Abstract
Background
We performed an analysis to clarify differences in clinicopathological and molecular features of lung invasive mucinous adenocarcinoma (IMA) based on computed tomography (CT) findings and their impact on prognosis.
Patients and methods
On the basis of CT findings, we divided lung IMA into three subtypes: solid, bubbling, and pneumonic. We then investigated differences in clinicopathological characteristics, prognosis, and the expressions of well-identified biomarkers, including cyclooxygenase-2 (Cox-2), excision repair cross-complementation group 1 (ERCC1), ribonucleotide reductase M1 (RRM1), class III beta-tubulin, thymidylate synthase (TS), secreted protein acidic and rich in cysteine (SPARC), programmed cell death-1 ligand-1 (PD-L1), and epidermal growth factor receptor mutation, among the three subtypes.
Results
A total of 29 patients with resected lung IMA were analyzed. Compared with the solid or bubbling type, the pneumonic type had a higher proportion of symptoms, a larger tumor size, a higher pathological stage, and a significantly worse prognosis. The immunohistochemical findings tended to show high expression of RRM1, class III beta-tubulin, and Cox-2 in the tumor and of SPARC in the stroma, but not of ERCC1, TS, and PD-L1 in the tumor. None of the biomarkers with high expression levels in the tumor were prognostic biomarkers, but the expression of SPARC in the stroma was correlated with a poor outcome.
Conclusion
Clinical and pathological features, in conjunction with molecular data, indicate that IMA should be divided into different subgroups. In our results, the pneumonic type was correlated with a significantly worse outcome. Further studies should be performed to confirm our conclusion and to explore its molecular implications.
Introduction
Lung cancer is a major cause of death in many developed countries. Surgical resection is the most important curative treatment option for this disease, especially early-stage non-small cell lung cancer (NSCLC). However, the 5-year survival rate of surgically treated NSCLC patients remains at ~70%.Citation1,Citation2 Several biomarkers have now been reported as predictors of survival and recurrence in patients with NSCLC.
The most common pathological subtype of NSCLC is adenocarcinoma, the prevalence of which has been increasing. A new classification for lung adenocarcinoma was proposed by an international multidisciplinary expert panel of the International Association for the Study of Lung Cancer/American Thoracic Society/European Respiratory Society (IASLC/ATS/ERS) in 2011.Citation3 Invasive mucinous adenocarcinoma (IMA) was recognized as a separate subtype of lung adenocarcinoma, whereas the definition of mucinous bronchioloalveolar carcinoma (BAC) is no longer used. IMA was supposed to contain components of columnar or goblet cells with abundant intracellular or extracellular mucus admixed with invasive adenocarcinoma patterns with stromal invasion. Compared with other lung adenocarcinoma subtypes, IMA has different immunohistochemical and molecular features.Citation4–Citation6 IMA also has a different progress pattern, compared with other subtypes of adenocarcinoma. In IMA, lymph node and distant metastasis are much less common than in other subtypes of adenocarcinoma. However, pulmonary metastasis frequently occurs in patients with IMA.Citation7
Two recent studies have discussed subtypes of IMA according to computed tomography (CT) findings; reportedly, these subtypes are closely related to the clinical outcomes of IMA patients.Citation8,Citation9 However, sufficient evidence of optimal management based on IMA subtypes does not yet exist. Here, we report a retrospective study examining surgically resected lung IMA with the aim of clarifying differences in clinicopathological and immunohistochemical features among IMA subtypes based on CT findings. In addition, we examined the optimal management of IMA based on a biomarker analysis.
Methods
Patients and specimens
From October 2005 to September 2014, a total of 605 patients with primary lung cancer underwent surgical resection at our hospital. Of these 605 patients, 29 patients (4.8%) presented with primary lung IMA. All the patients included in the present analysis met the following criteria: 1) curative resection and 2) neither radiotherapy nor chemotherapy administered prior to surgery. Written informed consent was obtained from each patient for the study of excised tissue samples from the surgical specimens. This study was conducted with the approval of the institutional Ethics Committee of Kawasaki Medical School (number 2159: approved on August 10, 2015).
Evaluation of CT findings
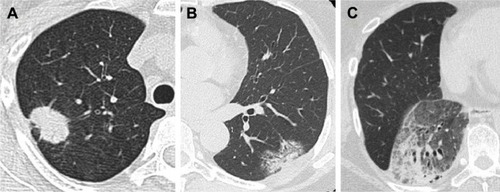
We classified the IMAs into three types based on the high-resolution CT (HRCT) findings as follows: 1) solid type, in which the shadows represented solitary nodules or masses; 2) bubbling type, in which the shadows represented bubbling shadow; and 3) pneumonic type, in which the shadows represented consolidations with or without air bronchograms ().Citation8
Immunohistochemical analysis
Immunohistochemical analyses of resected, paraffin-embedded lung cancer tissues were performed. After microtome sectioning (4 μm), the slides were processed for staining using an automated immunostainer (Nexes; Ventana, Tucson, AZ, USA). The streptavidin–biotin–peroxidase detection technique using diaminobenzidine as the chromogen was applied. The primary antibodies were used according to the manufacturer’s instructions. The antibodies that were used are summarized in .Citation10–Citation15 The slides were examined by two investigators who had no knowledge of the corresponding clinicopathological data. The expression of each marker protein was examined and evaluated according to the original protocol, as reported previously.
Nuclear staining for thyroid transcription factor-1 (TTF-1) and excision repair cross-complementation group 1 (ERCC1) and cell membrane or cytoplasmic staining for cyclooxygenase-2 (Cox-2), cytokeratin 7 (CK7), CK20, ribonucleotide reductase M1 (RRM1), thymidylate synthase (TS), class III beta-tubulin, secreted protein acidic and rich in cysteine (SPARC), and programmed cell death-1 ligand-1 (PD-L1) were assessed (Figure S1).
Immunoreactivity was evaluated semiquantitatively based on the intensity and estimated percentage of tumor cells that were stained. Intensity was quantified as follows: 1+, weak staining (detection required high magnification); 2+, moderate staining (readily detected at medium magnification); and 3+, strong staining (readily detected at low magnification). H (histologic)-scores were derived by multiplying the percentage of immunoreactive cells (0–100) by the intensity score (0, 1+, 2+, and 3+), yielding a number between 0 and 300. SPARC staining was also evaluated using the H-score and was scored for two separate compartments: peritumoral stromal SPARC in fibroblasts and tumor epithelial SPARC. If the H-score exceeded the mean value, the test result was considered to be positive for that marker.
EGFR mutation analysis
An analysis to detect epidermal growth factor receptor (EGFR) mutations was performed using resected, paraffin-embedded lung cancer tissues and the peptide nucleic acid-locked nucleic acid (PNA-LNA) polymerase chain reaction (PCR) clamp method.Citation16 The PNA-LNA PCR clamp assay was performed at Mitsubishi Kagaku Bio-clinical Laboratories, Inc, Tokyo, Japan.
Statistical analyses
All the statistical analyses were performed using the SPSS statistical package (version 22.0; SPSS, Chicago, IL, USA). Categorical data were examined using the χ2 test. The prognostic evaluation was performed by considering the recurrence-free survival (RFS), which was defined as the time until lung cancer recurrence or nonlung cancer-related death. The survival curves were estimated using the Kaplan–Meier method. Two-sided P-values of <0.05 were considered statistically significant.
Results
Relationship between the clinical and HRCT findings of IMA
shows the clinical characteristics of the patients according to the IMA subtypes based on HRCT findings. Among the clinical findings, the pneumonic type was associated with a higher proportion of symptoms (P=0.004) and a large tumor size (P=0.001). The bubbling type was associated with a lower maximal standardized uptake value (SUVmax) on fluorodeoxyglucose–positron emission tomography (P=0.002).
Table 1 Clinical characteristics of patients based on computed tomography findings
Relationship between pathological and HRCT findings of IMA
Among the pathological findings, no statistically significant associations were observed between lymph node metastasis, lymphatic invasion, vascular invasion, or pleural involvement and the HRCT findings among the subtypes (). However, the pneumonic type was associated with a higher pathological stage because of its relatively large tumor size (P=0.017). As many previous reports have indicated, the expression of TTF-1 was low and the expressions of CK7 and 20 were high for all subtypes.Citation11 EGFR mutation was positive in only 13.8% (4/29) cases.
Table 2 Pathological characteristics of patients based on computed tomography findings
Surgical procedure and prognosis
All patients with pneumonic type received standard lobectomy. Five patients with solid or bubbling type received wedge resection, who were considered at increased risk for standard resection because of poor physiologic respiratory reserve. Nine patients received adjuvant chemotherapy, who were pathologically diagnosed with large tumor size (>4 cm) or lymph node metastasis.
Seven (24.1%) patients developed cancer recurrence after resection. A significant association between pneumonic-type IMA and a high rate of recurrence (60.0% vs 10.0% for solid type and 0% for bubbling type, P=0.004) was observed. The initial recurrence sites are shown in . All the initial recurrences were intrathoracic metastases, such as lung metastasis, pleural dissemination, and mediastinal lymph node metastasis. No cases of extrathoracic metastasis of IMA occurred in this series.
Table 3 Prognosis of patients based on computed tomography findings
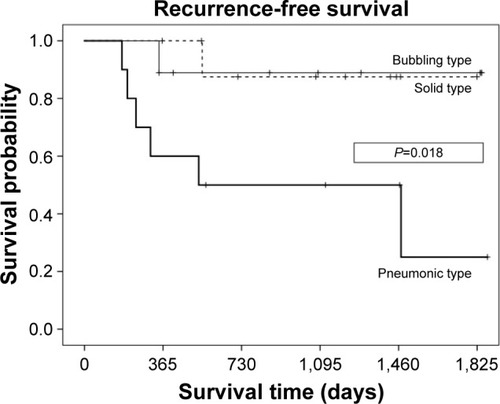
The median follow-up time was 980 days. The 5-year RFS rate was 87.5% for solid type, 88.9% for bubbling type, and 25.0% for pneumonic type. Compared with the solid or bubbling types, the pneumonic type had a significantly poorer RFS (P=0.018) ().
Biomarker analysis
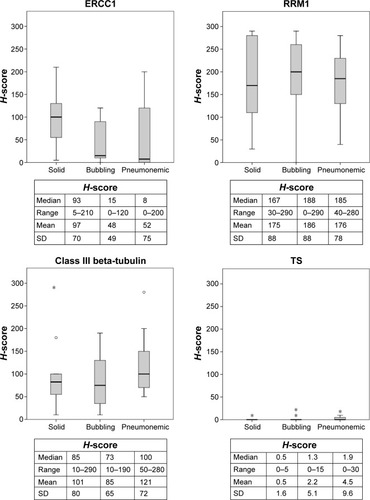
For the immunohistochemical analysis, the H-score for each marker expression profile was shown according to the subtypes based on the CT findings (). In an overall analysis, the H-score of the markers were as follows: ERCC1, 66.2±67.6; RRM1, 178.8±81.5; class III beta-tubulin, 103.1±71.7; TS, 2.4±6.4; SPARC in tumor tissues, 32.4±34.6; SPARC in stroma, 126.0±65.2; PD-L1, 2.0±3.5; and Cox-2, 170.5±68.6. The expressions of RRM1, class III beta-tubulin, Cox-2 in tumor, and SPARC in stroma were relatively high in all the IMA subtypes, whereas those of ERCC1, TS, and PD-L1 were relatively low. Of these, only the H-score of SPARC in stroma was significantly higher in the pneumonic type than in the solid (P=0.029) or bubbling type (P=0.048).
Figure 3 The immunohistochemical H-score for each marker expression profile based on the computed tomography findings.
Abbreviations: Cox-2, cyclooxygenase-2; ERCC1, excision repair cross-complementation group 1; H-score, histologic score; PD-L1, programmed cell death-1 ligand-1; RRM1, ribonucleotide reductase M1; SD, standard deviation; SPARC, secreted protein acidic and rich in cysteine; TS, thymidylate synthase.
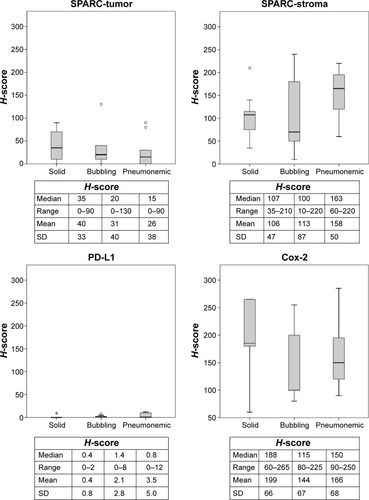
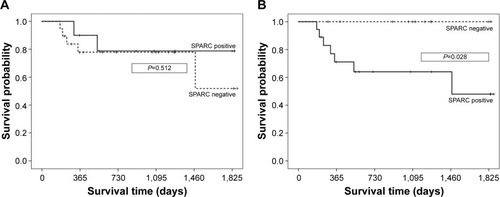
As to the RFS, none of the biomarkers were prognostic factors. However, the RFS of patients with positive SPARC expression in stroma tissue was significantly poorer than that of patients with negative SPARC expression in stroma tissue (P=0.028; ).
Discussion
We undertook this study to investigate whether it is reasonable to divide IMA into separate subtypes. To our knowledge, this is the first study to focus on the differences in prognosis and molecular alterations in IMA subgroups with different morphological features. Since the appearance of the IASLC/ATS/ERS classification for lung adenocarcinoma in 2011, many studies have focused on the influence of the pathological subtype on prognosis and molecular changes.Citation17–Citation19 IMAs, which account for 2%–10% of lung adenocarcinoma cases in East Asia, Europe, and the US, were considered to be more malignant than other common subtypes of lung adenocarcinoma, such as lepidic and acinar subtypes.Citation19–Citation22 Nonmucinous adenocarcinomas originate from type-II pneumocystis or Clara cells, whereas IMAs most likely originate from bronchiolar lining cells that have undergone mucinous (goblet cell) metaplasia. IMAs show a strong tendency for multicentric, multilobar, and bilateral lung involvement, which may reflect aerogenous spread.Citation11 IMA is also strongly correlated (76%) with KRAS mutation and almost entirely lacks EGFR mutations, whereas nonmucinous adenocarcinoma in situ/minimally invasive adenocarcinoma/lepidic predominant adenocarcinoma exhibit the opposite trends with 45% of cases positive for EGFR mutation but only 13% positive for KRAS mutation.Citation23
Generally, mucinous adenocarcinomas in other organs are also associated with lymph node metastasis and a poor prognosis.Citation24–Citation26 The reason is that the mucus is considered to play a critical role in the development of cancer.Citation27 In this study, the prognosis of resected IMA of the lung was relatively good, because lung IMA was not associated with lymph node metastasis. However, patients with pneumonic type had a poorer prognosis than those with other types. This subtype was also observed to have a higher rate of intrathoracic metastasis and was associated with a poor prognosis.
Recently, both experimental and clinical studies have revealed that many molecules contribute to various biological behaviors of malignant tumors, including NSCLC. New strategies based on a better understanding of tumor biology are, thus, needed to maximize the efficacy of current treatments. The associations between these strategies and the response to chemotherapy have been investigated, and the selection of effective chemotherapy regimens based on the evaluation of these biomarkers may improve the clinical outcome of NSCLC patients. Platinum-based chemotherapy remains the scaffold upon which combination chemotherapy regimens are assembled for NSCLC patients. As a predictor of the efficacy of platinum-based chemotherapy, the intratumoral expression of ERCC1, a major component of the nucleotide excision repair pathway, is reported to be associated with a lower responsiveness of patients to cisplatin.Citation28,Citation29 In addition, the intratumoral expression of class III beta-tubulin is likely to be associated with a lower responsiveness to taxanes, such as paclitaxel and docetaxel.Citation30,Citation31 Moreover, RRM1 is likely to be associated with a lower responsiveness to gemcitabine.Citation32 The expression of TS protein was associated with a reduced sensitivity of patients to pemetrexed treatment.Citation33,Citation34 Our results showed that the expressions of RRM1 and class III beta-tubulin were relatively high, whereas those of ERCC1 and TS were relatively low in IMA. Thus, we suspect that IMA might be susceptible to cisplatin or pemetrexed, but not to gemcitabine or taxans.
SPARC plays remarkable roles in altering the activity and the microenvironment of cancer cells, modulating cell growth, apoptosis, adhesion, migration, and invasion in human carcinogenesis.Citation35,Citation36 Thus, many studies have evaluated the effect of SPARC expression in many cancers. SPARC has generated remarkable interest as a potential molecular marker of prognosis for malignant tumors. However, whether a high or low, SPARC expression level is correlated with a poor survival outcome remains controversial. In pancreatic cancer, Han et al reported that high SPARC expression in the stroma, but not in the tumor, was a strong predictor of a shorter survival period.Citation37 Compared with its expression in tumor cells, the overexpression of SPARC is frequently found in the stroma in pancreatic cancer.Citation38 In the present results, the level of SPARC expression in the stroma was relatively high and seemed to be similar to that in pancreatic cancer. SPARC was considered to be a predictive biomarker of response to nab-paclitaxel in three different clinical trials for melanoma, pancreatic, and breast cancer.Citation39 Our present results showing a high level of SPARC expression in the stroma suggest that IMA, especially pneumonic type, might be susceptible to nab-paclitaxel.
In 2015, nivolumab, a new immunotherapy drug, was approved by the Food and Drug Administration for the treatment of lung cancer after the termination of standard chemotherapy.Citation15,Citation40 Especially in nonsquamous NSCLC, nivolumab was associated with greater efficacy in subgroups defined according to prespecified levels of PD-L1. However, our results suggested that IMA might not be susceptible to nivolumab because the IMA specimens had low PD-L1 expression levels.Citation15
In this study, the H-score for Cox-2 tended to be high in tumor cells. In 2008, Edelman et al reported that Cox-2 expression was a significant prognostic factor in patients with advanced NSCLC (Cancer and Leukemia Group B Trial 30203). Moreover, patients with moderate to high levels of Cox-2 expression had a better tumor response to a Cox-2 inhibitor (celecoxib) in terms of a longer median survival period compared with those not receiving celecoxib.Citation10
Limitations
The present study had several limitations. The clinical outcomes were of limited significance because some of the patients had different postoperative treatments. Meanwhile, a sample size of 29 patients is too small to confirm differences among IMA subgroups with different morphological features. The present findings need to be validated by further research with larger samples.
Conclusion
We found three subtypes of lung IMAs based on CT findings. This study represents the first comparison of clinical features and biomarker expressions in IMAs. Clinical and pathological features in conjunction with molecular data indicate that IMA should be divided into different subgroups. Further studies should be performed to confirm our conclusions and to explore the underlying molecular functions.
Acknowledgments
This work was supported, in part, by a Research Project Grant (number 26–64) from Kawasaki Medical School. The authors thank Kiyomi Maitani for providing technical assistance and IMIC for the English language review.
Supplementary materials
Figure S1 Representative photomicrographs of biomarker expression.
Notes: Magnification ×200. (A) ERCC1; nuclear staining, mean H-score: 66, negative case score: 0, positive case score: 190. (B) RRM1; cytoplasmic staining, mean H-score: 178, negative case score: 0, positive case score: 260. (C) TS; cytoplasmic staining, mean H-score: 2.4, negative case score: 0, positive case score: 30. (D) Class III beta-tubulin, cytoplasmic staining, mean H-score: 126, negative case score: 10, positive case score: 280. (E) PD-L1, membrane staining, mean H-score: 4.8, negative case score: 0, positive case score: 50. (F) Cox-2; cytoplasmic staining, mean H-score: 181, negative case score: 60, positive case score: 270. (G) SPARC in tumor tissue; cytoplasmic staining, mean H-score: 32, negative case score: 0, positive case score: 90. (H) SPARC in stroma tissue; cytoplasmic staining, mean H-score:122, negative case score: 10, positive case score: 240.
Abbreviations: Cox-2, cyclooxygenase-2; ERCC1, excision repair cross-complementation group 1; H-score, histologic score; PD-L1, programmed cell death-1 ligand-1; RRM1, ribonucleotide reductase M1; SPARC, secreted protein acidic and rich in cysteine; TS, thymidylate synthase.
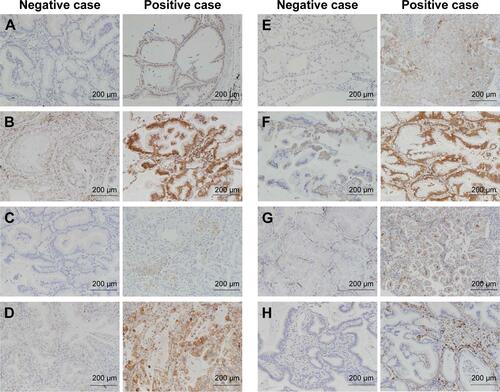
Table S1 Antibodies and conditions
References
- EdelmanMJWatsonDWangXEicosanoid modulation in advanced lung cancer: cyclooxygenase-2 expression is a positive predictive factor for celecoxib + chemotherapy–Cancer and Leukemia Group B Trial 30203J Clin Oncol200826684885518281656
- SimsirAWeiXJYeeHMoreiraACangiarellaJDifferential expression of cytokeratins 7 and 20 and thyroid transcription factor-1 in bronchioloalveolar carcinoma: an immunohistochemical study in fine-needle aspiration biopsy specimensAm J Clin Pathol2004121335035715023039
- HeYWZhaoMLYangXYZengJDengQHHeJXPrognostic value of ERCC1, RRM1, and TS proteins in patients with resected non-small cell lung cancerCancer Chemother Pharmacol201575486186725732635
- SèvePLaiRDingKClass III beta-tubulin expression and benefit from adjuvant cisplatin/vinorelbine chemotherapy in operable non-small cell lung cancer: analysis of NCIC JBR.10Clin Cancer Res200713399499917289895
- HidalgoMPlazaCMusteanuMSPARC Expression Did Not Predict Efficacy of nab-Paclitaxel plus Gemcitabine or Gemcitabine Alone for Metastatic Pancreatic Cancer in an Exploratory Analysis of the Phase III MPACT TrialClin Cancer Res201521214811481826169969
- BorghaeiHPaz-AresLHornLNivolumab versus docetaxel in advanced nonsquamous non-small-cell lung cancerN Engl J Med2015373171627163926412456
Disclosure
The authors report no conflicts of interest in this work.
References
- AsamuraHGoyaTKoshiishiYA Japanese lung cancer registry study: prognosis of 13,010 resected lung cancersJ Thorac Oncol200831465218166840
- SawabataNMiyaokaEAsamuraHJapanese lung cancer registry study of 11,663 surgical cases in 2004: demographic and prognosis changes over decadeJ Thorac Oncol2011671229123521610521
- TravisWDBrambillaENoguchiMInternational Association for the Study of Lung Cancer/American Thoracic Society/European Respiratory Society international multidisciplinary classification of lung adenocarcinomaJ Thorac Oncol20116224428521252716
- ZhangYSunYXiangJZhangYHuHChenHA clinicopathologic prediction model for postoperative recurrence in stage Ia non-small cell lung cancerJ Thorac Cardiovasc Surg201414841193119924667022
- CasaliCRossiGMarchioniAA single institution-based retrospective study of surgically treated bronchioloalveolar adenocarcinoma of the lung: clinicopathologic analysis, molecular features, and possible pitfalls in routine practiceJ Thorac Oncol20105683083620521350
- GoldsteinNSThomasMMucinous and nonmucinous bronchioloalveolar adenocarcinomas have distinct staining patterns with thyroid transcription factor and cytokeratin 20 antibodiesAm J Clin Pathol2001116331932511554157
- WislezMAntoineMBaudrinLNon-mucinous and mucinous subtypes of adenocarcinoma with bronchioloalveolar carcinoma features differ by biomarker expression and in the response to gefitinibLung Cancer201068218519119581016
- WatanabeHSaitoHYokoseTRelation between thin-section computed tomography and clinical findings of mucinous adenocarcinomaAnn Thorac Surg201599397598125624054
- LeeHYLeeKSHanJMucinous versus nonmucinous solitary pulmonary nodular bronchioloalveolar carcinoma: CT and FDG PET findings and pathologic comparisonsLung Cancer200965217017519111932
- EdelmanMJWatsonDWangXEicosanoid modulation in advanced lung cancer: cyclooxygenase-2 expression is a positive predictive factor for celecoxib + chemotherapy–Cancer and Leukemia Group B Trial 30203J Clin Oncol200826684885518281656
- SimsirAWeiXJYeeHMoreiraACangiarellaJDifferential expression of cytokeratins 7 and 20 and thyroid transcription factor-1 in bronchioloalveolar carcinoma: an immunohistochemical study in fine-needle aspiration biopsy specimensAm J Clin Pathol2004121335035715023039
- HeYWZhaoMLYangXYZengJDengQHHeJXPrognostic value of ERCC1, RRM1, and TS proteins in patients with resected non-small cell lung cancerCancer Chemother Pharmacol201575486186725732635
- SèvePLaiRDingKClass III beta-tubulin expression and benefit from adjuvant cisplatin/vinorelbine chemotherapy in operable non-small cell lung cancer: analysis of NCIC JBR.10Clin Cancer Res200713399499917289895
- HidalgoMPlazaCMusteanuMSPARC Expression Did Not Predict Efficacy of nab-Paclitaxel plus Gemcitabine or Gemcitabine Alone for Metastatic Pancreatic Cancer in an Exploratory Analysis of the Phase III MPACT TrialClin Cancer Res201521214811481826169969
- BorghaeiHPaz-AresLHornLNivolumab versus docetaxel in advanced nonsquamous non-small-cell lung cancerN Engl J Med2015373171627163926412456
- NagaiYMiyazawaHHuqunGenetic heterogeneity of the epidermal growth factor receptor in non-small cell lung cancer cell lines revealed by a rapid and sensitive detection system, the peptide nucleic acid-locked nucleic acid PCR clampCancer Res200565167276728216105816
- HungJJJengWJChouTYPrognostic value of the new international association for the study of lung cancer/American thoracic society/European respiratory society lung adenocarcinoma classification on death and recurrence in completely resected stage I lung adenocarcinomaAnn Surg201325861079108623532112
- RussellPABarnettSAWalkiewiczMCorrelation of mutation status and survival with predominant histologic subtype according to the new IASLC/ATS/ERS lung adenocarcinoma classification in stage III (N2) patientsJ Thorac Oncol20138446146823486266
- WarthAMuleyTMeisterMThe novel histologic International Association for the Study of Lung Cancer/American Thoracic Society/European respiratory society classification system of lung adenocarcinoma is a stage-independent predictor of survivalJ Clin Oncol201230131438144622393100
- TsutaKKawagoMInoueEThe utility of the proposed IASLC/ATS/ERS lung adenocarcinoma subtypes for disease prognosis and correlation of driver gene alterationsLung Cancer201381337137623891509
- YoshizawaAMotoiNRielyGJImpact of proposed IASLC/ATS/ERS classification of lung adenocarcinoma: prognostic subgroups and implications for further revision of staging based on analysis of 514 stage I casesMod Pathol201124565366421252858
- CadranelJQuoixEBaudrinLIFCT-0401 Trial Group IFCT-0401 Trial: a phase II study of gefitinib administered as first-line treatment in advanced adenocarcinoma with bronchioloalveolar carcinoma subtypeJ Thorac Oncol2009491126113519574932
- TangERSchreinerAMPuaBBAdvances in lung adenocarcinoma classification: a summary of the new international multidisciplinary classification system (IASLC/ATS/ERS)J Thorac Dis20146Suppl 5S489S50125349701
- ConsortiFLorenzottiAMidiriGDi PaolaMPrognostic significance of mucinous carcinoma of colon and rectum: a prospective case-control studyJ Surg Oncol2000732707410694641
- EnciuMAşchieMDeacuMPoinăreanuIMorphological characteristics of a mucinous adenocarcinoma of the prostate: differential diagnosis considerationsRom J Morphol Embryol201354119119423529329
- KunisakiCAkiyamaHNomuraMClinicopathologic characteristics and surgical outcomes of mucinous gastric carcinomaAnn Surg Oncol200613683684216604474
- BeattyPLNarayananSGariépyJRanganathanSFinnOJVaccine against MUC1 antigen expressed in inflammatory bowel disease and cancer lessens colonic inflammation and prevents progression to colitis-associated colon cancerCancer Prev Res (Phila)20103443844620332301
- LordRVBrabenderJGandaraDLow ERCC1 expression correlates with prolonged survival after cisplatin plus gemcitabine chemotherapy in non-small cell lung cancerClin Cancer Res2002872286229112114432
- OlaussenKADunantAFouretPDNA repair by ERCC1 in non-small cell lung cancer and cisplatin-based adjuvant chemotherapyN Engl J Med20063551098399116957145
- SevePMackeyJIsaacSClass III β-tubulin expression in tumor cells predicts response and outcome in patients with non-small cell lung cancer receiving paclitaxelMol Cancer Ther20054122001200716373715
- ReimanTLaiRVeillardASCross-validation study of class III beta-tubulin as a predictive marker for benefit from adjuvant chemotherapy in resected non-small-cell lung cancer: analysis of four randomized trialsAnn Oncol2012231869321471564
- BeplerGWilliamsCSchellMJRandomized international phase III trial of ERCC1 and RRM1 expression-based chemotherapy versus gemcitabine/carboplatin in advanced non-small-cell lung cancerJ Clin Oncol201331192404241223690416
- NicolsonMCFennellDAFerryDThymidylate synthase expression and outcome of patients receiving pemetrexed for advanced nonsquamous non-small-cell lung cancer in a prospective blinded assessment phase II clinical trialJ Thorac Oncol20138793093923722170
- ShimizuTNakanishiYNakagawaYAssociation between expression of thymidylate synthase, dihydrofolate reductase, and glycinamide ribonucleotide formyltransferase and efficacy of pemetrexed in advanced non-small cell lung cancerAnticancer Res201232104589459623060591
- BradshawADDiverse biological functions of the SPARC family of proteinsInt J Biochem Cell Biol201244348048822249026
- NagarajuGPDontulaREl-RayesBFLakkaSSMolecular mechanisms underlying the divergent roles of SPARC in human carcinogenesisCarcinogenesis201435596797324675529
- HanWCaoFChenMBPrognostic value of SPARC in patients with pancreatic cancer: a systematic review and meta-analysisPLoS One201611e014580326731428
- SatoNFukushimaNMaeharaNSPARC/osteonectin is a frequent target for aberrant methylation in pancreatic adenocarcinoma and a mediator of tumor-stromal interactionsOncogene2003225021503012902985
- DesaiNTrieuVKnauerDSPARC may be a predictive biomarker of response to nab-paclitaxelEur J Cancer200972388
- BrahmerJReckampKLBaasPNivolumab versus docetaxel in advanced squamous-cell non-small-cell lung cancerN Engl J Med2015373212313526028407