDG-PET/CT imaging and impact on patient managementCancer201111781621162921472709
- BachPBJettJRPastorinoUTockmanMSSwensenSJBeggCBComputed tomography screening and lung cancer outcomesJAMA2007297995396117341709
- BachPBMirkinJNOliverTKBenefits and harms of CT screening for lung cancer: a systematic reviewJAMA2012307222418242922610500
- InfanteMCavutoSLutmanFRDANTE Study GroupA randomized study of lung cancer screening with spiral computed tomography: three-year results from the DANTE trialAm J Respir Crit Care Med2009180544545319520905
- WangXCaoAPengMThe value of chest CT scan and tumor markers detection in sputum for early diagnosis of peripheral lung cancerZhongguo Fei Ai Za Zhi200471586321211195
- StemberJNKoJPNaidichDPKaurMRusinekHThe self-overlap method for assessment of lung nodule morphology in chest CTJ Digit Imaging201326223924723065123
- Rami-PortaRCrowleyJJGoldstrawPThe revised TNM staging system for lung cancerAnn Thorac Cardiovasc Surg20091514919262443
- LagerwaardFJVerstegenNEHaasbeekCJOutcomes of stereotactic ablative radiotherapy in patients with potentially operable stage I non-small cell lung cancerInt J Radiat Oncol Biol Phys201283134835322104360
- ThompsonRHKurtaJMKaagMTumor size is associated with malignant potential in renal cell carcinoma casesJ Urol200918152033203619286217
- AgarwalMBrahmandayGChmielewskiGWWelshRJRavikrishnanKPAge, tumor size, type of surgery, and gender predict survival in early stage (stage I and II) non-small cell lung cancer after surgical resectionLung Cancer201068339840219762109
- XueXWangPXueQComparative study of solitary thin-walled cavity lung cancer with computed tomography and pathological findingsLung Cancer2012781455022784387
- ShiCZZhaoQLuoLPHeJXSize of solitary pulmonary nodule was the risk factor of malignancyJ Thorac Dis20146666867624976989
- LeeJWGooJMLeeHJThe potential contribution of a computer-aided detection system for lung nodule detection in multidetector row computed tomographyInvest Radiol2004391164965515486524
- ShinoharaSHanagiriTTakenakaMEvaluation of undiagnosed solitary lung nodules according to the probability of malignancy in the American College of Chest Physicians (ACCP) evidence-based clinical practice guidelinesRadiol Oncol2014481505524587779
- KratzJRHeJVan Den EedenSKA practical molecular assay to predict survival in resected non-squamous, non-small-cell lung cancer: development and international validation studiesLancet2012379981882383222285053